Skin infections in veterinary patients are commonly treated with systemic antibiotics, but topical therapies can also be used.1 Topical therapy is available in various formulations (eg, shampoo, spray, mousse, cream, spot-on) and can be tailored to body regions, coat types, and pet owner capabilities. All treatment options for dermatologic disease should be considered to support antimicrobial stewardship and ensure antibiotics remain effective.
Following are the author’s top topical therapies to reduce systemic antibiotic use.
1. Chlorhexidine ± Miconazole
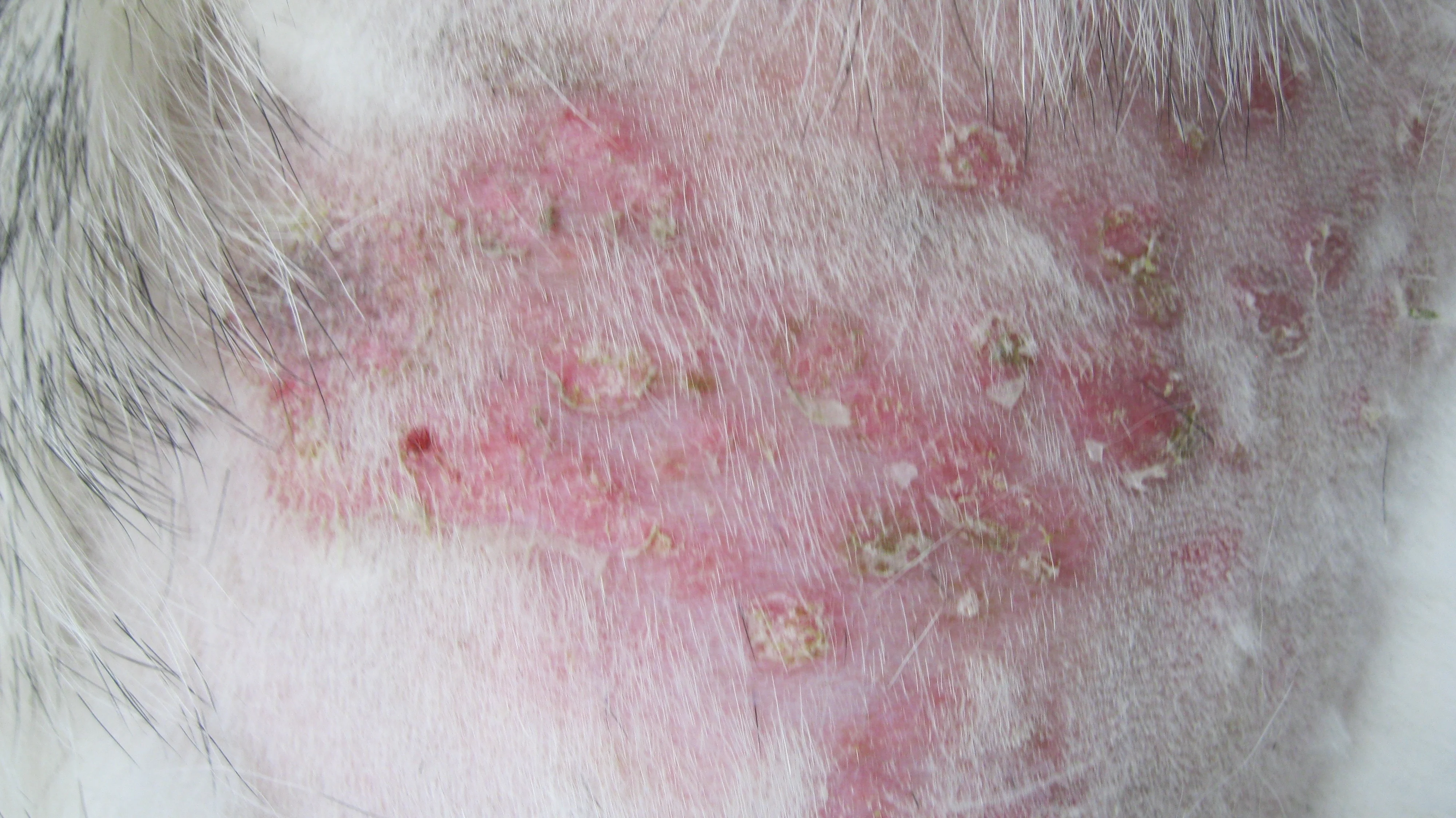
Topical antiseptics can replace systemic antibiotics in dermatology cases, particularly for treatment of superficial pyoderma (Figure 1), and are recommended when impression cytology shows bacteria or yeast (Figure 2). If yeast are the predominant microorganisms on cytology, systemic antibiotics are not indicated. Topical antiseptics alone can be effective for treatment of bacterial pyoderma.2-6 Chlorhexidine