
Enucleation is recommended in patients with a blind and painful eye or an intraocular tumor that cannot be effectively resected using other methods. Conditions that can lead to enucleation include glaucoma, severe uveitis, ocular trauma, and perforated corneal ulcers. The primary goals of enucleation are removing a source of chronic pain, infection, and/or metastasis, as well as gathering diagnostic information regarding the contralateral eye and therefore patient systemic health.
Techniques
Multiple techniques for enucleation are available. It is important to consider the underlying disease process when choosing an approach.
Subconjunctival Approach
The most common technique is the subconjunctival approach, in which the globe is reached via dissection through the conjunctiva. The eyelid margins, conjunctiva, and third eyelid are then resected. This approach should not be used if there is obvious infection of the conjunctiva, neoplasia of the extraocular surface, or corneal perforation.
Transpalpebral Approach
With the transpalpebral approach, initial dissection is made through the eyelids, allowing removal of the globe and associated supportive and secretory tissues as one unit. This approach minimizes the risk for leaving residual conjunctival tissue (which can cause draining fistulas from the orbit) and is recommended for neoplasia or infection (as there is less risk for spread of ocular surface contaminants throughout the orbit). The transpalpebral approach is discussed in this article.
Step-by-Step: Transpalpebral Enucleation
What You Will Need
Sterile drape
Towel clamps
Sterile gauze
Surgical staples
#10 scalpel blade and handle
Allis tissue forceps
Colibri forceps
Stevens tenotomy scissors
Bishop-Harmon forceps
Barraquer needle holder
4-0 absorbable suture
6-0 nonabsorbable suture
Absorbable gelatin sponge
Sterile bowl
Sterile saline
3-mL syringe
Vacuum pillow

Step 1
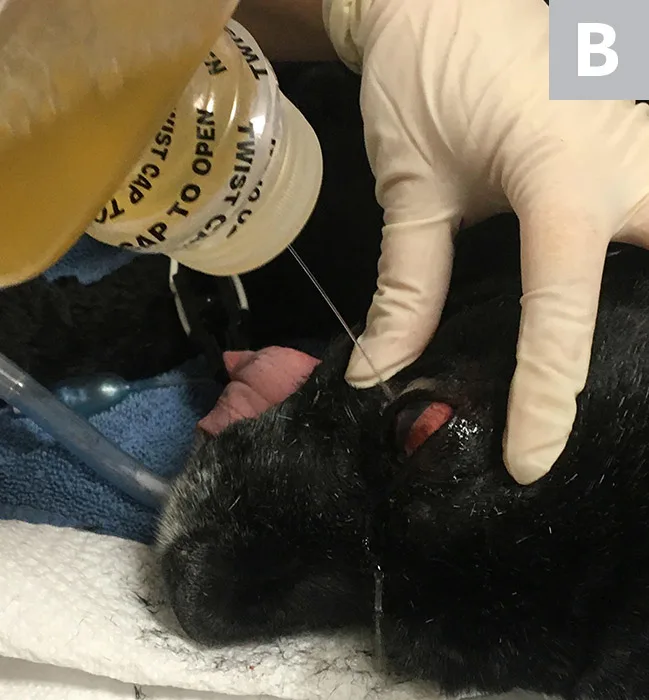
Place the patient in lateral recumbency with the surgical eye facing upward. Shave the eyelids (A), and prepare the periocular and ocular surface tissues with dilute povidone iodine (add povidone iodine [4 mL] to sodium chloride [1,000 mL]; B). Contact time for irrigation of the globe and associated structures is ≈2 to 3 minutes. Position and support the head with a vacuum pillow (C). Perioperative cefazolin can be administered intravenously at this time.


Author Insight
A retrobulbar block may be performed with 2% lidocaine (2 mL) and/or 0.5% bupivacaine (2 mL) to provide intraoperative and postoperative analgesia. Before injection, the syringe plunger should be drawn back to check for aspirated blood to avoid inadvertent injection into a vessel. Acceptable approaches include the inferior–temporal palpebral and supratemporal routes (Figure). Alternative analgesia options include intraoperative bupivacaine splash blocks and intraorbital lidocaine–bupivacaine infused absorbable gelatin sponges.

Step 2
Reirrigate the eyelids with dilute povidone iodine, and drape the surgical site.
Author Insight
Surgical scrubs that contain detergents should be avoided. Periocular skin and ocular surface require presurgical prepping with sterile drape after povidone iodine has been used to clean the periocular and ocular surfaces.

