Top 5 Oral & Dental Lesions
Kevin Stepaniuk, DVM, DAVDC, University of Minnesota

Most patients hide signs of pain associated with dental infections. Disease in the oral cavity may manifest in small, yet obvious, lesions. Clinicians should be aware of the subtle signs that often present with oral or dental disease and indicate the need for further evaluation. Overlooking these common pathologies is a missed opportunity to provide care and treat infection and pain in patients. When a clinical lesion is identified, general anesthesia and intraoral radiographs are required to confirm diagnosis and develop a comprehensive treatment plan.1-3
1. Fractured teeth
Approximately 25% of dogs are presented with one or more fractured teeth, and 10% have a complicated crown fracture indicating the pulp canal is exposed (Figure 1).4-6 Once exposed to the oral cavity, the canal pulp becomes contaminated, infected, and necrotic, eventually resulting in periapical infection and pain. An oral examination of the patient while under general anesthesia can detect exposed canal pulp; a dental explorer will stick or drop into the open pulp. If open pulp is identified, intraoral radiographs are required to assess the periapical tissues (eg, periapical lucency, root resorption) and the size of the pulp canal (eg, may be wider compared to the contralateral tooth; Figure 2). Necessary treatment options for a pulp-exposed, infected tooth include root canal treatment or surgical extraction.

Left mandibular canine tooth root (tooth 304) that had a complicated crown fracture. A periapical lucency, external inflammatory apical root resorption, and a relatively widened pulp canal are present, indicating the tooth has been dead and infected for months. The chronically exposed pulp results in periapical infection and inflammation.
2. Parulis
A parulis is an opening of an intraoral sinus tract in the oral mucosa; hidden periodontal disease is often indicated if the parulis is within the gingiva (Figures 3 and 4). Periodontal disease is caused by a subgingival biofilm (an adherent bacterial community living in an exopolysaccharide matrix that protects the bacteria and allows cooperation of the microorganisms) that results in loss of attachment of the periodontium (ie, gingiva, alveolar bone, periodontal ligament, cementum), regardless of the amount of plaque or calculus on the supragingival crown. Periodontal disease is predominately a subgingival disease, so general anesthesia and intraoral radiographs are required. Extraction is often necessary for periodontal disease associated with a parulis. If the parulis is within the oral mucosa, it is likely caused by endodontic disease, and root canal treatment may be an option. A parulis at the mucogingival junction might be caused by either periodontal or endodontic disease.
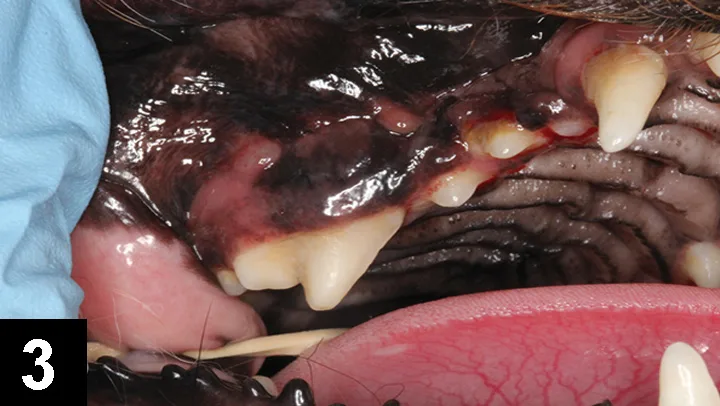
Parulides at the mucogingival junction of the right maxillary fourth premolar (tooth 108). Although the crown does not appear clinically fractured or to have significant plaque and calculus, the presence of the parulides indicates infection resulting in sinus draining tracts exiting in these regions. Intraoral radiographs are indicated.

