Top 5 Complications of Tooth Extractions
Kendall Taney, DVM, DAVDC, FAVD, Center for Veterinary Dentistry & Oral Surgery, Gaithersburg, Maryland
Because of the prevalence of periodontal disease in companion animals, tooth extraction is commonly performed in veterinary medicine.1 Complications from tooth extractions can arise and may significantly increase anesthesia time and morbidity in patients2; an awareness of the causes of such complications can help prevent them.
Following are the author’s 5 most common tooth extraction complications.
1. Root Breakage
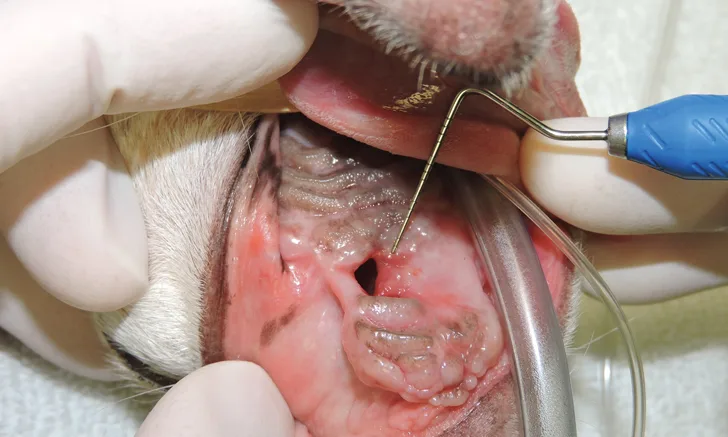
Mucoperiosteal flaps should be developed for most extractions to allow for appropriate exposure for alveolar bone removal, which allows for better visualization and subsequent tooth root elevation.2-4 As a general rule, buccal alveolar bone should be removed before elevation is attempted to expose, at minimum, approximately half of the root.5 A small bur can be used to create a mesial and distal space to allow for placement of a dental elevator. Tooth root elevation is a slow process that fatigues the periodontal ligament; if abrupt force is applied before the periodontal ligament is fatigued or severed, the root often fractures (Figure 1). Adequately exposing soft and hard tissues at the beginning of the procedure can save time and allow for successful root removal; however, even if careful and appropriate techniques are used, roots may still break during extraction (eg, due to tooth resorption or ankylosis of the root to the alveolus). If a root breaks, additional removal of alveolar bone is often necessary to retrieve the remaining root fragment.
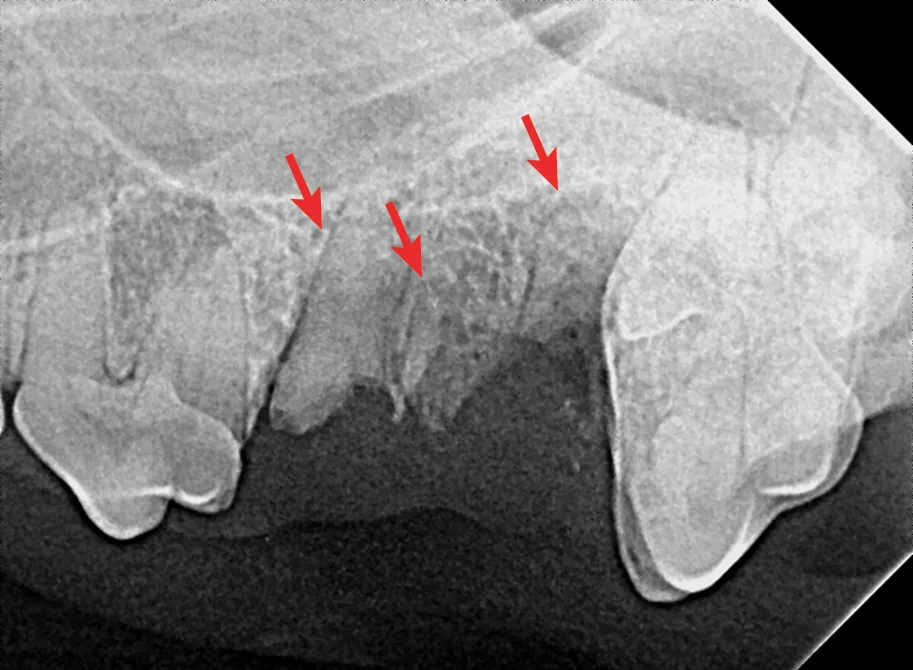
Fracture of the mesiobuccal and distal roots (arrows) during extraction of the left maxillary 4th premolar tooth in a dog
2. Root Tip in Nasal Cavity & Mandibular Canal
A potential sequela of root breakage is root tip protrusion into the nasal cavity (Figure 2) or mandibular canal (Figure 3),6 which, as with root breakage, can be caused by inadequate exposure or bone removal. In cases of root breakage, it is important to determine the location of the root tip and assess bone quality via dental radiography. If there is significant bone loss, a root fragment may be pushed through the apical extent of the alveolus and into an area that makes retrieval challenging. If this complication occurs and the root tip cannot be easily located, closing the extraction site and referring to a dental specialist is recommended.

