Top 5 Cytologic Findings in Aspirates of Enlarged Lymph Nodes
Lisa M. Pohlman, DVM, MS, DACVP, Kansas State University

Lymph node enlargement is a common physical examination finding. Fine-needle aspiration with cytology is a fast, noninvasive, and relatively inexpensive means of classifying the cause of enlargement.
To cytologically identify the cause of abnormal or enlarged lymph nodes, clinicians must understand the cell populations that comprise normal lymph nodes (Figure 1); however, it is relatively rare to view a normal node on cytology, as normal nodes are often difficult to palpate, making aspiration difficult. Cytologically, approximately 85% to 90% of a normal lymph node is composed of small lymphocytes,1,2 which are approximately 1 to 1.5 times the size of an RBC. Small lymphocytes have rounded nuclei with dense, dark-staining chromatin and have scant blue cytoplasm. The remaining 10% to 15% of cells in a normal lymph node include mostly medium (ie, nucleus 2-2.5× the diameter of an RBC) and large (ie, nucleus ≥3× the size of an RBC) lymphocytes, both of which have a fine, lightly staining chromatin pattern. Occasional plasma cells and macrophages and rare mast cells, neutrophils, and eosinophils may also be seen in a normal lymph node.2 Varying numbers of cytoplasmic fragments (ie, lymphoglandular bodies) that originate from ruptured lymphocytes are also a typical finding in both normal and abnormal lymph node cytology.1 Morphologic descriptions are based on staining with Romanowsky-type stains (eg, Wright’s, Diff-Quik).
Following are 5 cytodiagnostic groups that should be considered in the evaluation of an aspirate of an enlarged node, according to the author.
1. Reactive or Hyperplastic Node
Reactive lymphoid hyperplasia occurs when antigens in high concentrations reach the draining lymph node and stimulate the immune system.2 As in a normal node, small lymphocytes still predominate cytologically, but an increase—typically constituting 15% to 25% of the cell population—in medium and large lymphocytes, plasma cells, ± both Mott cells (ie, plasma cells that contain packets of immunoglobulin [ie, Russell bodies]) and scattered mast cells can be expected (Figure 2). Macrophages may be mildly increased. Neutrophils and eosinophils are rare. Morphologically normal mitotic figures may occasionally be seen.1
An enlarged lymph node may sometimes have cytologic features more consistent with a normal node without the reactive components (eg, increased concentration of medium and large lymphocytes and plasma cells). In such cases, it is important to recognize that the node is enlarged and interpret the cytologic findings together with the node’s size. The interpretation may simply be lymphoid hyperplasia, but, in the author’s experience, there has been no clearly defined agreement among clinical pathologists on terminology (ie, lymphoid hyperplasia vs reactive lymphoid hyperplasia). Differentiation in terminology, however, is of little utility, as both cause lymph node enlargement due to local or systemic antigenic stimulation and/or response (eg, inflammation, infection, neoplasia, immune-mediated disease).1,2
In reactive or hyperplastic nodes, the overall impression from a low-power view of a cytologic sample should be a heterogeneous population of predominantly lymphoid cells, most of which are small (Figure 3).
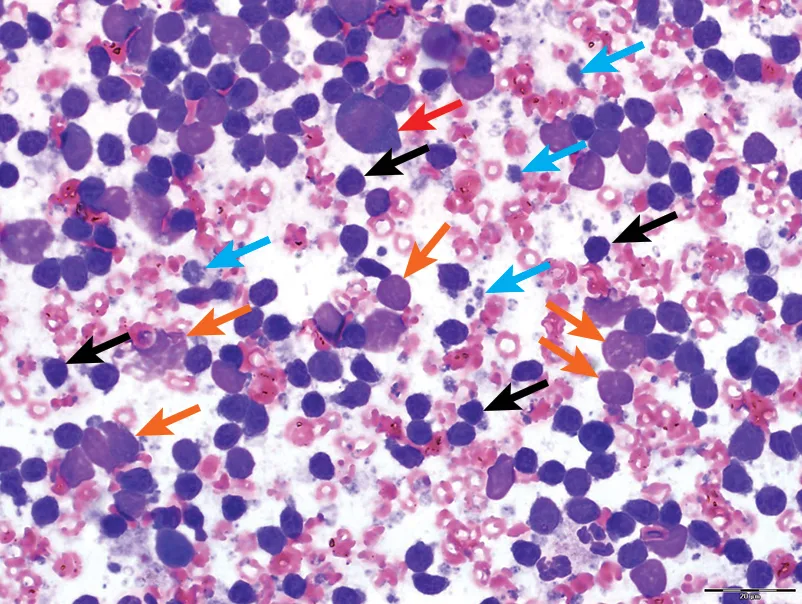
FIGURE 1
Normal lymph node. The predominance of small lymphocytes (black arrows) can be observed. A large lymphocyte (red arrow), nuclear remnants (orange arrows), and cytoplasmic fragments from ruptured cells (blue arrows) are among a background of crenated and poorly preserved RBCs. Modified Wright’s stain; 600× magnification
2. Lymphoma
Cytology is often sufficient for confirming a diagnosis of lymphoma. A homogeneous, monomorphic population of medium and/or large lymphocytes is the most common key cytologic feature of most lymphomas in dogs and cats (Figure 4).1,2 A diagnosis of lymphoma can be made when the medium and/or large lymphocytes comprise the vast majority of the cell population in an array of well-made, highly cellular cytologic smears that represent sampling from an entire lymph node or multiple nodes.1,2 Although lymphoma is often a relatively straightforward diagnosis on cytology, prognostic information should be obtained after cytology through immunophenotyping and/or histopathology for specific classification of the disease process. In addition, some types of lymphoma (eg, small-cell variant, T-cell–rich, large B-cell) are more difficult to diagnose via cytology, so histopathology or PCR for antigen receptor rearrangement may be required to confirm diagnosis.