Combined vertical and horizontal bone loss of the distal and buccal roots of tooth 108 from the patient in Figure 3, resulting in almost complete bone loss. The tooth has a wide pulp canal compared with other teeth, indicating the pulp in this tooth died a long time ago (combined periodontal–endodontic disease). Surgical extraction is the only option in this case. The pulp chambers in tooth 106 wider than the other teeth, indicating that the pulp in this tooth is also necrotic and requires extraction.
3. Tooth resorption
While tooth resorption is becoming increasingly common in dogs, feline tooth resorption affects 27% to 72% of all domestic cats.7-12 Cats rarely exhibit overt signs of oral pain associated with tooth resorption; however, tooth resorption may be so painful that patients may become hyporexic or anorexic, drop food, have exaggerated jaw movements, abruptly stop eating, and/or paw at the face while eating and drinking. Lesions start subgingivally, so subtle lesions at the free gingival margin (Figure 5) may be missed, particularly when on the lingual and palatal sides of the teeth. General anesthesia, full-mouth intraoral radiographs, and indicated treatment should be recommended.

Figure 5 Feline tooth resorption lesion located at the buccal gingival margin of the right mandibular canine tooth (tooth 404). Identification of this lesion at examination warrants full-mouth intraoral radiographs and treatment as indicated in this patient.
4. Maxillary draining tracts
A maxillary extraoral draining tract rostral to the eye is most commonly associated with chronic infection (periodontal or endodontic) of a maxillary premolar or molar tooth (Figure 6). In brachycephalic breeds, it might even be the canine tooth. Dental disease is subgingival, and both periodontal and endodontic infections can result in maxillary draining tracts. There may be associated bone proliferation or reaction, and the region may be firm on palpation. Dental disease should be the top differential for these lesions before dermatologic conditions, ophthalmologic conditions, or tumors are considered. The infected tooth can be identified with general anesthesia, oral examination, periodontal probing, and intraoral radiographs of the maxillary regional dentition on the ipsilateral side of the draining tract (Figures 7 and 8) with similar radiographs of the contralateral side for comparison. Surgical extraction of the infected tooth or teeth is often necessary. The carnassial tooth is not always at fault; therefore, intraoral radiographs are needed to diagnose the infected tooth, which could be any of the ipsilateral dentition (eg, first maxillary molar).
5. Stomatitis
Infectious or inflammatory conditions can cause inflammation of the gingiva and oral mucosa. Unfortunately, the termstomatitishas historically been and continues to be used loosely, blurring the discussion and treatment of inflammatory conditions in the feline oral cavity; the true definition of stomatitis is inflammation of the oral cavity.4Biopsy and histopathology findings of the oral cavity are often reported as variants of lymphoplasmacytic gingivitis, mucositis, or stomatitis, which implies chronic inflammation. The more common age-related periodontal disease and aggressive periodontitis, caused by subgingival plaque biofilms, should not be mistaken for the less common, true immune-dysregulated stomatitis (Figure 9).13,14 True immune-dysregulated stomatitis has a component of caudal mucositis. Corticosteroids and antibiotics are inappropriate for the treatment of periodontal bacterial-induced oral inflammation. General anesthesia, oral examination with periodontal probing, and full-mouth intraoral radiographs are necessary to differentiate periodontally inflamed tissue from true immune-dysregulated oral mucosa. Short- and long-term surgical and medical treatment plans are based on accurate diagnosis. Although stomatitis is often discussed in relation to feline patients, there are painful stomatitis conditions that also occur in the dog.

Caudal mucositis (inflammation in the caudal oral mucosa) consistent with a true immune-dysregulated stomatitis. In addition to the gingivitis and buccal mucositis, the caudal mucositis is a clinically distinguishing finding to help differentiate a true immune-dysregulated stomatitis from aggressive periodontitis-causing oral inflammation. Surgical and medical treatment plans and prognosis, both short- and long-term, depend on correct diagnosis.
Closing thoughts
Correct assessment of these clinical lesions requires general anesthesia, oral examination with periodontal probing, and intraoral radiographs. Patients often suffer quietly with hidden pain and infection, so clinicians need to identify these lesions, advocate for patient health, educate the client, and develop and recommend a treatment plan.