FIGURE 2 Right maxillary premolar tooth root in the nasal cavity (A; circle) and root fragment after removal from the nasal cavity (B)
Root removal from the nasal cavity can be especially difficult because of the large size of the nasal cavity and the potential for tooth root migration. Large mucoperiosteal flaps, bone windows, and suction can aid in the removal process. Avoiding the mandibular neurovascular structures when removing roots from the mandibular canal can be challenging but is crucial, as hemorrhage can occur if structures are punctured.
3. Hemorrhage
The oral cavity has a rich blood supply from many vascular structures. Bone removal and development of mucoperiosteal flaps for extractions may expose major blood vessels (eg, branches of the maxillary artery [infraorbital in the maxilla and inferior alveolar in the mandible]). Damage to these vascular structures can result in significant hemorrhage (Figure 4A).
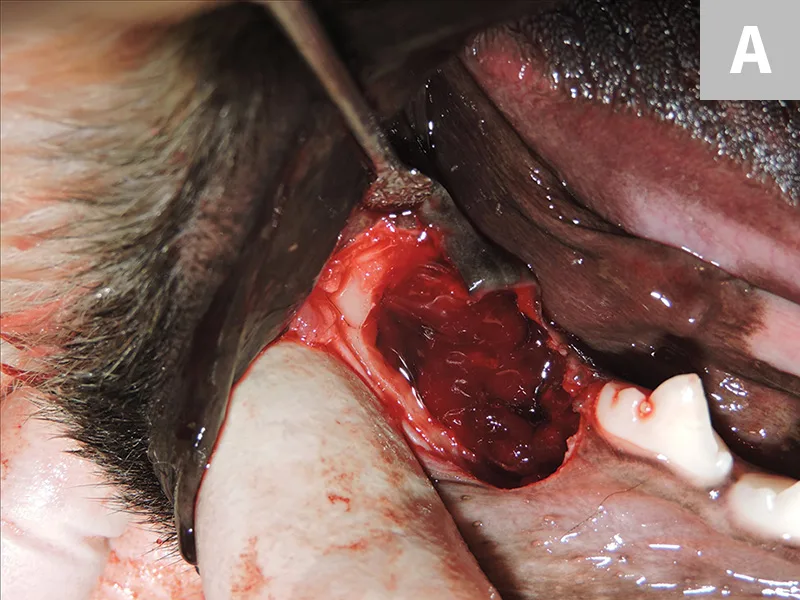

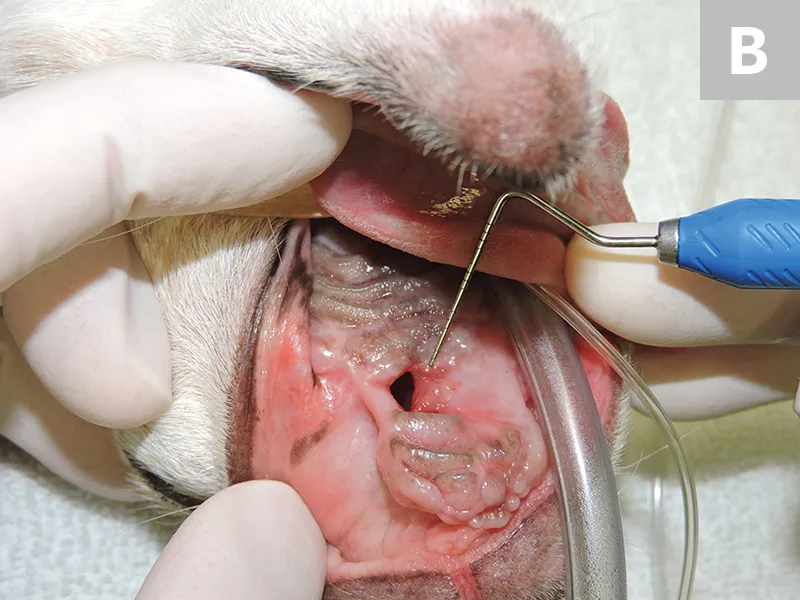
Hemorrhage of the mandibular artery during extraction of an impacted mandibular first molar tooth (A). Postcauterization of the mandibular artery (B); the mandibular canal is visible and was close to the roots of the impacted first molar tooth.
