Topical Serum for Treatment of Keratomalacia
Amy Knollinger, DVM, DACVO, Eye Care for Animals, Salt Lake City, Utah

Corneal Anatomy
An understanding of corneal anatomy is vital to determine if serum therapy for the treatment of keratomalacia should be initiated. The cornea makes up the anterior portion of the globe and provides multiple functions for vision: it is transparent (despite originating from surface ectoderm), thereby allowing for clear vision; it acts as the major refractive (bending of light) surface of the globe; and it provides a protective barrier between the globe and the environment
The cornea consists of 4 layers in domestic species, being approximately 0.45–0.55 mm thick in the normal dog. The corneal epithelium is the most external layer overlying the stromal layer, which accounts for 90% of the total corneal thickness. The corneal epithelium in the dog and cat is 5–11 cells thick and has a turnover rate of approximately 7 days.1 The stroma is made up of collagen fibers, which are precisely arranged in parallel sheets running the entire diameter of the cornea, allowing for its transparency. The third layer is an acellular membrane (ie, Descemet’s membrane), which forms the basement membrane for the innermost layer, the endothelium. The corneal endothelium is a single layer of hexagonally shaped cells forming the internal barrier between the anterior chamber and the cornea.2
Corneal Disease
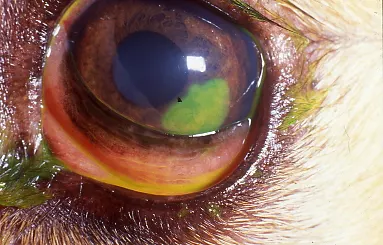
Corneal ulcers are classified by underlying cause. Common causes of corneal ulcerations include trauma (foreign bodies, scratches), desiccation (keratoconjunctivitis sicca, lagophthalmos), or eyelid abnormalities (eyelid masses, distichiasis, or ectopic cilia). Recognition of the primary cause is important; if not treated effectively, progression or recurrence of corneal ulceration is likely. Diagnosis of corneal ulceration can be made by evaluation of clinical signs and a positive fluorescein stain test (Figure 1).
Noninfected superficial corneal ulceration
Corneal ulcers are also classified by the depth of corneal involvement. Superficial corneal ulcers are those in which only epithelium is lost, have no signs of infection, and usually heal rapidly (5–7 days). Conversely, complicated corneal ulcers have yellowish cellular infiltrate (indicative of infection), and frequently have, or will progress to have, corneal stromal loss.
Uncomplicated corneal ulcers are usually superficial and heal rapidly. These ulcers are not infected and do not progress. Conversely, complicated corneal ulcers are typically more chronic in nature and have other underlying factors that cause them to be progressive.2 For any corneal ulceration, it is important to perform initial diagnostics. Cytologic analysis of the corneal surface and performing a culture and sensitivity test is recommended to determine proper antimicrobial therapy.
Keratomalacia
Keratomalacia, defined as collagenolysis, is the rapid breakdown or melting of the corneal stroma (Figure 2). Clinically, keratomalacia is characterized by a soft, gelatinous appearance of the cornea. This rapidly progressive condition occurs typically in response to corneal injury and involves infiltration of white blood cells. Corneal repair normally involves the production of proteinases and collagenases to remove damaged corneal tissue, which causes the characteristic melting appearance.

Severely infected deep corneal ulceration with keratomalacia. This canine patient also has borderline keratoconjunctivitis sicca.
In early stages of injury, keratomalacia is primarily bacterial in origin, particularly Pseudomonas spp. When keratomalacia is present, intensive medical therapy is required to arrest corneal deterioration as quickly as possible. Targeted antimicrobial therapy, both orally and topically, and anticollagenase medications should be started immediately to control both the corneal infection and keratomalacia. Corneal ulceration (especially superficial corneal ulceration) is painful, and systemic analgesia is always recommended. Systemic opioids (tramadol, buprenorphine), with or without the use of an NSAID, are suggested for analgesia. Finally, an Elizabethan collar is highly recommended to prevent further self-trauma and globe rupture.
Melting corneal ulcers should be reexamined within 24 hours to determine the extent of progression. Malacic ulcers can progress rapidly, prompting referral to a veterinary ophthalmologist for surgical stabilization of the cornea. If not aggressively treated, full thickness perforation can occur, leading to globe rupture.
Autologous Serum as Antiproteinase Therapy
When a melting ulcer is suspected, antiproteinase and anticollagenase (ie, antimelting) therapy is strongly recommended to prevent further stromal loss. Several antiproteinases are available for veterinary ophthalmic use. These include N-acetylcysteine (NAC), disodium ethylenediaminetetraacetic acid (EDTA), oral tetracyclines, and autologous serum. Autologous serum contains what is considered the most effective inhibitor of collagenase activity. Therefore, if a melting ulcer is suspected, frequent topical ophthalmic application of autologous serum is highly recommended. Finally, autologous serum also contains factors that may reduce discomfort.
