Top 5 Lip Depigmentation Causes in Dogs
Alexander Werner Resnick, VMD, DACVD, Animal Dermatology Center

Skin pigmentation in mammals is primarily produced by the transfer of eumelanin (ie, black–brown pigment) and pheomelanin (ie, yellow–red pigment) within melanosomes through the dendritic processes of melanocytes to adjacent keratinocytes in the basal cell layer.1 In dogs, the dendritic processes of one melanocyte are associated with 10 to 20 keratinocytes to produce the epidermal melanin unit.2
Because of the cytotoxicity of synthesis intermediates, melanogenesis is confined within melanocytes to the membrane-bound melanosomes.2 Abnormal loss or absence of pigmentation (ie, leukoderma or hypomelanosis, respectively) can be caused by reduced pigment production and/or loss of melanocytes.
The lip margin in dogs is highly visible and often darkly pigmented. Both the degree and pattern of normal pigmentation differ by breed type and individual dog. Thus, determining whether pigmentation changes suggest a pathologic process must be based on what is normal or abnormal for each dog and on the presence or absence of inflammation and/or pigmentation changes at other locations. In general, acute inflammation often produces depigmentation, whereas chronic inflammation may lead to hyperpigmentation.
Following are the author’s top 5 causes of lip depigmentation in dogs.
1. Mucocutaneous Pyoderma
Mucocutaneous pyoderma is an inflammatory dermatitis that primarily affects the lip margins and perioral skin. Lesions are distinctive and typically consist of swelling of the lips, most notably at the commissures and lip folds, that progresses first to crusting and exudation then to focal erosions and ulcerations (Figure 1).3 Localized depigmentation is a common sequela. Intertrigo (ie, when one skin area comes in contact with other skin areas) causes inflammation as well as accumulation of moisture and debris. Lip fold intertrigo is often associated with development of mucocutaneous pyoderma (Figure 2); infection may also result from chronic excoriation caused by allergic reaction. Significant malodor, frequently mistaken as halitosis, and tenderness of infected tissues may be present.

Mucocutaneous pyoderma affecting the lip margins of a 13-year-old neutered male crossbreed Chihuahua. Adherent crusts can be seen overlying mildly eroded skin on the lower lip margin (arrows) and are most severe around the lip fold (arrowhead).

Mucocutaneous pyoderma causing erosions at the lip folds, with secondary depigmentation of the lip margins in a 4-year-old spayed Maltese
Diagnosis is made by excluding other dermatoses associated with depigmentation and by finding large numbers of bacteria in epidermal exudates. Culture and susceptibility testing is indicated in patients that fail to respond to treatment with a first-choice antibiotic.4 Initial treatment includes gentle clipping and cleaning of the lip margins. Application of a topical antiseptic or antibiotic can be sufficient, but oral antibiotic therapy may be required in severe or chronic cases. Recurrence is best prevented through regular cleaning of affected areas and correction of any secondary cause (eg, allergy, damage from excessive chewing).
2. Discoid Lupus Erythematosus
Discoid lupus erythematosus (DLE), more specifically facial-predominant DLE, is a common but usually mild variant of cutaneous lupus erythematosus.5,6 Many factors, including genetic and environmental triggers, are believed to influence the development of autoimmunity in patients with DLE. Lesions often worsen with sun exposure.
Deposition of autoantibodies and complement at the epidermal basement membrane zone results in lymphocytic lichenoid-interface dermatitis, with keratinocyte apoptosis, loss of melanosomes from melanocytes (ie, pigmentary incontinence), and reduced melanin production.7 Whereas depigmentation occurs secondary to inflammation in other conditions, loss of pigmentation is an initial sign of DLE. In these patients, the nasal planum is the primary location of lesions; however, diffuse-to-patchy lightening of the pigmentation around the lip margins occurs in most cases (Figure 3).

