Top 5 Methods for Assessing Tooth Vitality
Kendall Taney, DVM, DAVDC, FAVD, Center for Veterinary Dentistry & Oral Surgery, Gaithersburg, Maryland

We sat down with Dr. Taney to discuss different treatment options for nonvital teeth. Listen to her episode of Clinician's Brief: The Podcast here.
When a tooth becomes nonvital, it can become a nidus for infection and, over time, can develop periapical pathology with tooth root abscessation at the end stage. Clinicians must be able to identify nonvital teeth to recommend appropriate treatment.
Following are the author’s top 5 methods for assessing tooth vitality.
1. Visual Inspection of the Crown of the Tooth
Visual inspection of the crown of the tooth allows the clinician to take note of any deviation from normal tooth color and any abnormalities in crown structure, whether congenital or acquired.
Enamel and/or dentin fractures can suggest that a tooth has been traumatized and may undergo irreversible pulpitis (Figure 1, above and Figure 2, below). Any tooth with a complicated crown fracture will become nonvital over time due to oral bacterial colonization of the pulp. Carious lesions can also irritate the pulp and cause pulpitis.
Extrinsic staining is limited to tooth enamel and can typically be removed via scaling and polishing. Intrinsic staining occurs in the dentin, can be systemic or localized, and may indicate a nonvital tooth. A common cause of localized intrinsic staining is intrapulpal hemorrhage with necrosis that occurs when a tooth is traumatized.1 The byproducts of hemorrhage can penetrate the dentin tubules and cause discoloration of the dentin. The discoloration can change over time as the byproducts break down in the tubules. Teeth can initially appear pink to purple and can eventually become gray (Figure 3). Intrinsic staining from hemorrhage or necrosis indicates that significant trauma to the pulp has occurred and pulpitis is or was present.
The shape of the crown and/or root can also give insight into any developmental abnormalities of the tooth that can potentially affect vitality (Figures 4 and 5).

Figure 2
Uncomplicated chip fracture of the right mandibular canine tooth. The tooth has been traumatized and should be monitored for signs of pulpitis. A dental explorer would not be able to enter the pulp chamber for this type of fracture.
2. Sensibility & Vitality Testing
Sensibility testing is not particularly reliable in animals, as it typically relies on verbal communication. The 2 most common types of sensibility testing in humans are thermal testing and electrostimulation. Sensibility tests are more indicative of nerve conduction and do not prove that a tooth is vital with a healthy blood supply.
Vitality testing assesses the vascular supply of a tooth and is a more reliable indicator of pulpal health as compared with sensibility testing. Most vitality testing modalities are limited in veterinary clinical practice due to cost and time constraints.2 Examples of diagnostic methods to assess the vascularity of the pulp include laser Doppler flowmetry, dual wavelength spectrophotometry, and pulse oximetry (Figure 6). Pulse oximetry is not limited by cost and time constraints and is widely used in veterinary medicine. Pulse oximetry of the teeth has been evaluated in one veterinary study but was only tested on vital teeth.3 Further veterinary studies are needed to determine the accuracy of vitality testing via pulse oximetry.

