Top 5 Tips for Successful Anesthetic Monitoring
Rebecca A. Johnson, DVM, PhD, DACVAA, University of Wisconsin
Anesthesia requires diligent, accurate patient assessment before, during, and after the procedure. Appropriate monitoring allows for early detection of, and intervention in, anesthetic complications. The following 5 tips, although not comprehensive, can help ensure optimal anesthetic monitoring.
1. The anesthetist is the most important monitor.
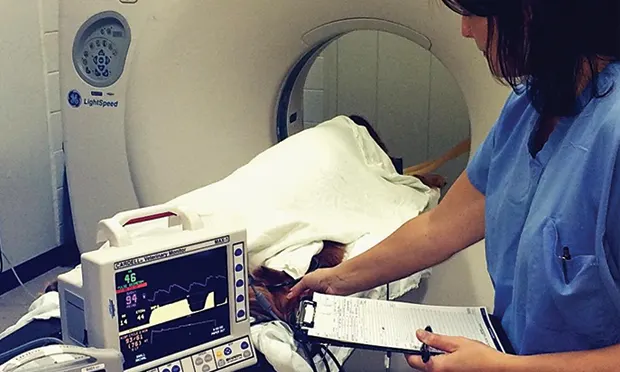
Extreme vigilance is required throughout the anesthetic procedure (ie, during premedication, anesthetic maintenance) and into the postanesthetic recovery period, and skilled, attentive team members are key.1 A dedicated anesthetist (ie, a veterinarian or certified veterinary technician) familiar with all monitoring equipment, as well as hands-on techniques, should be responsible for monitoring patients. He or she can assess muscular tone and ocular and withdrawal reflexes, palpate pulses, auscultate cardiac and pulmonary sounds, and observe changes in mucous membrane color and respiration quality; this information is frequently missed if monitoring equipment only is used (Figure 1).

A hands-on approach (eg, palpating pulses) with anesthetic monitors provides information used to assess an anesthetized patient.
Constant vigilance is key, and the anesthetist should record the physiologic parameters every 5–10 minutes and note them in the patient’s medical record (Figure 2). This will allow the anesthetist to follow changes in patient physiology and provide a permanent document to refer to during subsequent procedures (eg, regarding choice of drugs and doses, endotracheal tube size, anesthetic complications).

An anesthetic record
2. Combine pulse oximetry & capnometry.
Simultaneous use of pulse oximetry (ie, a noninvasive method used to estimate hemoglobin saturation with oxygen and pulse rate) and capnometry (ie, the determination of the end-tidal partial pressure of carbon dioxide, frequently with graphic representation) to assess ventilation, oxygenation, and tissue perfusion is highly recommended (Figure 3). This combination has the potential to greatly reduce more than 90% of avoidable anesthetic mishaps.2
For capnometry, the patient must be ventilating (either spontaneously or mechanically) and have sufficient cardiac output to return venous blood to the lungs for carbon dioxide removal. In normal patients, carbon dioxide levels at the very end of expiration (end-tidal) closely approximate gas tensions in the arterial blood.

Concurrent use of pulse oximetry (via a tongue probe) and capnometry in an anesthetized dog. Hemoglobin saturation is adequate at 100% with a pulse rate of 76 bpm. End-tidal carbon dioxide levels are slightly low at 33 mm Hg, with a respiratory rate of 9 bpm.
Pulse oximetry measures pulse rate and hemoglobin saturation (normal values, >95%). Similar to capnometry, pulse oximetry relies on cardiac output to generate an adequate signal. However, because hemoglobin saturation values are usually located far right on the flat part of the oxygen-hemoglobin dissociation curve, pulse oximetry is not always sensitive in detecting hypoxemia when administering 100% oxygen (eg, during inhalant anesthesia).
During induction and recovery, when inhaled oxygen levels are less than 100% (and are closer to room air, ~21%), pulse oximetry may quickly determine deficiencies in oxygenation because patients are closer to the sloped portion of the curve (ie, further to the left), where small changes in oxygenation greatly affect hemoglobin saturation.
3. The Ultrasonic Doppler Flow Detector is essential.
Adequate circulation and tissue perfusion are vital during anesthesia. The Ultrasonic Doppler Flow Detector (or Doppler) is a versatile, relatively inexpensive, and effective way to audibly assess peripheral blood flow, pulse rate, and blood pressure in many species (Figure 4). A piezoelectric crystal placed over a peripheral artery detects shifts in sound frequency as blood flows through and amplifies it into an audible signal.

Use of an audible Ultrasonic Doppler Flow Detector (gray box) on the tail of a pot-bellied pig. Note the concurrent use of the pulse oximeter (blue box) and noninvasive oscillometric monitor on the hind limb.
The anesthetist can assess pulse rate and signal quality as it changes over time. A pressure cuff and sphygmomanometer can be used to gauge approximate blood pressure: As the cuff is inflated, the flow becomes inaudible; as the cuff pressure is slowly released, the first audible signal is usually associated with the systolic blood pressure in most anesthetized dogs, but is closer to the mean blood pressure in anesthetized cats.3-5
To maintain organ perfusion and minimize complications associated with hypotension, mean blood pressures should be kept above 60–70 mm Hg. Because the assessment is real-time with minimal delay between readings, the anesthetist is quickly alerted to abrupt changes or even slowly developing trends in cardiovascular status, and he or she can intervene when appropriate.
4. An electrocardiogram detects only arrhythmias.
An electrocardiogram (ECG) measures and records the heart’s electrical activity but does not assess cardiac contractility; therefore, the ECG may continue to record complexes when there is no cardiac output. For example, pulseless electrical activity and non-pulsatile ventricular tachycardia will continue to show electrical activity on an ECG but are not associated with any peripheral pulses (Figure 5).

Pulseless electrical activity recorded in a dog in cardiopulmonary arrest. The top screen shows electrical activity recorded with a lead II ECG; however, the pulse oximeter (middle screen) does not reveal any pulsatile activity and the capnometer (bottom screen) suggests minimal carbon dioxide is returning to the lungs, with eventual apnea.
Also, many ECG monitors use an algorithm to calculate heart rate, so estimates are frequently inaccurate. An ECG should be used only to detect cardiac arrhythmias—not for pulse rate determination or assessment of blood flow, unless used concurrently with other monitors (eg, pulse oximetry, Doppler, direct arterial blood pressure).
5. Consider all the information.
Using all the available information to assess technique adequacy and quality, rather than looking at only one parameter, is most important for a successful anesthetic procedure. If too much emphasis is placed on one parameter, changes in depth or physiologic status may be missed, so using a combination of a hands-on approach with monitoring equipment is recommended. When difficulties arise, it is important for the anesthetist to collect his or her thoughts and not lose perspective of the complete picture. The anesthetic record can subsequently be used to visualize all monitored parameters simultaneously and detect trends impossible to see when focusing on just one time point or parameter.
Conclusion
Anesthetic monitoring has sometimes been referred to as “periods of boredom separated by episodes of panic.” If the above 5 tips are followed, the anesthetic period should be more predictable and less stressful for team members and provide better care for patients.
This article originally appeared in the March 2015 issue of Veterinary Team Brief.