and miconazole are synergistic in vitro against Staphylococcus pseudintermedius, killing bacteria more effectively than either ingredient alone.7,8 A variety of commercial products containing 2% chlorhexidine and 2% miconazole are available; products with up to 4% chlorhexidine alone are also available.
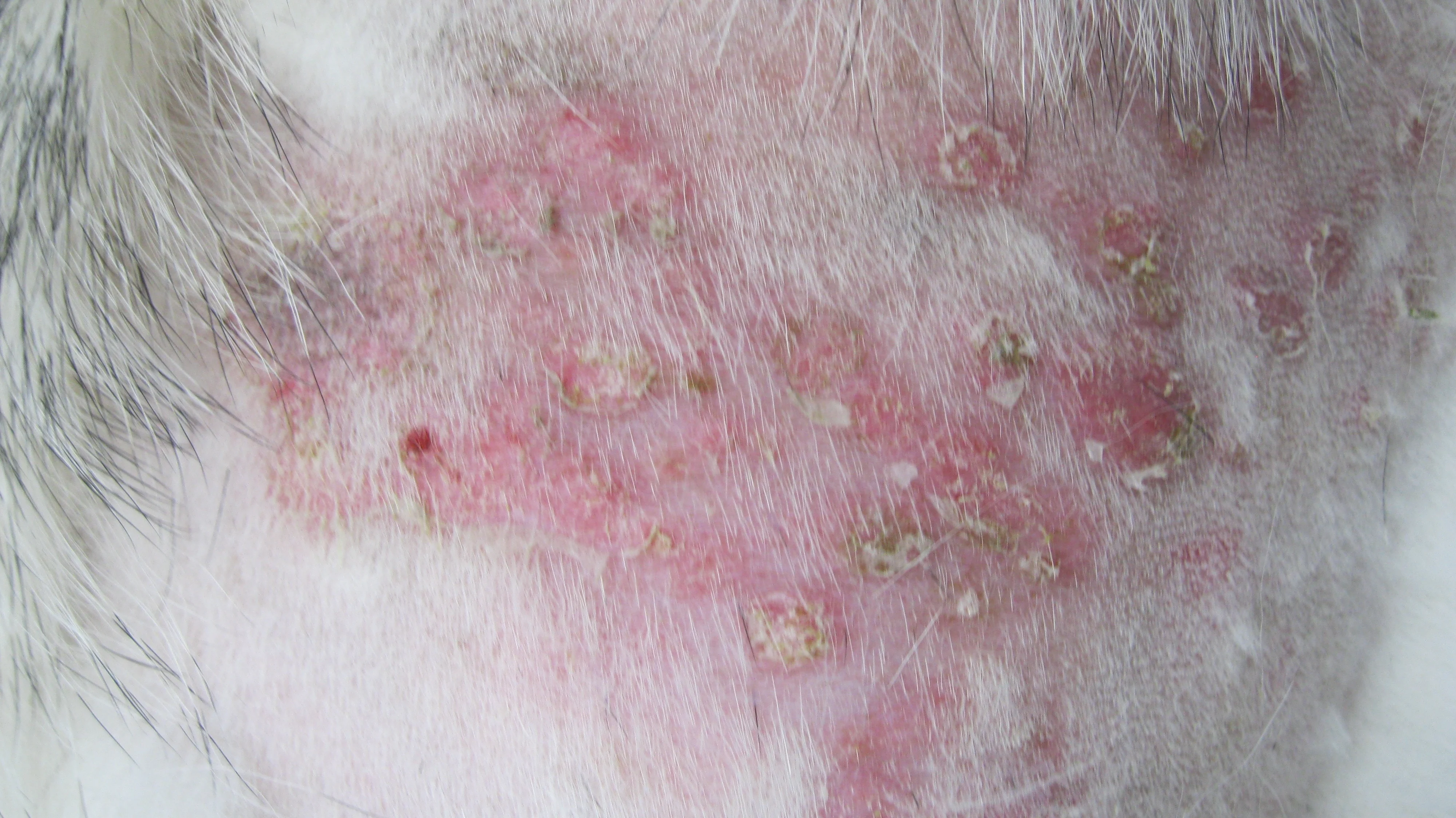
FIGURE 1 Papules, crusted papules, and epidermal collarettes typical of superficial pyoderma can be seen in a dog. These lesions can be treated solely with topical chlorhexidine with or without miconazole in many patients.
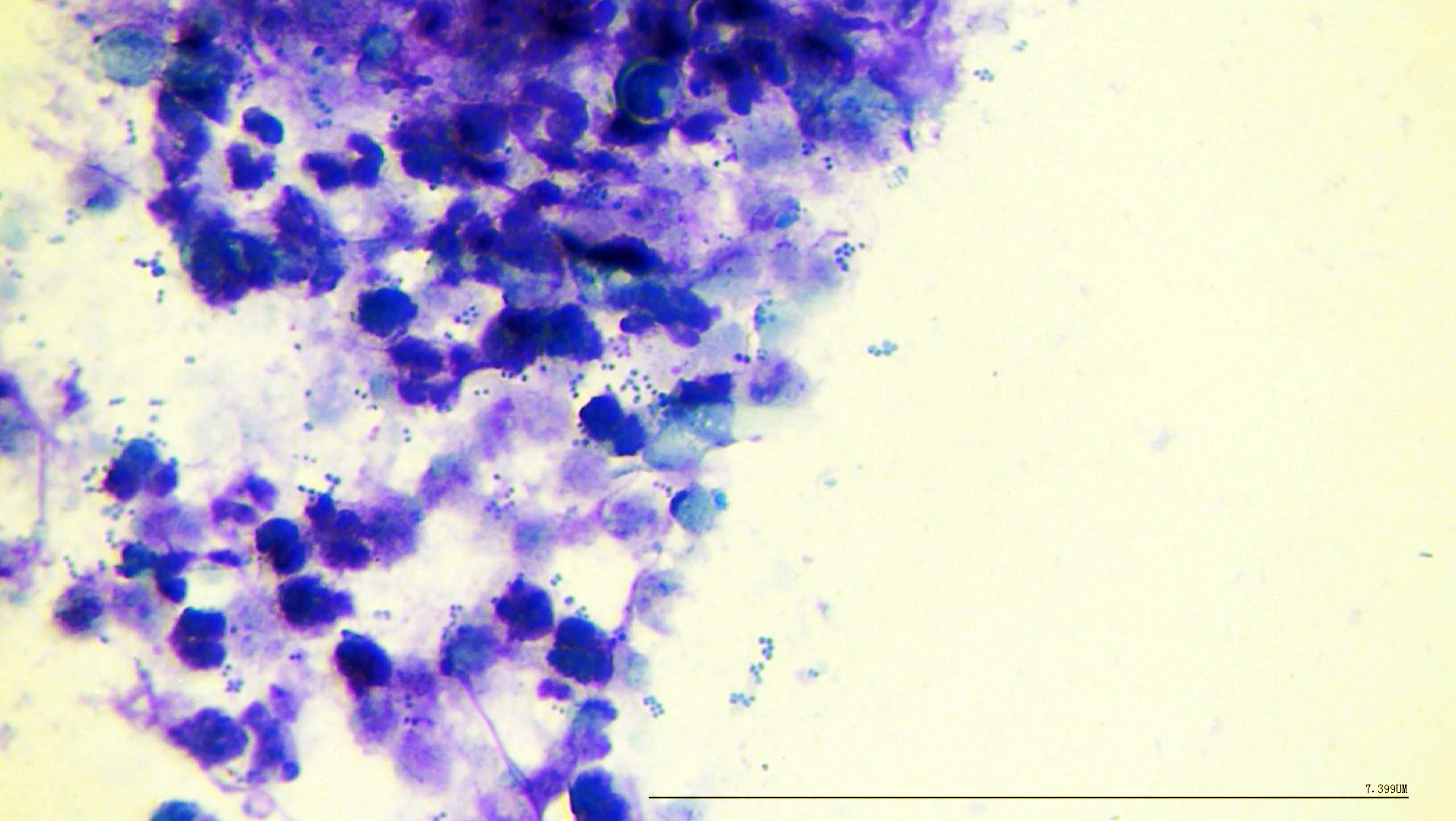
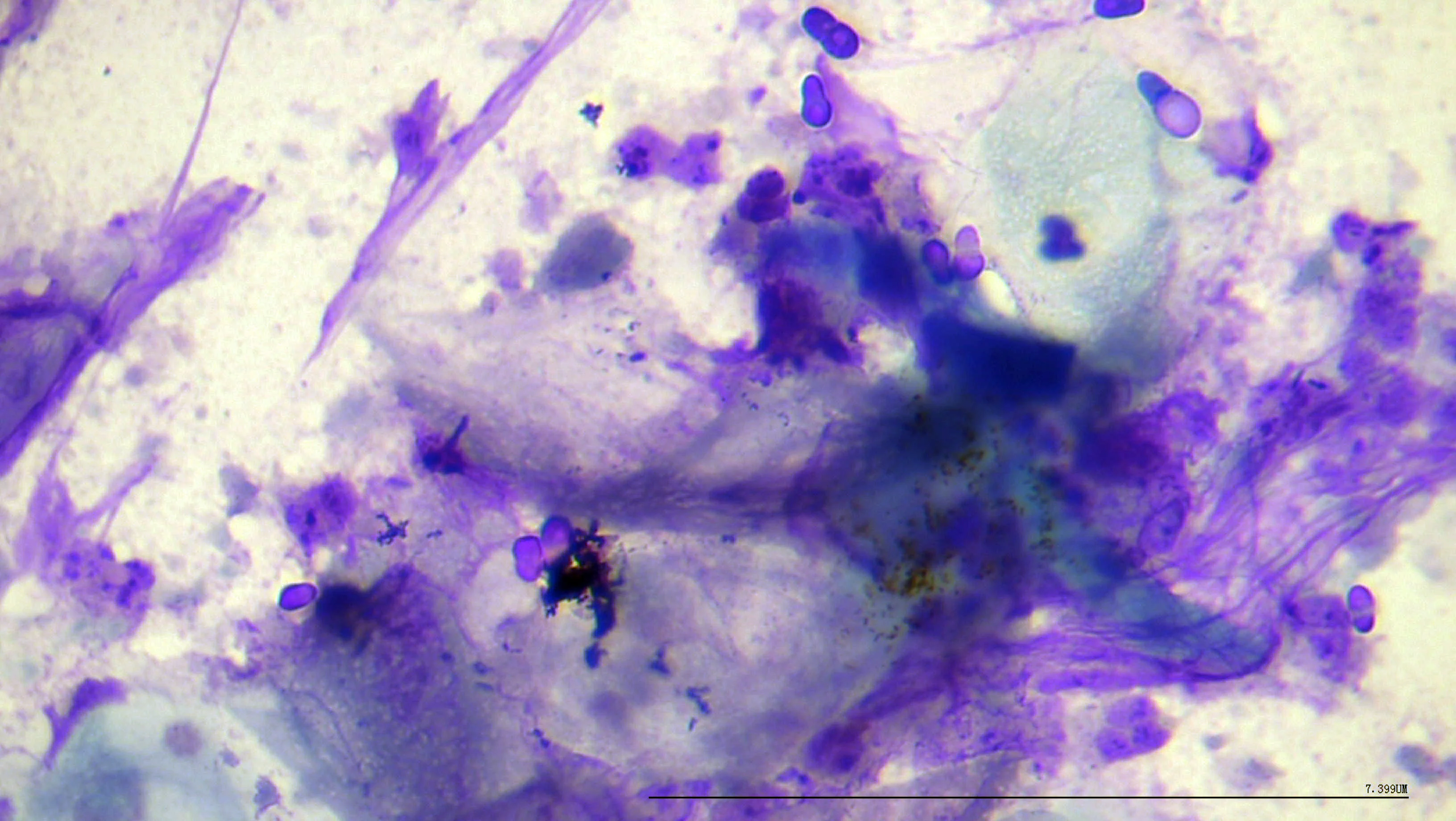
Numerous coccoid bacteria and neutrophils on impression cytology from superficial pyoderma (A); moderate number of yeast and neutrophils on impression cytology from yeast dermatitis (B). 100× magnification
Shampoo is important for removal of scale, grease, dirt, and allergens. Emphasizing the importance of skin and coat hygiene can improve owner compliance, and