In the Literature
Henke CS, Beal MW, Walton RAL, et al. Retrospective evaluation of the clinical course and outcome of zinc toxicosis due to metallic foreign bodies in dogs (2005-2021): 55 cases. J Vet Emerg Crit Care (San Antonio). 2023;33(6):676-684. doi:10.1111/vec.13330
The Research …
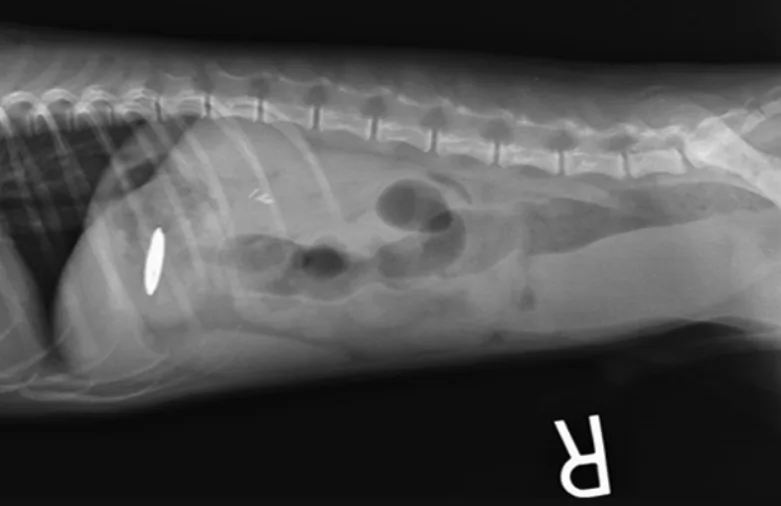
Zinc toxicosis can occur following ingestion of metallic foreign bodies (MFBs) that contain zinc, most commonly US pennies minted after 1982. Zinc ions and zinc salts are rapidly released from MFBs in the acidic environment of the stomach. The mechanism of toxicity is largely unknown but proposed to be due to oxidative damage resulting in hemolysis.1 MFB removal and supportive care are critical to recovery from zinc toxicosis.2
This retrospective study described the clinical course and outcome of 55 dogs with zinc toxicosis at veterinary teaching hospitals in the United States. Clinical signs at presentation included lethargy, vomiting, inappetence, diarrhea, pigmenturia, and pale mucous membranes. Median patient age was 2 years (range, ≈9 weeks-14 years), and median weight was 12.6 lb (5.7 kg; range, 2.1-112.4 lb [0.95-51 kg]).
MFBs were removed via endoscopy (72.8%), laparotomy (10.9%), spontaneous or induced emesis (10.9%), or gastric lavage (1.8%) or were spontaneously passed or manually removed from the rectum (3.6%). Median time to stabilization of hematocrit after MFB removal was 24 hours in 30 of 36 dogs.
In dogs for which data were available, the most common sequelae included anemia (47 of 54 dogs), acute liver injury (41 of 50 dogs), coagulopathy (10 of 14 dogs), thrombocytopenia (16 of 45 dogs), acute kidney injury (14 of 52 dogs), and acute pancreatitis (3 of 55 dogs).
Supportive care commonly included IV or SC fluids, gastroprotectants, antiemetics, antioxidants, and blood products. Three patients received chelation therapy with edetate calcium disodium, one of which developed anuric renal failure. Of all dogs, 45 survived, 3 died, and 7 were euthanized.
… The Takeaways
Key pearls to put into practice:
Zinc toxicosis is uncommon but should be considered in dogs with anemia and lethargy, especially with concurrent GI signs. Abdominal radiography and a thorough patient history (including vomiting of metal objects and ingestion of MFBs) should be performed rapidly.
Rapid MFB removal is key. Most dogs recover quickly after removal with supportive care.
Although the survival rate was 81% in this study, pet owners should be educated about the potential for poor outcomes and cost of treatment. In this study, 92.7% of dogs required hospitalization for a median of 3 days (range, 0-17 days).
Acute kidney injury and acute pancreatitis secondary to zinc toxicosis may be more common than previously suspected and should be monitored for closely. In this study, 2 of 3 dogs with acute pancreatitis were euthanized.
Chelation for zinc toxicosis is controversial, as these patients typically improve rapidly after removal of the MFB.1 Chelation should be considered on a case-by-case basis, as edetate calcium disodium can cause acute kidney injury. One patient that was chelated in this study developed anuric renal failure and was euthanized.
You are reading 2-Minute Takeaways, a research summary resource presented by Clinician’s Brief. Clinician’s Brief does not conduct primary research.