Top 5 Complications of Gonadectomy
Karen M. Tobias, DVM, MS, DACVS, University of Tennessee
Gonadectomy (ie, ovariohysterectomy [OHE] or neutering) is one of the most commonly performed veterinary surgical procedures.1-6 Gonadectomy reduces pet overpopulation and euthanasia in animal shelters and decreases the risk for gonadal tumors, mammary neoplasia and pyometra in dams and queens, and perianal adenomas and benign prostatic hyperplasia in male dogs.7 It may also increase longevity and reduce hormonally driven behavior.7
Although gonadectomy is considered a routine procedure, complications can arise. Following are 5 of the most common complications of gonadectomy according to the author.
1. Incisional Complications
Incisional inflammation is an expected effect of any surgery and typically resolves without treatment8; incisional complications, however, occur less frequently1 and are likely underreported, as clinicians may not closely evaluate the incision line after anesthetic recovery or may not record findings they consider expected, minor, or self-limiting. Incisional complications associated with gonadectomy can include incisional and/or scrotal swelling, pain, redness, seromas, hernias, peri-incisional dermatitis, and skin bruising and generally occur more frequently in dogs >50 lb (22.7 kg) and in cats.4,9-11
Incision location may affect complication rates. For example, in a study of kittens undergoing OHE, incisional complications occurred more commonly with a midline approach as compared with a flank approach.12 In a study of dogs, prescrotal neuters resulted in a higher rate of self-trauma than did scrotal neuters,11 which may be attributed to scrotal neuters being performed without suture closure, thus lessening the amount of tissue handling.10,11
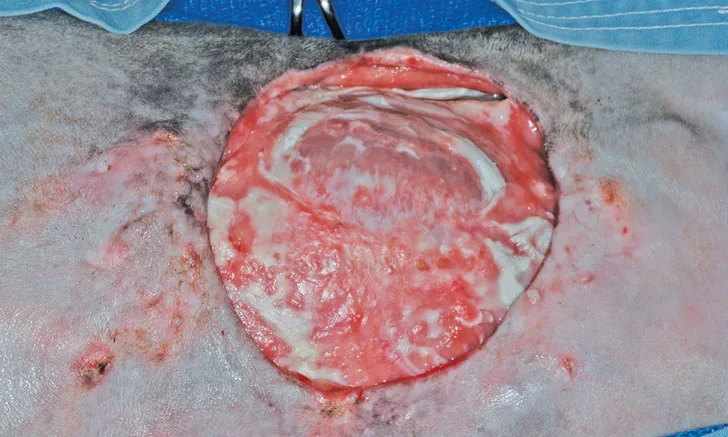
Surgical-site infections and other serious wound complications that are suggestive of infection (eg, wound pain and swelling, dehiscence, drainage; Figure 1) have been reported in 0.1% to 3% of elective gonadectomies.1,2,4,13 This rate is similar to the infection rates reported for clean, elective procedures in general (2.3%-5.7%).14 Infection rates can be reduced by decreasing surgery duration and using appropriate surgical technique (eg, gentle tissue handling, closure of dead space).14,15

Incisional infection and dehiscence after OHE in a dog (patient orientation, head left)
2. Intra-Abdominal Hemorrhage
Intraoperative hemorrhage is noted in 1.1% to 11% of dogs and cats undergoing gonadectomy and is most common in dogs >50 lb (22.7 kg) or when the surgery is performed by students.1,4,16 Postoperative abdominal hemorrhage is noted in ≤2.8% of patients undergoing gonadectomy.4 Rough tissue handling, poor ligation technique, inexperience, and inadequate exposure may play a role in intra-abdominal hemorrhage.
Cats undergoing gonadectomy are less likely to experience intra-abdominal hemorrhage than are dogs, even if ligatures are not used for ovarian pedicle hemostasis, as feline ovarian pedicles are generally small, less vascular, and more mobile as compared with canine ovarian pedicles. In a study of 2136 cats undergoing pedicle tie OHE, 0.28% of cats experienced intra-abdominal hemorrhage17; most cases were recognized and corrected during the procedure. In that study, uterine pedicle hemorrhage was noted in 0.14% of cats, and suspensory ligament hemorrhage was noted in 0.05% of cats.