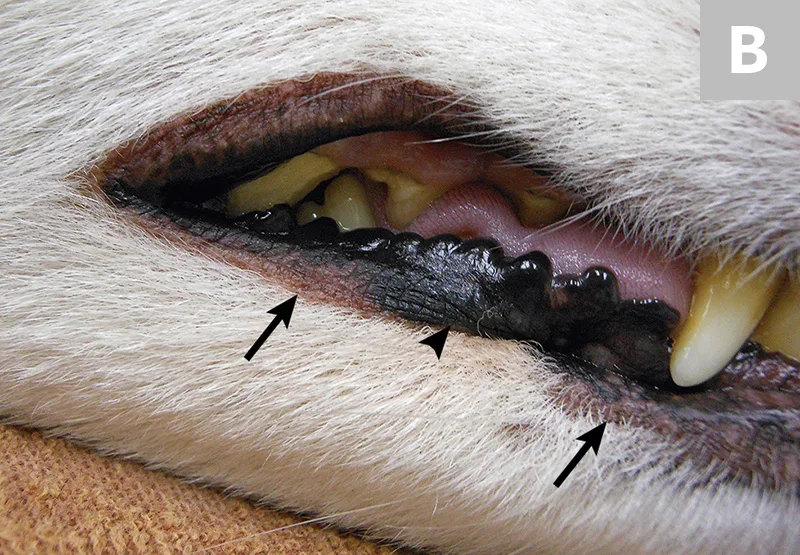
Significant depigmentation with loss of cobblestone-like appearance and crusting of the nasal planum in a 9-year-old neutered male American Eskimo dog with discoid lupus erythematosus. Mottled depigmentation of the adjacent skin is also present (A). Regions of depigmentation (B; arrows) adjacent to normally pigmented skin (arrowhead) are evident on the lip margins.
Diagnosis requires biopsy with histologic confirmation. Treatment primarily consists of sun avoidance and administration of topical corticosteroids or tetracycline-derivative antibiotics (eg, doxycycline [10 mg/kg PO q24h], minocycline [5 mg/kg PO q12h]) combined with niacinamide (250 mg PO q12-24h in dogs weighing <22 lb [10 kg] and 500 mg PO q12-24h in dogs weighing >22 lb [10 kg]).8 Long-term treatment with oral corticosteroids or immunosuppressive therapy is rarely required.
3. Epitheliotropic Lymphoma
Epitheliotropic lymphoma is an uncommon cutaneous neoplasia of older animals. In dogs, this disease is commonly associated with infiltration by CD8+ cells, whereas in humans, disease most often results from infiltration by CD4+ cells.9 Studies have suggested a 12-fold increased risk in patients with chronic atopy.10 The mucocutaneous form is often mistaken for other causes of inflammation around the lip margins and oral cavity; depigmentation is often associated with intense inflammation (Figure 4).

Diffuse depigmentation on the lip margins and nasal planum of a 9-year-old neutered male shih tzu with epitheliotropic lymphoma
Diagnosis requires biopsy with histologic confirmation. Overall prognosis is poor except when a lesion or lesions are identified early in disease and excised. Referral to a veterinary oncologist or dermatologist for treatment is advised.
4. Vitiligo
Vitiligo is an acquired, possibly immune-mediated, disease associated with melanocyte destruction. There may be a genetic basis for increased melanocyte susceptibility to damage as well as increased risk for developing antimelanocyte antibodies. Vitiligo has an increased incidence in certain breeds (ie, rottweilers, Old English sheepdogs).11,12 Striking depigmented patches can develop on multiple areas of the body (Figures 5 and 6). Lesions are distinctive and are not typically associated with inflammation. Both skin (leukoderma) and hair (leukotrichia) may be affected. Systemic signs are absent.

Vitiligo producing noninflammatory, well demarcated patches of depigmentation on the lip margins of a 3-year-old spayed Airedale terrier. Similar changes affect the nasal planum. Unlike lesions in patients with mucocutaneous pyoderma and discoid lupus erythematosus, inflammation and crusting are not associated with depigmentation.

Discrete, strikingly depigmented patches of vitiligo and leukotrichia affecting the lip margins, muzzle, and nasal planum of an adult crossbreed German shepherd dog
Diagnosis requires biopsy with histopathologic examination to exclude inflammatory causes of depigmentation. No effective treatment has been reported, and lesions may spontaneously regain pigmentation.
5. Uveodermatologic Syndrome
Similar to Vogt-Koyanagi-Harada disease in humans, uveodermatologic syndrome (often called Vogt-Koyanagi-Harada–like syndrome) is a multisystem autoimmune disease that affects pigmented tissues of the eye, ear, nervous system, skin, and hair.13,14 The syndrome is seen most often in young adult to middle-aged Akitas, Samoyeds, and Siberian huskies.13 Bilateral acute-onset painful uveitis is typically the first and most severe sign. Skin and hair coat depigmentation are secondary but occasionally can be concurrent. Skin lesions consist of whitening of the face, muzzle, and hair coat, with less frequent generalization. Erythema and erosions are uncommon but can occur (Figure 7).

Severe lesions of erosion and depigmentation in a 1-year-old neutered male Akita with uveodermatologic syndrome. On presentation, uveitis had progressed to permanent blindness.
Diagnosis is often made by ophthalmologic examination correlating with the cutaneous signs mentioned previously. Biopsy sampling with histopathologic examination is recommended in patients that lack active ocular signs. Aggressive, rapid initiation of immunosuppressive therapy is recommended to prevent formation of posterior synechiae and secondary glaucoma, cataracts, or blindness; prognosis is fair to good for patients appropriately treated.13,15
Conclusion
In patients with pigmentation disorders, the most important determination to make is whether loss of pigmentation developed before, after, or concurrently with inflammation (or absence of inflammation). Mucocutaneous pyoderma and epitheliotropic lymphoma can cause depigmentation secondary to intense inflammation but will rarely cause leukotrichia. In patients with DLE, depigmentation precedes inflammation and does not cause leukotrichia. In those with uveodermatologic syndrome, depigmentation of the skin and hair coat typically follows uveitis and is often associated with minimal inflammation of the skin. Vitiligo is rarely inflammatory. Patients with mucocutaneous pyoderma should respond to appropriate antibacterial therapy; for patients with lip depigmentation that fail to respond to antibacterial therapy, biopsy and histopathologic examination are required to determine the cause and to formulate an appropriate treatment plan.