specific instructions (eg, bathe entire body twice per week for 4 weeks, use spray daily on nonbath days for 4 weeks) should be given. When the underlying trigger for pyoderma (eg, flea allergy dermatitis, demodicosis, Sarcoptes spp infestation) can be controlled, antiseptic shampoo alone can treat superficial pyoderma. Mousse, spray, and wipe products can be useful for specific body regions (eg, face/lips, perineum).
2. Corticosteroids
Atopic dermatitis is a common underlying cause of superficial pyoderma. Atopic skin inflammation combined with a compromised epidermal barrier allows overgrowth of normal flora that is worsened by self-trauma.9 Bacterial pyoderma and yeast dermatitis are often complicating factors of atopic dermatitis, but not all patients with itchy, red skin have infections. If cytology samples from multiple affected areas are negative for bacteria and/or yeast, topical corticosteroids can control inflammation and prevent self-trauma and the need for systemic antimicrobials.
Other inflammatory skin conditions (eg, interdigital furunculosis, acute moist dermatitis) can often be controlled with topical corticosteroids alone or in combination with topical antiseptics when indicated by cytology.10 Interdigital spaces and ear canals are particularly amenable to topical corticosteroid therapy. Appropriate corticosteroid formulation is critical to avoid cutaneous adverse effects (eg, skin atrophy, ulceration, milia; Figure 3). Highly potent corticosteroids (eg, betamethasone) should be avoided on areas with thin skin (eg, inguinal and axillary regions), and caution is needed with frequent administration of lower-potency corticosteroids (eg, hydrocortisone aceponate, triamcinolone) to avoid cutaneous adverse effects. Triamcinolone acetonide 0.015% spray is a corticosteroid-only product FDA-approved to control pruritus associated with atopic dermatitis in dogs.11 Hydrocortisone aceponate 0.584 mg/mL spray is available outside the United States and can be an effective sole treatment for canine otitis externa.12

Severe cutaneous corticosteroid adverse effects (ie, skin atrophy, erosion, milia) following multiple daily applications of a spray containing gentamicin and betamethasone over several months in the right inguinal region of an atopic 5-year-old neutered male golden retriever/standard poodle crossbreed
Many topical corticosteroid preparations exist for human use. Studies on optimal doses in veterinary patients have not been published; therefore, the lowest frequency of application that controls clinical signs should be used. Triamcinolone 0.1% cream is widely available and effective for localized inflammatory lesions of the paws, nasal planum, and pressure points. If pyoderma is diagnosed based on cytology, antiseptic shampoo or spray (see Chlorhexidine ± Miconazole) can be used in combination with a topical corticosteroid to avoid unnecessary use of gentamicin, a broad-spectrum antibiotic commonly combined with ultrapotent betamethasone in a variety of veterinary spray products.