Step-by-Step: Aseptic Collection of Autologous Serum
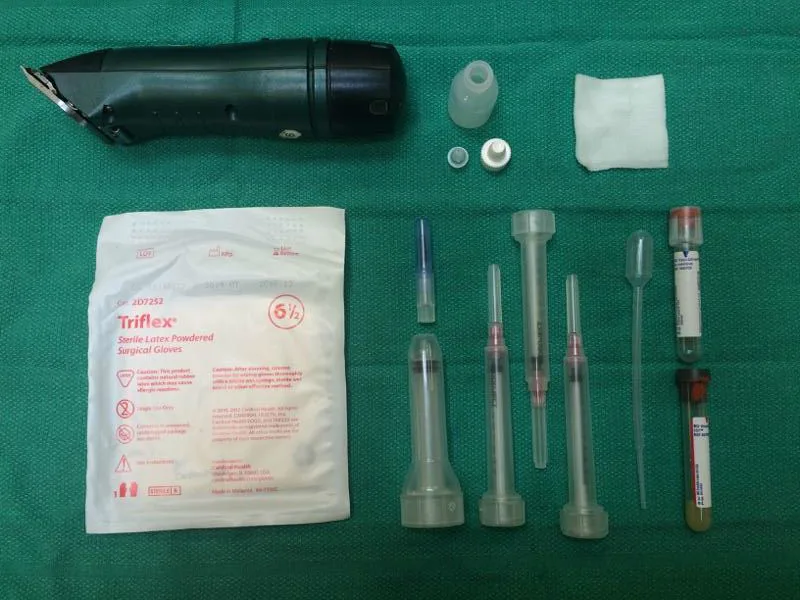
What You Will Need
Sterile gloves
Clean #40 clipper blade
Chlorhexidine scrub and solution
Sterile needle and syringe
Red top sterile blood collection or serum separator tube
Centrifuge
Sterile pipette
Sterile multidose injection vial
Sterile 1-mL syringes
Step 1
Clip and clean the skin around the area of a vein on the patient, typically either the jugular vein or a cephalic vein. This helps prevent normal skin flora from contaminating the blood sample.
Step 2
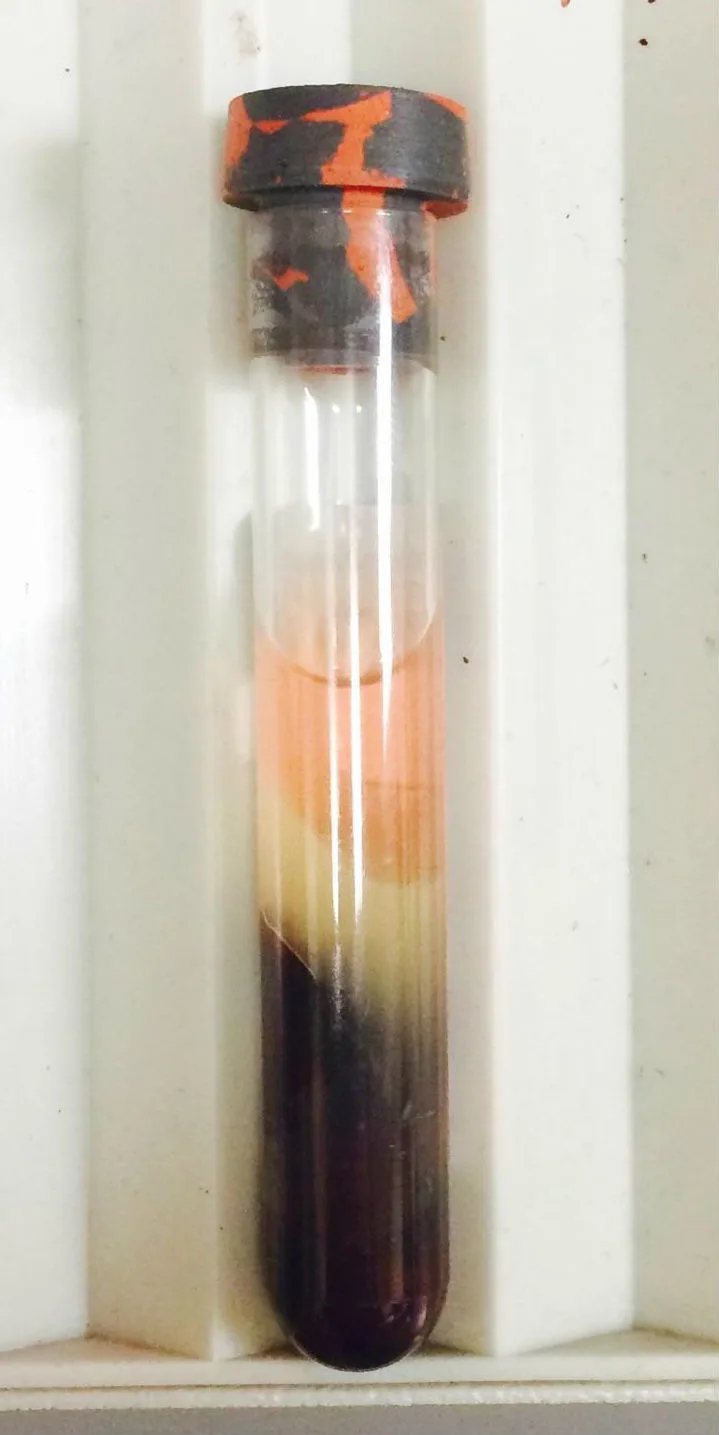
Collect a blood sample—as much as safe and feasible. Once the blood is drawn, allow it to clot in a sterile standard red top blood collection tube or serum separator tube
Step 3
Once coagulation is complete (approximately 10 minutes), centrifuge the blood tube for 10 minutes to separate the serum.
