The Veterinary Significance of Emerging Infectious Diseases
J. Scott Weese, DVM, DVSc, DACVIM, FCAHS, University of Guelph, Ontario, Canada
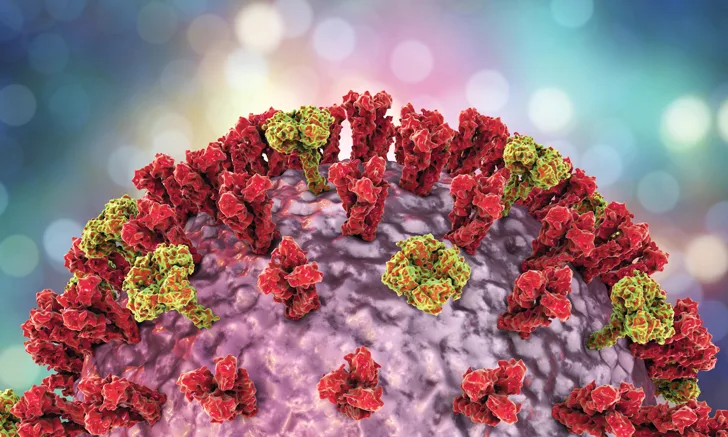
Emerging infectious diseases pose a significant threat to humans and animals but are inherently unpredictable. Although historical trends and disease patterns can provide insight, determining which diseases are likely to emerge and the impact they will have on human and animal populations is an educated guess at best. Of additional concern is the estimate that 60% to 80% of emerging diseases are zoonotic,1 which emphasizes the importance of veterinarians in the identification, prevention, and control of emerging infectious diseases.
An ecosystem approach to health considers disease occurrence to be at the intersection of the microbial agent, the host (human or animal), and the environment.1 Any alterations in the agent, host, or environment can alter the risk for disease. Thus, new infectious disease threats can emerge from a variety of sources.
Emergence of New Pathogens
Emergence of new pathogens is uncommon but continues to occur. If highly transmissible, new pathogens can have profound effects, as the worldwide population would be immunologically naïve to the emerging pathogen. For example, the emergence of canine parvovirus in the 1970s2 became a worldwide epidemic, with rapid international transmission and high morbidity and mortality rates.
Canine influenza is a more recent example of the threats posed by emerging pathogens. The emergence of equine-origin canine influenza H3N8 in the United States in the early 2000s3 demonstrated the potential impact of antigenic shift of influenza on the canine population. The more recent emergence of avian-origin canine influenza H3N2 caused—and continues to cause—widespread illness and disruption in parts of Asia, the United States, and Canada.4,5
Change in Existing Pathogens
Alterations in existing pathogens can impact a pathogen’s virulence (eg, acquisition of new virulence factors) and the ability to treat (eg, acquisition of antimicrobial-resistant genes or antiviral resistance) or prevent disease (eg, alterations in vaccine efficacy, resistance to heartworm prophylaxis). The worldwide epidemic of antimicrobial resistance, particularly methicillin-resistant staphylococci6 and extended-spectrum β-lactamase production in gram-negative bacteria, has had tremendous impacts on human and animal populations.7 Multidrug-resistant pathogens cause large numbers of infections every year and can be associated with higher morbidity and mortality rates; the need for more expensive, toxic, or cumbersome treatments; and the risk for transmission to other humans or animals. Economic impacts are similarly profound; the World Bank has estimated that by 2050 the global burden of antimicrobial resistance could surpass that of the 2008 financial crisis.8 New resistance mechanisms, including resistance to “last-resort” drugs such as colistin,9 continue to be identified and will continue to pose a problem to the veterinary profession as bacterial evolution outpaces antimicrobial development.
Development of Virulence
Virulence may develop through an existing but typically nonpathogenic microbe. Elizabethkingia anophelis is an example of such virulence development in humans; the risk in animals is unknown. This gram-negative bacterium is widespread in the environment and was considered innocuous until clusters of serious infections were identified in humans, primarily immunocompromised humans in hospitals, in various countries.10 The reasons for this change are unclear. Although E anophelis infection has not been reported in animals, it is possible that there is some degree of risk for infection. Regardless, E anophelis highlights the potential for organisms that were previously considered to be ubiquitous and innocuous to cause disease.