Another source of intra-abdominal hemorrhage is splenic laceration, which can be caused by laparoscopic equipment or excessive spay hook use.18
Fatal abdominal hemorrhage from OHE or ovariectomy is rare, as most hemorrhaging is noted and addressed prior to closure.1,4,16,17 Patients with significant postoperative hemorrhage may have nonspecific signs (eg, slow anesthetic recovery, tachycardia, hypothermia, pale mucous membranes). Diagnosis is made via abdominal ultrasonography and abdominocentesis. In clinics without ultrasonography equipment, 4-quadrant abdominocentesis can be performed if the falciform ligament, which will block the needle, and spleen are avoided. Nonclotting blood on abdominocentesis confirms the diagnosis of hemoabdomen.19 If significant abdominal hemorrhage is detected, coagulation tests should be considered. The clinician must decide whether to treat the patient conservatively (eg, abdominal bandaging, sedation, monitoring, judicious use of fluids) or perform exploratory surgery. If surgery is chosen, the incision should be extended to provide adequate exposure, and the ovarian pedicles, suspensory ligaments, uterine stump, and other organs should be closely evaluated. If bleeding is identified, the tissue in question should be gently elevated from underlying structures with thumb forceps before the vessels are clamped and ligated. Transected ovarian pedicles commonly retract caudomedial to the kidneys and may rest immediately over the ureters. In cats, the distal ureters lie close to the uterine stump. Regardless of location, the ureters can be inadvertently ligated. If no active hemorrhage is observed during surgery, all pedicles should be ligated again, as anesthetic hypotension may mask vessel leakage.
Serious hemorrhage from gonadectomy is rare, but bleeding can occur from the incision or, in dogs undergoing prescrotal neutering, in the scrotum. In one study of scrotal and prescrotal neutering in 437 dogs >6 months of age, hemorrhage was observed in 16% of all dogs.11 Bleeding occurred more commonly in larger dogs, and surgical approach was not a factor in its occurrence.11 In another study of scrotal neutering with sutureless pedicle ties in dogs <6 months of age, no postoperative hemorrhage was noted.10 Hemorrhage after neutering is often related to bleeding from the tunics or SC tissue and is usually self-limiting.14 Affected patients can be treated with local pressure (dogs, scrotum; cats, scrotum or inguinal ring), cold packs, sedation, and exercise restriction and monitored for significant changes in hematocrit. Dogs with severe scrotal hematomas may develop abscessation or scrotal necrosis necessitating scrotal ablation. In rare cases, testicular vessels can retract through the inguinal ring into the peritoneal cavity, resulting in intra-abdominal hemorrhage. In these patients, clinical signs and treatment are similar to those in patients with postoperative hemorrhage after OHE.
3. Postoperative Pain
Some clinicians consider postoperative pain a normal effect of surgery. In one study, ≤12% of clinicians did not administer any postoperative analgesics to their patients, and many others relied on butorphanol, which may provide insufficient analgesia.3 Most retrospective studies of elective gonadectomy do not list pain as a potential surgical complication, and dogs undergoing routine gonadectomy are less likely to be prescribed postoperative analgesics than those undergoing other surgeries.1,2,9,12,20
Inadequate treatment of postoperative pain may be due to generational or gender differences among clinicians, cost or regulatory concerns, lack of access to appropriate drugs, and/or insufficient knowledge of pharmacology or pain detection in various species. For example, pain in cats tends to be undertreated because cats rarely show signs of pain after elective procedures.21 However, when mechanical nociceptor threshold (scrotal pressure tolerance) was measured in a study of cats after neutering, cats often reacted for ≥8 hours after surgery.21 In another study, cats exhibited decreased tolerance to abdominal palpation 18 hours after OHE but appeared pain free on visual assessment.22
Prolonged pain has also been noted in gonadectomized dogs. In one study, abdominal palpation and pain scores had not returned to normal by 72 hours after OHE.8 In another study, when pain was closely monitored after neutering, ≈50% of dogs required rescue analgesia within 3 to 4 hours of receiving preoperative morphine.23 Owners may note patient discomfort in dogs in the form of lethargy, restlessness, vocalization, and/or decreased appetite 1 to 3 days after gonadectomy.20,24
Clinicians should consider pre-emptive analgesics (eg, local or regional nerve blocks) and administer rescue opioids while the patient is being monitored in the clinical setting.3,25 Analgesics should also be prescribed for several days after the procedure.
4. Surgical Errors
Reported surgical errors include incomplete ovariectomy, pedicle granulomas and fistulas from use of nonabsorbable multifilament suture or nylon cable ties, inadvertent ureteral ligation, incisional hernias, retained surgical sponges or other foreign bodies (ie, gossypibomas), and inadvertent prostatectomy during cryptorchidectomy.1,14 The author has also seen uterine horns inadvertently tied together around the colon or urethra, resulting in stricture or obstruction. The exact incidence of surgical errors during elective gonadectomy is unknown. As with intra-abdominal hemorrhage, surgical errors can occur from inexperience or lack of sufficient anatomic exposure.