3. Lymphadenitis
Lymphadenitis is characterized by an accumulation of inflammatory cells in the lymph node and is classified as either neutrophilic, eosinophilic, or histiocytic, depending on the type of cell(s) present.
Neutrophilic lymphadenitis is present if neutrophils comprise an estimated >5% of cells in the absence of blood contamination.2 Neutrophilic lymphadenitis may be associated with immune-mediated disease, neoplasia, and/or bacterial or fungal infection; fungal infection is also typically associated with the presence of macrophages.2
Eosinophilic lymphadenitis is present if, in the absence of blood contamination, >3% of nucleated cells are eosinophils.2 Eosinophilic lymphadenitis is most commonly associated with hypersensitivity and/or parasitic infection (eg, flea bite allergy; Figure 5) but may also be seen with other conditions, such as some neoplasms (eg, mast cell tumor, lymphoma, carcinoma), hypereosinophilic syndrome, or GI eosinophilic sclerosing fibroplasia.
Histiocytic lymphadenitis is present if there is a moderate increase in macrophages in the node and/or if multinucleated giant cells and/or epithelioid macrophages are among the histiocytic population. Conditions associated with histiocytic lymphadenitis include fungal infection, mycobacteriosis, salmon poisoning disease, protothecosis, pythiosis, and hemosiderosis, among others.2
Multiple inflammatory cell types may be present in some cases (eg, neutrophilic and eosinophilic lymphadenitis [Figure 6], neutrophilic and histiocytic [ie, pyogranulomatous] lymphadenitis).
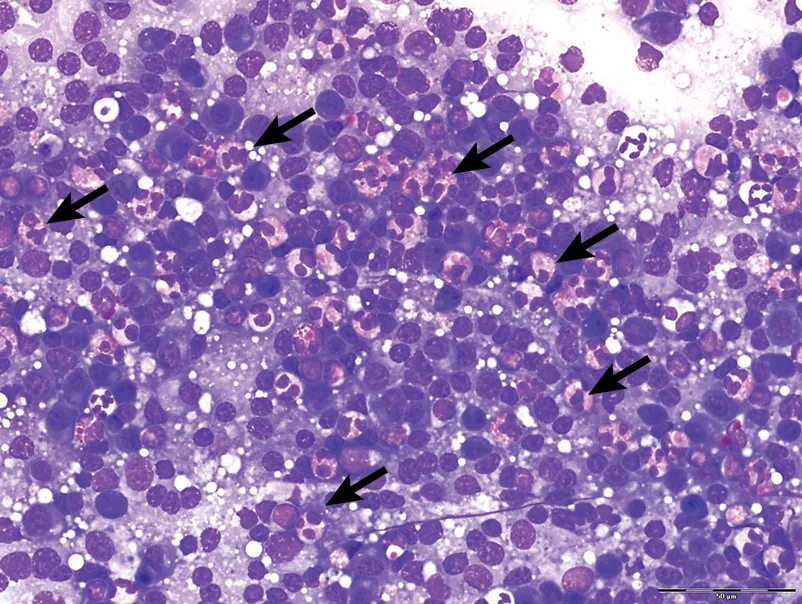
FIGURE 5
Eosinophilic lymphadenitis in a dog with heartworm disease. A few of the many eosinophils are indicated by the arrows. Modified Wright’s stain; 600× magnification
4. Metastatic Disease
A marked increase in cells expected in a lymph node (eg, mast cells) or the presence of cells not expected in a lymph node (eg, epithelial cells) may be indicative of metastatic disease,1 particularly if features of malignancy are present in the cell population in question.
Carcinomas frequently metastasize to lymph nodes (Figure 7). Malignant epithelial cells often appear in large sheets or individually in a node. Epithelial cells should not be present in a lymph node and should raise suspicion for metastatic disease when observed in a correctly collected sample.1,2 Tonsils, however, are an exception to this, as squamous epithelial cells are occasionally observed in aspirates.3
Malignant melanomas commonly metastasize to lymph nodes; however, a diagnosis of metastatic melanoma must be based on the presence of neoplastic melanocytes—not the presence of pigment (eg, carbon, bile, hemosiderin, melanin), melanophages, or siderophages in the node.1 Mast cell tumors also commonly metastasize to lymph nodes; however, caution must be exercised when assessing the significance of mast cells in lymph nodes, as mast cells are occasionally seen in a normal node and are often increased in number in reactive nodes.1,2 The presence of large groups or sheets of mast cells or of poorly differentiated mast cells in a lymph node is more indicative of metastatic disease as compared with the presence of increased numbers of morphologically normal mast cells.1
5. Accidental Salivary Gland Aspirate
The submandibular lymph node and salivary gland are in close proximity2; thus, it is common for clinical pathologists to receive salivary gland cytology submitted as a lymph node aspirate2 or to occasionally identify epithelial cells from the salivary gland in a lymph node aspirate (Figure 8).1 It is crucial that clinicians are able to differentiate these cells and do not confuse them with malignancy.1 Normal salivary gland cytology contains individualized, cohesive clusters of secretory epithelial cells that have small, round, dark purple nuclei and foamy cytoplasm. Eosinophilic mucus is often present and can result in a windrowing effect (ie, lining up of cells) secondary to the viscous nature of the sample.1,2