Pulse oximeter application on a canine tooth to check for vitality
3. Dental Radiography
Dental radiography can be used to evaluate tooth structure anomalies and root pathology and to assess pulp canal size. Assessment of pulp canal size can be particularly useful for diagnosing nonvital teeth. A common misconception is that after a tooth dies, the canal becomes uniformly wider. In reality, the canal appears wider as compared with other canals because it stopped producing dentin at the time it became nonvital (Figure 7). Vital teeth with intact pulp have odontoblasts that will continue to produce secondary dentin, causing the pulp chamber to continue to narrow.4 Presence of periapical lucencies (Figure 8) and root resorption on dental radiographs are other indicators that a tooth is nonvital.
If the insult to the tooth happened recently, the pulp chamber size will be the same as the contralateral tooth. Repeat radiographs in 6 months may show that the pulp chambers of vital teeth will continue to narrow and the nonvital tooth pulp chamber will appear larger. Of note, it can be difficult to evaluate subtle changes in canal size in mature dogs with narrow canals.
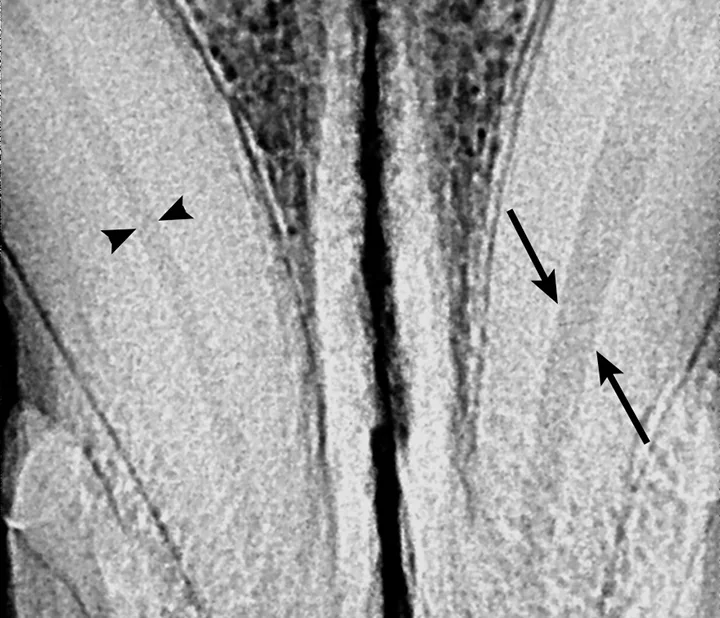
Figure 7
The pulp chamber of the left mandibular canine (arrows) is significantly wider than the right (arrowheads), indicating that the pulp is no longer producing secondary dentin and is nonvital. Although this is a definitive sign of nonvitality, its absence does not confirm vitality.
4. Direct Examination of the Pulp
Definitive confirmation of tooth vitality is not always possible. Clinicians must use the appropriate tools and observations to make a clinical diagnosis and treat the tooth accordingly. Deliberate exposure of the pulp for visual inspection (Figure 9) is not recommended for determining tooth vitality, as this would predispose the tooth to bacterial contamination and necessitate a subsequent endodontic or exodontic procedure. If treatment of the tooth is planned, the pulp characteristics can be noted at that time to confirm the clinical diagnosis.

Observation of a bleeding pulp in a recently fractured tooth could indicate vitality but cannot predict if the pulp will survive the insult.
5. Histopathologic Evaluation
Histopathology of the pulp should be the gold standard in determining pulp vitality. However, it is not a practical step, as it requires removal of the pulp from the tooth, which would cause the remaining pulp to become nonvital. If confirmation at the time of treatment is desired, the pulp can be removed from the endodontically or exodontically treated tooth and submitted for evaluation.
Conclusion
Pulpitis can be reversible (ie, the pulp is able to recover from the insult) or irreversible, which results in pulp death. The hard tissue of the tooth that encases the pulp can hinder the ability of the pulp to recover from pulpitis, especially in older patients.5 A single canine study evaluating teeth with localized intrinsic staining found that 59 out of 64 teeth evaluated had either partial or total pulp necrosis.6 Monitoring of a tooth is appropriate in some cases, such as a recently traumatized tooth with an intact crown. Monitoring of vitality can be achieved with serial dental radiography at regular intervals to evaluate for root canal size and development of periapical pathology. If a tooth is determined to be nonvital, treatment is indicated by either endodontic or exodontic methods. Teeth in patients younger than 2 years have a higher chance for recovery from trauma due to the larger size and high cellularity of the pulp, which may allow for repair from trauma. Older patients may be more prone to permanent pulpal damage after trauma because of loss of reserve cell capacity.4