3. Fluorescence Biomodulation
Fluorescence biomodulation (FBM) comprises application of a photoconverting gel containing chromophores that produce multiple wavelengths of light with broad biologic action to a lesion in a 2-mm layer, followed by application of fluorescent light for 2 minutes. This process is generally repeated twice per week until the lesion is healed; protocols vary based on severity and clinician experience. FBM can treat larger areas of skin compared with low-level laser light therapy, which has low evidence of efficacy for dermatologic conditions.13,14 The precise mechanism of action is not understood. Although laboratory studies have not demonstrated bactericidal activity, clinical evidence supports FBM as sole or adjunct treatment for localized pyoderma, infected surgical incisions, interdigital furunculosis, and other inflammatory skin conditions (Figure 4).15-17


Right thoracic limb of a 4-year-old spayed blue heeler crossbreed with 2 acral lick granulomas before (A) and after (B) 8 weekly treatments with FBM and oral naltrexone and fluoxetine
4. Epidermal Barrier Repair
Most skin diseases disrupt the barrier provided by the skin, predisposing the skin to dysbiosis that manifests as secondary bacterial infection.18 Topical therapies that improve the barrier can reduce this predisposition and the need for systemic antibiotics. Other conditions that involve a compromised epidermal barrier include primary disorders of keratinization (eg, forms of ichthyosis, idiopathic seborrhea, nasodigital hyperkeratosis) and sebaceous adenitis. Standard poodles have a genetic predisposition to sebaceous adenitis, which may increase in incidence as standard poodle crossbreeds become more popular.
Secondary infections detected on cytology should be treated with topical antiseptics and barrier repair therapy to replace epidermal lipids lost due to sebaceous gland destruction in sebaceous adenitis and altered epidermal function in other disorders.19,20 Other advantages of barrier repair include reduced inflammation, normalization of keratinocyte turnover, and inhibition of microorganisms.18,20 Barrier repair ingredients include fatty acids, phytosphingosine, ceramides, and plant-derived oils. Spray, mousse, and spot-on formulations are available. Clinical reports of efficacy are available; however, rigorous clinical trials for specific products have not been published, and some trial and error is necessary to determine which formulation and frequency of application are useful for specific conditions.20 Maintenance barrier repair therapy can provide ongoing prevention of infection as clinical signs are controlled.
5. Medical Honey
Honey has historically been used for wound treatment and can benefit healing through fibroblast proliferation, decreased edema, bactericidal activity, and possible antibiofilm properties (depending on the dominant plant nectar).21 Studies have shown in vitro activity against skin pathogens,22 but evidence to support use of honey for treatment of superficial pyoderma is lacking.23 Distinguishing superficial pyoderma from skin wounds is key because honey is useful for treatment of skin wounds (eg, bite wounds, lacerations, burns, postsurgical wounds, pressure sores).24 Systemic antibiotics may not be necessary with proper surface cleaning and wound management.25 Medical-grade honey products processed for safety and sterility are available through medical distributors and online without a prescription.
Listen to the Podcast
Dr. Layne joined the podcast to emphasize the critical role of topical treatments in veterinary dermatology and their potential to reduce reliance on systemic antibiotics.