Step 3
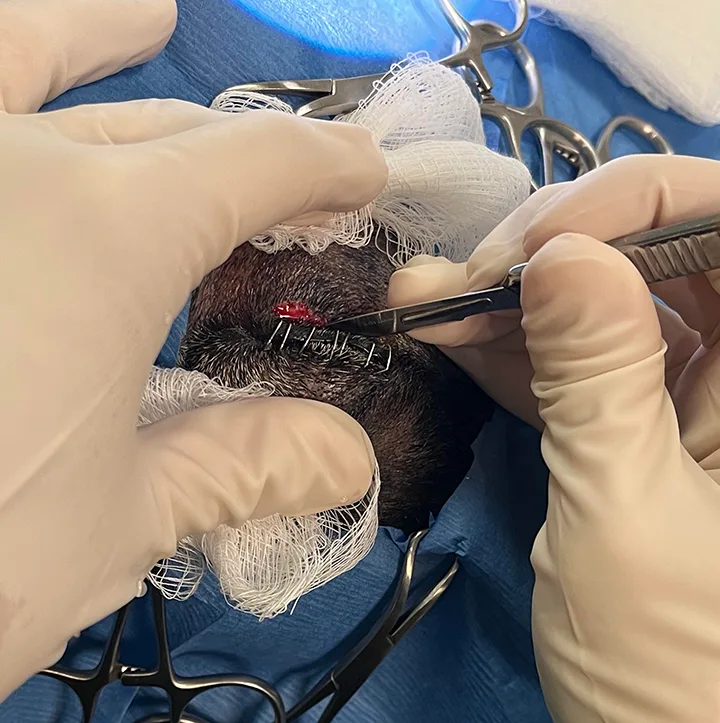
Suture the eyelids closed with an absorbable or nonabsorbable suture in a continuous suture pattern.
Author Insight
Initial incisions should be no further than 2 mm from the eyelid margin, and caution should be used with wide bites of the suture to avoid accidentally cutting out the appositional layer. Alternatively, surgical skin staples can be used (Figure).

Step 4
Using a #10 scalpel blade, make 2 elliptical skin incisions into the eyelids ≈2 mm from the lid margin, completely encircling and including the medial and lateral canthus.

Step 5
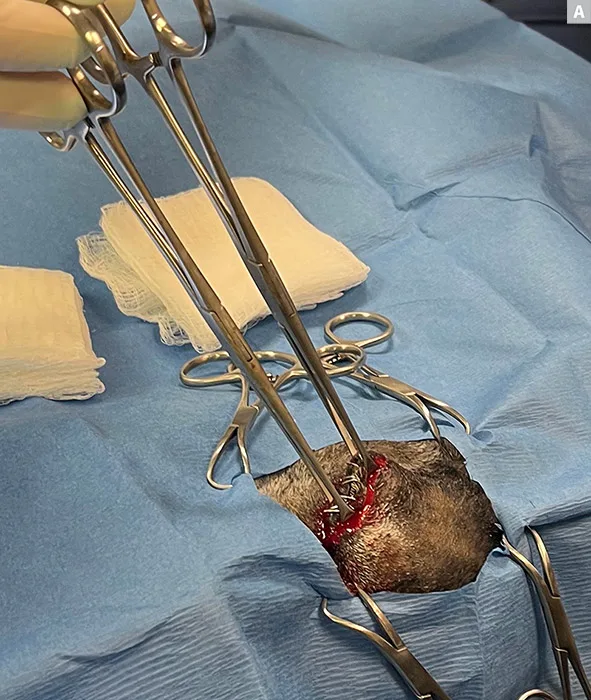
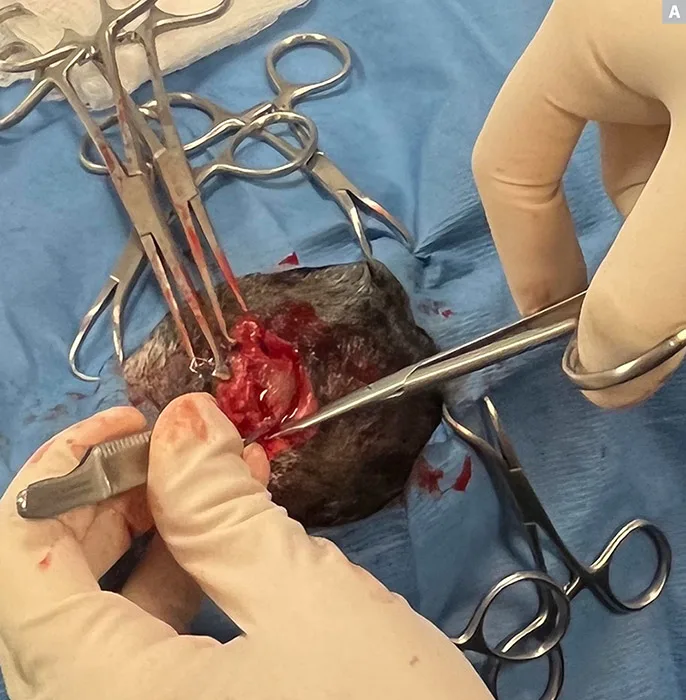
Use Allis tissue forceps to grasp the eyelid margins (only grasp tissue intended to be excised), creating mild traction to aid with initial dissection (A). Transect the canthal ligaments, and dissect the superficial eyelid fascia with light sweeps of the scalpel blade until just posterior to the limbus (B, C).

