
Updated February 2025 by Katherine Doerr, DVM, DACVD; Veterinary Dermatology Center, Maitland and Rockledge, Florida
Profile
Definition
Demodicosis occurs when Demodex spp mites, which are part of the normal flora in dogs and cats, overproliferate in the skin (typically the hair follicle).
The incidence and prevalence of demodicosis are unknown.
Generalized demodicosis in dogs is associated with heritable factors; no known heritable tendencies have been found in cats.1
Read about diagnosis (including causes, signalment, laboratory testing, and risk factors) of demodicosis in Diagnosis of Demodicosis in Dogs & Cats.

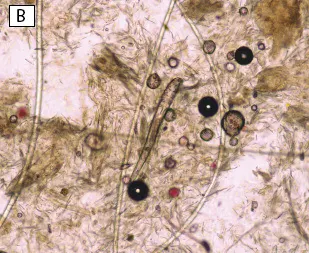

FIGURE Two species of Demodex spp mites affect dogs: Demodex canis (A) and Demodex injai (B; long-bodied mite). Two species of Demodex spp mites affect cats: Demodex cati (long-bodied mite) and Demodex gatoi (C; short- and wide-bodied mite). Magnification, 100×
Treatment
Inpatient or Outpatient
Demodicosis can be treated on an outpatient basis.
Concurrent bacterial/yeast overgrowth should be treated so miticidal therapy does not fail. In cases that lack appropriate response to antibiotics/antifungals, the skin should be cultured to rule out methicillin-resistant Staphylococcus pseudintermedius.
Dogs with adult-onset demodicosis and complications from underlying disease or dogs with deep pyoderma, fever, and sepsis may require hospitalization for supportive care and diagnostic testing.
In cats, hospitalization is rare and related to underlying conditions.
Medications
The only labeled treatment for demodicosis is amitraz every 2 weeks. Additional medications listed in this article are extra label, but use is supported by research.
All oral medications should be given with food.
Dogs
Fluralaner
25-50 mg/kg PO or topically every 90 days2
Fluralaner can be given to dogs ≥4.4 lb (2 kg) and ≥6 months of age.
Adverse effects are rare and include decreased appetite, ataxia, and vomiting.3,4
Afoxolaner
2.5 mg/kg PO every 4 weeks
Afoxolaner can be given to dogs ≥4 lb (1.8 kg) and ≥8 weeks of age.
Adverse effects are rare and include seizures, vomiting, dry skin, diarrhea, lethargy, and anorexia.5
Afoxolaner + milbemycin
Afoxolaner (2.5-6.3 mg/kg) + milbemycin oxime (0.5-1.07 mg/kg) PO every 4 weeks6
Adverse effects are rare and include seizures, vomiting, dry skin, diarrhea, lethargy, and anorexia.5,7
Sarolaner
2 mg/kg PO every 4 weeks
Sarolaner can be given to dogs ≥5.6 lb (2.5 kg) and ≥6 months of age.
Adverse effects are rare and include vomiting, diarrhea, lethargy, tremors, and ataxia.8,9
Lotilaner
20 mg/kg PO every 4 weeks
Lotilaner can be given to dogs ≥4.4 lb (2 kg) and ≥8 weeks of age.10
Adverse effects are rare and include vomiting, diarrhea, lacrimation, and hyperemic gingiva.11
Amitraz12,13
Product use is variable, and this drug is not marketed currently in the United States.
Ivermectin
300-600 micrograms/kg PO every 24 hours. Administration should be started at the low dose and gradually increased over 1 to 2 weeks to the maintenance dose.
Patients should be negative for heartworm disease.13
Aqueous formulations are more palatable than propylene glycol-based formulations.
Adverse effects include lethargy, muscle tremors, mydriasis, ataxia, severe neurotoxicosis (eg, depression, stupor, coma, ataxia, seizures, death), and blindness.
Multidrug sensitivity gene (MDR1 gene, also known as ABCB1 gene) mutation (also known as ABCB1-1delta) testing should be used to screen for sensitivity.
This drug should not be used in dogs or breeds sensitive to ivermectin.
Milbemycin oxime
1-2 mg/kg PO every 24 hours13
Patients should be negative for heartworm disease.
Milbemycin oxime can be given to dogs ≥2 lb (0.9 kg) and ≥4 weeks of age.
Multidrug sensitivity gene (MDR1 gene, also known as ABCB1 gene) mutation (also known as ABCB1-1delta) testing should be used to screen for sensitivity.
Adverse effects include lethargy, drooling, seizures, and depression.
Moxidectin/imidacloprid
This product can be administered topically every other week; however, weekly applications appear to be more effective.14,15
Patients should be negative for heartworm disease.