Ovarian remnant syndrome (ORS) occurs when functional ovarian tissue is inadvertently left in the patient (Figure 2).14 Patients with ovarian remnants are often overweight or have been spayed through a small incision, both of which can interfere with ovary visualization and appropriate clamp or ligature placement.1 Affected patients may display signs of estrus (eg, mammary or vulvar enlargement, behavior changes, vulvar discharge) or become clinically ill due to stump pyometra. Diagnosis of ORS is based on elevated concentrations of anti-Müllerian hormone and progesterone in peripheral blood.26 Treatment includes exploratory celiotomy, ovariectomy, and/or, if stump pyometra is present, removal of the uterus. Retained ovarian remnants are easier to locate when the patient is showing signs of estrus, as associated vessels will be enlarged and cystic follicles may be present in retained tissue.14

Retained left ovary (arrow) in a cat with behavioral signs of estrus 6 months after OHE (patient orientation, head right)
Inadvertent prostatectomy during removal of a cryptorchid testicle can also result from inadequate exposure, in which the clinician incorrectly identifies the almond-shaped prostate as a retained intra-abdominal testicle without noting the attached bladder and urethra. The author has witnessed students inadvertently expose the prostate through an abdominal incision when using a spay hook in attempt to locate a retained testicle. Dogs that have undergone inadvertent prostatectomy will have azotemia and anuria from urethral transection and ligation; subsequent bladder necrosis from overdistension can result in uroabdomen. Some dogs will regain urinary continence with surgical reanastomosis of the urethra.27
Retained surgical sponges can become walled off and cause no clinical signs for years; alternatively, affected patients may develop clinical signs as a result of adhesions, mass effect, fistulas or sinus tracts, vessel or visceral erosion, infection, or neoplastic transformation.28,29 Diagnosis can be difficult if a radiopaque marker is not present in the sponge, although the mass is usually evident on ultrasonography or CT. Treatment entails surgical removal of the sponge, in which careful dissection is required to prevent damage to local structures.29 Institution of sponge counts before and after each abdominal surgery can help decrease the risk for gossypibomas.
Ventral midline hernias occur in <1% of patients undergoing OHE.1,2,13,14 If the hernia is present within the first week after surgery, it is likely the result of technical error (eg, missed external rectus fascia, inappropriate suture size, suture bites that are too small or too far apart, knot failure).1,14
5. Hormonal Changes
Gonadectomy is common in the United States due to its value in surgical sterilization and preventing or reducing reproductive diseases (eg, benign prostatic hyperplasia, testicular tumors, pyometra, mammary neoplasia) and sexually driven behaviors.7 Adoption rates of shelter dogs are often increased with preadoption gonadectomy; however, evidence of its potential negative effects has been accumulating.7,30-40
Gonadectomy has been correlated with obesity in dogs and cats,30-32 which may result from changes in fasting metabolic rate (as has been noted in female cats), increased food intake, and/or decreased activity.31,32 Obesity may increase the risk for or exacerbate osteoarthritis and/or other systemic illnesses. Owners should be instructed on how to adjust activity levels and food intake to maintain their pet’s ideal body condition.
Another condition associated with neuter status is urinary incontinence in female dogs.33 Urinary incontinence is rare in intact bitches (0%-1%) but reportedly occurs in 5% to 20% of spayed female dogs.7,33,39,40 The risk appears to be greatest in dogs >33 lb (15 kg).40 Some studies have reported correlations with the dog’s age at the time of OHE, whereas others have found no significant effects.39-41 Signs of urinary incontinence can manifest as early as 4 weeks postoperation or may be delayed for 3 to 10 years.24,33 The pathophysiology of this acquired sphincter mechanism incompetence is unclear. Small-breed female dogs may have a greater risk for pyometra and mammary tumors than urinary incontinence; thus, the benefits of OHE before the first or second heat may outweigh the likelihood of complications.
Large- and giant-breed dogs, particularly golden retrievers, German shepherd dogs, and rottweilers, may be at greater risk for morbidity and mortality from joint disease, neoplasia, and urinary incontinence resulting from gonadectomy at a young age. Gonadectomy has been shown to increase the incidence of joint disorders in large-breed dogs by 2 to 5 times that of intact dogs, especially when performed in dogs <6 months of age.7,34,35 For example, in one study, the incidence of joint disorders was 5% in intact adult male golden retrievers as compared with 27% in those neutered before 6 months of age.34 In another study, joint disorders were diagnosed in 21% and 16% of male and female German shepherd dogs, respectively, gonadectomized at <1 year of age as compared with 7% and 5% of intact male and female German shepherd dogs, respectively.35
Gonadectomy may also be associated with an increased risk for certain cancers in large-breed dogs, although controlled studies are lacking. In one study of 683 rottweilers, bone sarcoma was diagnosed in 12.6% of dogs36; the risk for development of bone sarcomas was >3 times greater in dogs gonadectomized before 1 year of age. In other breeds, cancer-related deaths may be increased because gonadectomized animals live longer.7 Delaying gonadectomy until physical maturity (eg, >12 months of age) may be beneficial for large-breed dogs, although delaying surgery increases the risk for wound complications and surgical errors, likelihood of greater costs due to increased surgical time and anesthesia, and potential for unwanted litters before sterilization.
Because cats do not appear to experience many long-term ill effects from gonadectomy, other than the potential for obesity, prepubertal gonadectomy is usually considered acceptable for this species.37 However, gonadectomy in animals <7 months of age will delay physeal closure, which could increase the risk for physeal fractures in male cats, particularly if they become obese.42
Clinicians must weigh the risks and benefits of gonadectomy with the pet owner and determine the most appropriate age to neuter different breeds and species.