Step 6
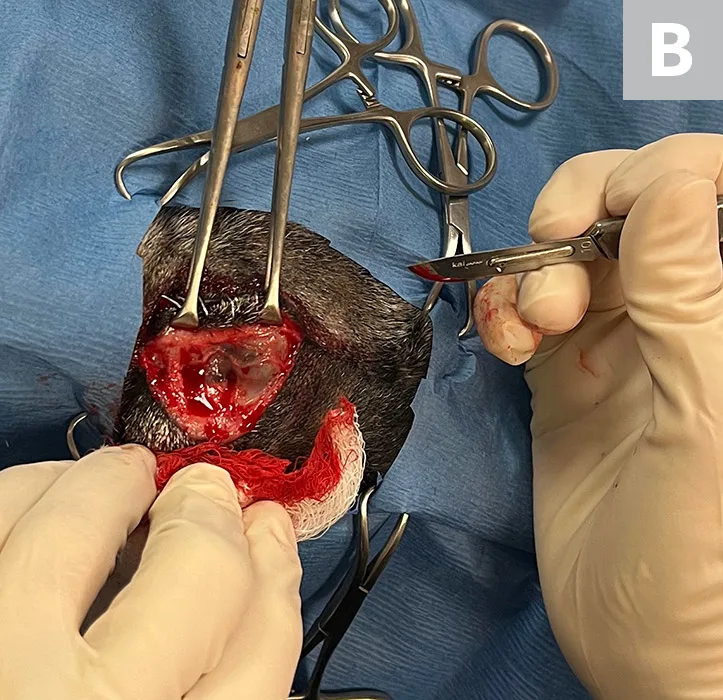
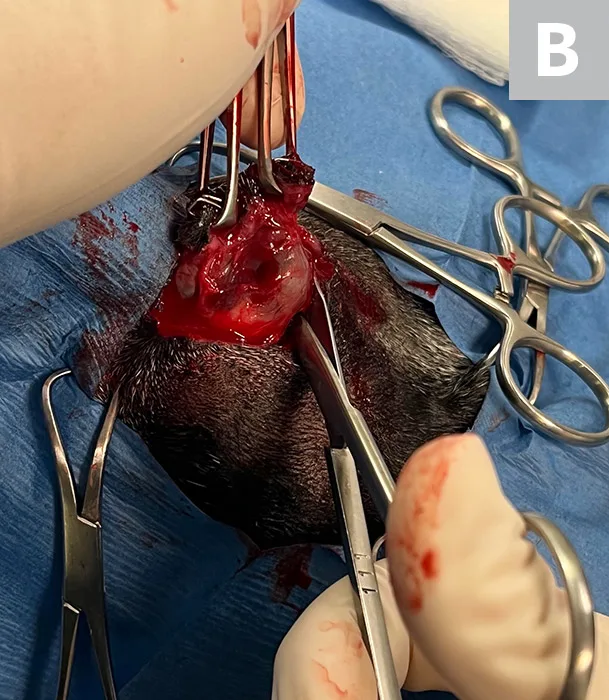
Perform deep dissection through the periorbital tissue with Stevens tenotomy scissors (A). Dissect toward the globe until the sclera is visualized, then extend the pocket around the globe with a combination of blunt dissection and cutting (B). Transect the extraocular muscles close to their scleral insertion, allowing the globe to be mobilized. Use caution in the dorsomedial location near the orbital rim to avoid transecting the medial angularis oculi vein. If this is transected, ligate the vessel.
Step 7
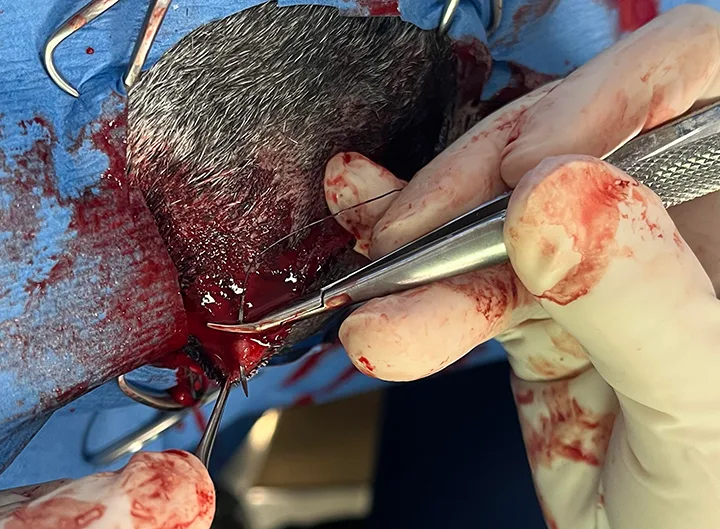
Place slight traction, reach behind the globe with the scissors held open, and cut the optic nerve.