Step 4
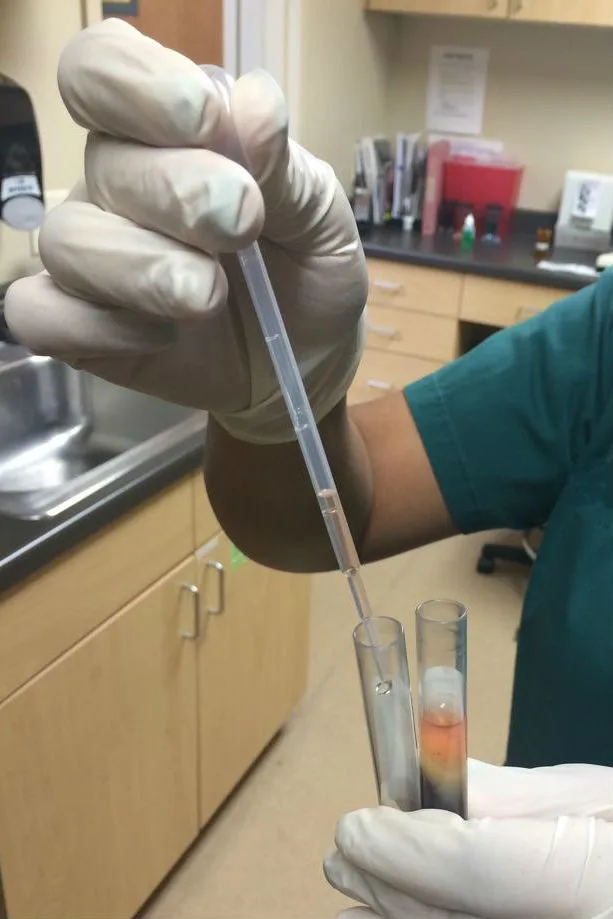
Carefully draw off the resulting serum with a sterile pipette and introduce into an empty sterile multi-dose injection vial.
Step 5
Draw off serum from the injection vial and inject into 1-mL syringes aseptically and keep refrigerated. Alternatively, serum can be stored and applied from a sterile dropper bottle.
Step 6
Periocular hair can be clipped short around the affected eye to prevent hair contamination and help with owner compliance giving topical medications and cleaning (Figure 3). Extreme caution should be used during the clipping process, as excessive pressure on the globe can cause globe rupture.

Step 7
Serum can be placed topically on the eye directly out of the syringe with the needle removed. Larger volume syringes should not be used to avoid bacterial contamination, which is very common because of the high protein content of serum.4,5 A bacteriostatic agent or preservative does not need to be added if the serum is produced in a sterile manner.
Author Insight
The multidose vial can be used as a reservoir for any remaining serum, which can be stored safely for up to 7 days if refrigerated.
Step 8
One drop of the autologous serum should be applied every 1–2 hours initially during medical therapy. These drops can be reduced to every 4 hours once proteolytic activity has been halted and the corneal tissue becomes healthier, usually between 48 and 72 hours after initiation of aggressive medical therapy. Hospitalization for the first 24–48 hours is indicated for administration of intense medical therapy and monitoring of the patient for worsening condition.
Expert Insight
Autologous serum can be used when keratomalacia is suspected. Complications of the use of autologous serum are rare, so it can be used safely in most ulcerative keratitis patients even if keratomalacia is not present.
Monitoring for worsening ulcerative keratitis is important if an infectious cause or melting cornea is present. Reexamination is recommended within 24 hours to ensure the ulcer or melting has not worsened, as changes can occur very quickly. Hospitalization in the initial 24 to 48 hours is indicated for appropriate monitoring of the patient and/or for compliance to the intense medication regimen.
Keeping periocular hair clipped short and the area dry is key for preventing skin infections secondary to excess ocular discharge (Figure 3). Use extreme caution when shaving and handling in order to not cause globe rupture if deep ulcer is present.


Long-haired Shih Tzu requiring clipping (A); appropriately clipped periocular region (B)
Proper client instruction is needed for administration of autologous serum and all ophthalmic medications at home. Clients should be informed to tip the nose of the patient as high as possible and to place a drop onto the ocular surface (conjunctiva or cornea). Opening the eyelids is not recommended, as this can cause excess ocular pressure, possibly leading to globe rupture if a deep ulcer is present.