Top 5 Tips on Radiographic Diagnosis of Obstructive Foreign Bodies
Nathalie Rademacher, Dr. med. vet., DECVDI, DACVR, Louisiana State University

Ileus can be functional or mechanical. In functional ileus, peristaltic contractions of the bowel cease as a result of vascular or neuromuscular abnormalities within the bowel wall, but the bowel remains patent. In mechanical ileus, physical obstruction occludes the lumen and can be caused by foreign bodies (FBs), intussusception, mural mass, or extraluminal lesions. GI FBs are a common cause of mechanical obstruction, which may be complete or partial. The jejunum is reported to be the most common location.1
The majority of obstructive GI FBs compromise the blood supply by luminal distention, leading to intestinal wall edema and progressive necrosis.1 Complete obstruction is associated with more dramatic clinical and radiographic signs, whereas partial obstruction may be associated with more chronic signs.2 Differentiation between mechanical and functional ileus may be impossible because of overlapping radiographic findings.
The following focuses on the detection of obstructive FBs and provides a few tips to improve detection of FBs on radiographs to make a diagnosis of mechanical ileus easier and support the decision for surgical exploration.
1. Use Radiographic Findings
Radiographic features of small intestinal mechanical obstruction depend on its completeness, location, and duration.2 Whereas metallic FBs or those with mineral content are easily recognized within the GI lumen (Figure 1), nonmineralized, nonmetallic objects (eg, cloth) within the GI tract are more difficult to identify (Figure 2). Some may be recognized by their geometric shape. The most consistent sign of mechanical obstruction is variable dilation of intestinal loops proximal (orad) to the obstruction (described as a mixed population of small intestine; Figure 2). Determination of small intestinal diameter can be made by comparing it to the L5 vertebral body height in dogs.3 Values greater than 1.6 are suggestive of obstruction (Figure 2A). In cats, a ratio of the maximum small intestinal diameter to vertebral end plate height of L2 greater than 4 indicates a high likelihood of intestinal obstruction.4

VD abdominal radiograph of a 1-year-old cat with a 2-day history of vomiting and a nonobstructing metallic foreign body. A coin with a radiolucent center caused by erosion is present within the small intestinal loops in the right midabdomen. No dilated loops of small intestine are seen to indicate mechanical obstruction.
Qualitative assessment of intestinal size by experienced clinicians may be as accurate in determining the presence of mechanical obstruction as calculation of ratios. Obstructed intestine usually contains fluid and gas; however, if the obstruction is orad, reflux into the stomach can occur and limited intestinal distension may be apparent. More distal (aborad) or more complete obstruction leads to greater dilation. Stacking of intestinal loops occurs with more severe dilation as segments become increasingly crowded in a relatively smaller space (Figure 2B).
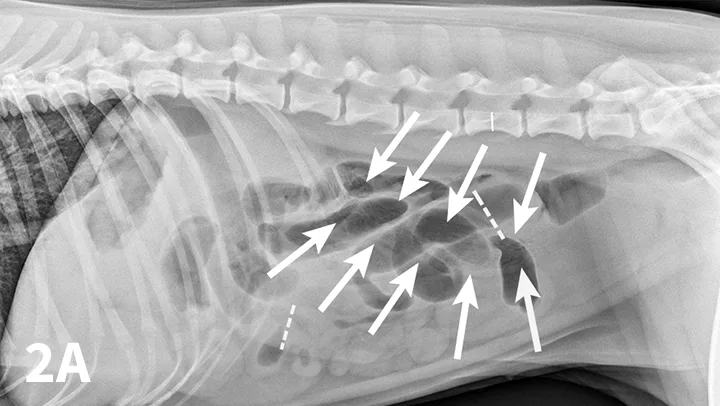
FIGURE 2
Right lateral (A) and VD (B) abdominal radiographs of a Labrador retriever with an obstructive ileus. A FB (sock) is present within a dilated small intestinal loop in the right caudoventral abdomen (arrows). The dashed lines outline a fluid-filled loop measuring 2.7 cm and a gas-filled loop measuring 2.4 cm, compared to the height of L5 (A; solid line, 1.1 cm); the resulting ratios of 2.4 and 2.2, respectively, are much greater than the upper limit of 1.6 for normal small intestine to L5 height ratio. Several stacked gas-filled loops of small intestine are present in the left midabdomen (B).
2. Repeat Abdominal Radiography 24 to 36 Hours After Fasting
Food or ingesta can look similar to foreign material and can be difficult to differentiate. Depending on the presentation, radiography can be repeated after fasting period to document passage (or lack thereof) of GI content (Figures 3 and 4). Persistence of opaque foreign material in the same location over a 24- to 48-hour period should increase the suspicion of partial obstruction. In cases of complete mechanical obstruction, radiographic features of obstruction can develop during this time. This makes it easier to recognize the obstruction radiographically (Figure 4C).