Author Insight
The optic nerve should not be clamped before cutting to avoid damage to contralateral optic nerve fibers at the optic chiasm. Minimal traction to the ocular tissues is needed to protect the contralateral eye. Excessive traction on the eye should be avoided to limit the risk for oculocardiac reflex.
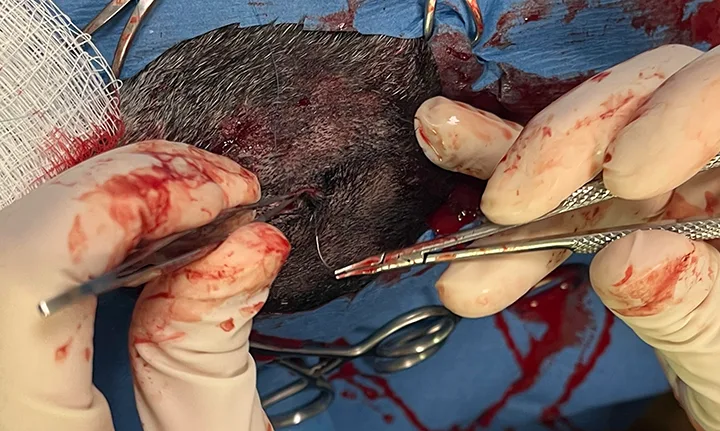
Step 8
Remove the globe, pack the orbit with gauze sponges, and apply firm digital pressure for 2 to 3 minutes to control hemorrhage. Once hemorrhage is controlled, remove the gauze and irrigate the orbit with sterile saline.

Step 9
Soak a sterile absorbable gelatin sponge with bupivacaine (optional) and place in the orbit.

Author Insight
Absorbable gelatin sponges are typically absorbed in 4 to 6 weeks.
Step 10
Close the deep fascial layers and subcutaneous tissues with 4‐0 absorbable suture material in a simple continuous pattern.

Step 11
Close the skin with simple continuous or interrupted sutures using 6-0 nonabsorbable monofilament suture.

Postoperative Care
Systemic antibiotics and systemic pain management should be given for 2 weeks postoperatively. Postoperative antibiotics should be administered if there is a break in sterility or noticeable abscessation in the orbit. Typically, cephalexin (22 mg/kg PO every 12 hours for 2 weeks) can be administered.
Systemic NSAIDs should be used if not contraindicated to reduce surgical site inflammation.
A cold compress can be applied for 10 to 15 minutes immediately following surgery to help reduce inflammation.
Skin sutures should be removed after 10 to 14 days.
Patients should wear an Elizabethan collar until sutures are removed to prevent self-trauma.
Normal postoperative findings include mild serosanguinous drainage from the incision site and/or ipsilateral nostril for 2 to 3 days, as well as swelling and bruising of the incision site.
Complications may include the following:
Hemorrhage within the first few hours following surgery (most common) that can be controlled with cold compresses, pressure bandages, exercise restriction, and/or mild sedation
Draining orbital fistulas due to incomplete removal of the medial canthus, conjunctiva, or third eyelid gland
Orbital infection
Orbital emphysema (less common; can occur in brachycephalic breeds)
Listen to the Podcast
Listen in as Dr. Haeussler discusses the common indications for enucleation, typical complications, dives deeper into the details of the transpalpebral approach.