Inflamed tissues are a hallmark of active periodontal disease and are prone to heavier bleeding as compared with normal tissues.1 If a major vessel is damaged, procedures to control hemorrhage (ie, direct pressure, ligation, cauterizing, topical hemostatic agents) should be instituted (Figure 4B). In general, there are no major long-term complications of complete ligation of major vessels such as the maxillary and mandibular arteries. The high vascularity of the oral cavity ensures collateral circulation will be available to maintain vitality of the soft and hard tissues7; the only exception to this is damage to vessels that provide major blood supply to mucoperiosteal flaps. For example, damage to the greater palatine artery can lead to failure of a hard palate flap used to close a large defect.8,9
4. Dehiscence & Fistula Formation
When operating in the oral cavity, general surgical principles should be applied to avoid dehiscence and/or formation of an oronasal fistula (Figure 5A). A common cause of oronasal fistula formation is extraction of a diseased maxillary canine tooth without a mucoperiosteal flap. Even if the canine tooth was diseased and easily extracted, flap closure of the extraction site is still indicated. Gentle tissue handling, tension-free closure, and a healthy environment for healing are essential to prevent flap failure at the surgical site. Adequate blood supply in the mouth is generally not an issue, but debridement of diseased bone and soft tissue are important to encourage rapid healing.

Oronasal fistula formation in a dog after extraction of the left maxillary canine tooth (A); closure of the defect was achieved with a single mucoperiosteal flap after debridement of the mature epithelium at the fistula edges. Chronic/recurrent oronasal fistula in a small-breed dog (B); closure of this defect required more advanced flap repair techniques.
Most surgical wounds in the oral cavity heal rapidly (ie, in 10-14 days). Appropriate suture materials and patterns should be selected; absorbable suture materials are recommended to avoid the need for suture removal posthealing. The sutures will need to remain intact for the healing period of 14 days, which is typically not an issue for most available absorbable suture materials. If the extraction site has not healed after 14 days or an oronasal fistula has formed, the patient should be reevaluated under anesthesia to assess the need for biopsy and/or culture and susceptibility testing to rule out neoplasia or osteomyelitis as a cause of dehiscence.
A single, well-developed mucoperiosteal flap may be all that is required to close an oronasal fistula after debridement of the fistula edges. For more challenging cases or recurrent fistulas, a double-flap or other advanced technique by a dental specialist may be needed (Figure 5B).10-13
5. Iatrogenic Jaw Fracture
Dental radiography can provide information (eg, bone quality, root structure, pathology) that can help avoid iatrogenic jaw fracture (Figure 6A). Many patients with severe periodontal disease will have significant bone loss (Figure 6B) but teeth that are still well anchored in the alveolar bone. Tooth resorption and ankylosis provide further obstacles to successful extraction. The mandibular canine and mandibular first molar are the most common locations for iatrogenic jaw fracture.3,4

FIGURE 6 Iatrogenic fracture of the left rostral mandible after extraction of the left mandibular canine tooth (A; arrows). Same patient with iatrogenic jaw fracture after extraction (B); significant bone loss from periodontal disease was present, which contributed to this complication. Dilacerated root of the left mandibular first molar in a small-breed dog (C). The first molar in these breeds is often very large as compared with the width of the mandible. The hook on the mesial root can make extraction more challenging.
Small-breed dogs have a high first molar:mandibular height ratio, which increases the risk for fracture in cases of periodontal disease.14 In such cases, the roots can also be dilacerated (ie, there is an abnormal bend, hook, or overall shape to the root[s]); the tooth may have significant bone loss and appear to be an easy extraction, but the hook on the end of the root tip often makes removal much more difficult (Figure 6C).
For most patients, prognosis after iatrogenic jaw fracture is good. Complete recovery can be expected with appropriate reduction and stabilization.15
Conclusion
Owners should be made aware of the specific types of complications that may be encountered with tooth extraction. Patients with significant periodontal disease may be at increased risk, and owners should be informed before the procedure that complications, some of which could warrant referral to a boarded veterinary dental specialist, may arise. The scenarios presented here provide the more common complications that may be encountered and can provide clinicians talking points to discuss with owners to establish appropriate informed consent. With open and honest communication between the owner and veterinarian, these difficult situations can be handled with the patient’s best interest in mind.