FIGURE 3A
Left lateral radiograph of a 4-year-old crossbreed dog with a history of vomiting. The patient was clinically stable. Granular, well-defined soft tissue opaque material is present within the fundus of the stomach, consistent with food or foreign material.
3. Use Positional Radiography
Right and left lateral abdominal radiographs are easy to obtain and are often helpful in cases of suspected GI FBs and obstruction because this positional change shifts the fluid and gas present into different areas, which might highlight potential intraluminal FBs (Figure 5). The main benefit of this simple technique is in the identification of pyloric FBs in cases of suspected pyloric outflow obstruction, but it is also useful in the small intestine, especially if duodenal FBs are suspected.


Left lateral radiograph (A) of a 4-year-old crossbreed dog with a 3-day history of vomiting and anorexia. An irregularly marginated, well-defined, soft tissue opaque structure (arrows) outlined by gas is present within the pylorus on the left lateral view. A right lateral radiograph of the same dog (B). The irregularly marginated, well-defined, soft tissue opaque structure displayed in Figure 5A is not clearly seen on the right lateral view because of the dependent distribution of fluid into the pyloric antrum silhouetting with the foreign body. This was confirmed to be cloth causing a gastric outflow obstruction.
4. Perform Pneumocolonography
Pneumocolonography is a rapid, safe, and relatively easy procedure that can be performed to identify the position of the colon when it cannot be determined on survey radiographs. Usually the colon is filled with feces and gas, which makes its position apparent. If, however, the colon is poorly visualized or confusing fluid or gas opacities are present, the colon can be easily localized by creation of pneumocolon.5
In cases of suspected FBs, this technique can be helpful to differentiate dilated small intestinal loops from colon or determine whether mottled mineralized material is in the colon or small intestinal tract. After initial survey radiographs are taken (Figures 6A and 6B), the animal is placed in lateral recumbency. Air is instilled into the rectum and colon using a large lubricated syringe or rubber catheter; approximately 10 to 12 mL/kg of air is needed for moderate distention of the colon.6,7 Standard lateral and ventrodorsal radiographs are then taken (Figures 6C and 6D). In most animals, it is desirable to fill the colon to the cecum. Partial filling of the distal jejunum and ileum may occur and is normal.

FIGURE 6A
Left lateral (A) and VD (B) survey radiographs of a 4-year-old pit bull terrier with a 3-day history of vomiting, diarrhea, and anorexia. A dilated loop of bowel is present within the midabdomen (star) caudal to the stomach, which could represent large or small bowel.
5. Conduct Compression Radiography
Compression radiography is a simple technique that may help clarify the presence of an obstruction.8
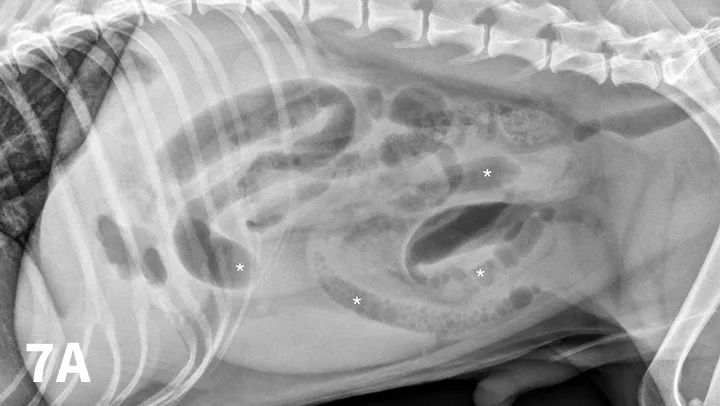
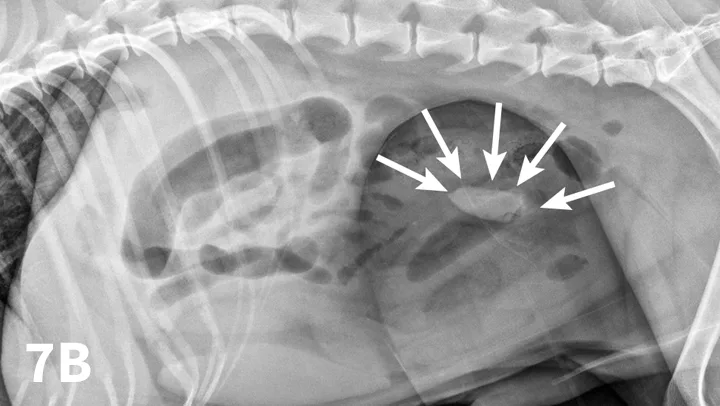
Left lateral radiograph of a 9-year-old Jack Russell terrier with a 4-day history of vomiting and anorexia (A). Moderate dilation with small gas bubbles (stars) of the small intestinal tract is noted (B). Left lateral compression radiograph of the same dog. A wooden spoon was used to apply compression to the caudal abdomen. Ventral to the colon, a well-defined ovoid mineral opacity (arrows) is visible within a dilated small intestinal loop. This was a piece of rubber confirmed at surgery.
With the patient in lateral recumbency and using a wooden or plastic spoon or paddle, the abdomen is mildly compressed in an area of concern identified on survey films (Figure 7A). Using the paddle and compression, adjacent bowel or masses are displaced to increase radiographic conspicuity. This results in better visualization of potential foreign material (Figure 7B), plication of small intestinal loops in cases of linear FBs, or intestinal masses otherwise obscured by superimposed bowel.