Change in the Range of Existing Pathogens
Many pathogens have well defined ranges that may be limited by geography and control measures (eg, rabies), vector ranges (eg, Borrelia burgdorferi), reservoir host ranges (eg, Cytauxzoon felis), and climate (eg, various parasites). Changes in any of these limiting factors can result in the potential for range expansion. Range expansion can also occur through human activities (eg, international movement of humans and animals) and accidental international transportation of pests and, thus, the pathogens they carry. Although of limited consequence in dogs and cats, introduction of West Nile virus through a route that is still unknown resulted in establishment of this foreign mosquito-borne virus in North America, and the impacts of this disease on humans and some animal populations are ongoing.11-15
Expanding ranges of various vector-borne diseases are particularly noteworthy. In North America, tick ranges have been expanding due in part to climate change.16 When reservoir hosts move in parallel with vectors or when competent hosts are already present in the expansion regions, vector-borne pathogens may spread with the vectors, as shown by the steady movement of Lyme disease into the northern and western United States and into Canada.17 Such movement highlights the need for predictive modeling to identify new threats and the need for awareness of disease threats in adjacent regions.
New Human Encounters in Remote Endemic Ranges
Various pathogens presumably exist in remote sites where there is little human presence. There are still regions of the world that have had limited human exposure, particularly parts of sub-Saharan Africa and regions of the Amazon basin. With the remarkable biodiversity in these areas, expansion of humans and their animals into these areas may result in exposure to pathogens considered new to the region.
Ability to Diagnose
Apparent emergence of a disease may sometimes simply reflect advances in diagnostic testing. For example, Bartonella spp can be difficult to identify. As new methods for detection have become available, members of this genus have been increasingly implicated in a variety of diseases.18
Advances in laboratory methods that allow for rapid, cost-effective detection of all microorganisms in a sample, including previously unknown bacteria and viruses, have made it possible to identify unknown microorganisms rapidly and at low cost. This has led to identification of myriad “new” viruses.19-21 Humans and animals have extensive commensal virome populations, and the ability to identify new viruses currently outpaces the ability to interpret the relevance of these discoveries. A high-profile example is the identification of canine circovirus. After reports of this virus and the subsequent ability to test for it first emerged, there was widespread concern about canine circovirus as a cause of serious enteric disease in dogs; however, proof of its role as a primary pathogen is still lacking.22-24 This highlights the potential confusion that can be associated with availability of new diagnostic tests when the clinical relevance of the results is unclear.
Change in Host Susceptibility
A change in host susceptibility has been exemplified in medicine early in the era of human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS). Before effective HIV management approaches were available, progression to end-stage AIDS resulted in profoundly immunocompromised individuals, which led to identification of a range of previously rare or unknown infectious diseases caused by organisms that were predominantly or only pathogenic in these highly compromised hosts (see Suggested Reading).25-29 Such a severely compromising and widespread disease is not currently recognized in animals; however, emergence of new secondary pathogens in humans with AIDS demonstrates the potential for disease caused by a range of novel or overlooked microorganisms associated with the emergence of new, highly susceptible patient populations. It also emphasizes the challenges that might be posed by advances in veterinary care (eg, treatment of cancer or immune-mediated disease) that can prolong the life of patients but increase their risk for infection from existing and emerging pathogens.
The Future
Logical estimations and models for emergence can be developed, but emergence is ultimately unpredictable. New infectious disease issues will pose threats to animal and, potentially, human populations. Infectious diseases of current significance may not have been recognized or considered important 5 to 10 years ago, and infectious diseases that will be significant 10 years from now may not be currently recognized or considered important, illustrating the dynamic nature of disease.
AIDS = acquired immune deficiency syndrome, HIV = human immunodeficiency virus