Moxidectin/imidacloprid can be given to dogs ≥3 lb (1.4 kg) and ≥7 weeks of age.
Multidrug sensitivity gene (MDR1 gene, also known as ABCB1 gene) mutation (also known as ABCB1-1delta) testing should be used to screen for sensitivity.
This drug is not as effective as other options.2,4
Adverse effects include lethargy, vomiting, diarrhea, blindness, and neurologic signs.13
Doramectin
600 micrograms/kg body weight SC or PO once weekly
Patients should be negative for heartworm disease.
Doramectin has been shown to be effective in small studies.16,17
Adverse effects are similar to ivermectin.
This drug should not be used in dogs sensitive to ivermectin.
Cats
Feline otic demodicosis
Topical milbemycin oxime (0.1% milbemycin oxime)12,13
Generalized demodicosis due to D gatoi or D cati12,13
Lime sulfur (topical leave-on agent) is the preferred treatment for D gatoi and can be administered once or twice weekly for 6 weeks; a higher concentration (8-oz product thoroughly mixed in 128-oz warm water) may provide faster resolution—cats tolerate warm water better. This product should be applied thoroughly (a rose-garden sprayer can be used) to soak the coat and skin and not rinsed off. Application should be in a well-ventilated area, and cats should be kept warm.
Milbemycin oxime (1-2 mg/kg PO every 24 hours) is well tolerated by most cats. Vomiting, diarrhea, and neurologic signs (rare) can occur.7
Aqueous ivermectin (300-600 micrograms/kg PO every 24 hours). Neurotoxicosis may develop.7,18
Doramectin (600 micrograms/kg SC injection once weekly)16
Moxidectin/imidacloprid has been used topically in a small number of cats anecdotally and can be administered weekly or every other week.
Fluralaner (28 mg/kg) PO once21
Response to treatment trial
Cats with suspected D gatoi infestation should be treated for at least 6 weeks.
Precautions/Interactions
Dogs without an ivermectin-sensitive genotype can show signs of toxicosis if ivermectin is given with P-glycoprotein inhibitors.
Commonly used dermatology drugs that can interact with ivermectin include erythromycin, itraconazole, ketoconazole, cyclosporine, and tacrolimus. (Oral tacrolimus use has not been recommended.19)
In most cases, application of topical tacrolimus does not result in significant absorption; however, in humans, significant absorption is possible if the agent is used over large areas.20
Glucocorticoids or other immune-suppressive medications should not be used in patients with Demodex spp.
Additional Medical Therapies
Fever, pain, sepsis, and dehydration should be treated in dogs with concurrent deep pyoderma.
Pain medication can be given to dogs with pododemodicosis if needed.
Sedation and clipping of the hair coat (especially in long-haired breeds) can facilitate medicated bathing.
Concurrent topical antimicrobial shampoo therapy (eg, 2.5% benzoyl peroxide, 3%-4% chlorhexidine, 1% ketoconazole) should be initiated.
Aggressive antimicrobial therapy is needed pending bacterial culture and susceptibility results in patients with deep pyoderma.
Patients with severe generalized demodicosis should be monitored during initial therapy for development of peripheral edema; systemic miticidal drugs can cause massive mite kills and obstruction of lymphatics.
Nutritional Aspects
A complete, balanced, age-appropriate diet should be fed, especially if the patient’s body condition is poor.asis.
Pet Owner Education
Dogs
Owners should be educated that localized demodicosis may progress to generalized demodicosis in ≈10% of affected dogs.
Owners should understand the cost and duration of treatment, especially for juvenile-onset generalized demodicosis, and the possibility of relapse or lack of cure.
A thorough workup of dogs with adult-onset demodicosis is needed. Owners should be informed of the implications of underlying disease and provided the advantages and disadvantages of treatment options.
Cats
Owners should be educated on the contagious nature of D gatoi and the need to treat all cats that come into contact with the infected cat.
Underlying predisposing disease is likely in cats with D cati, but evaluation costs to identify the underlying cause should be considered.
Owners should be given the advantages and disadvantages of treatment options.
Follow-Up
Patient Monitoring
In dogs, treatment should continue until at least 2, preferably 3, consecutive skin scrapings are negative at 1-month intervals.
The most common treatment error is stopping treatment too soon.
Complications
Relapse of generalized demodicosis in dogs is not uncommon.
Adult cats or dogs with demodicosis due to an underlying disease may not achieve remission unless the underlying disease is managed.
Prognosis
Dogs with generalized demodicosis require lifelong monitoring for relapse. A dog is considered cured when there are 2 negative deep skin scrapings 1 year apart.
Cats with D gatoi can be cured, and relapse is not an observed problem. D cati infestation will not resolve without treatment or management of the underlying disease.