Top 5 Complications During & After Heartworm Treatment
Jennifer Anne Sidley, DVM, DACVIM (Cardiology), CVCA Cardiac Care for Pets, Alexandria, Virginia
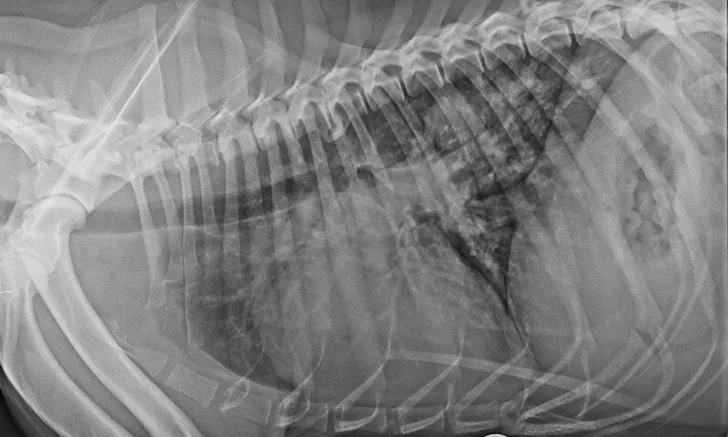
Radiograph from a dog with severe heartworm disease illustrating severe pulmonary arterial dilation, right heart enlargement, diffuse bronchointerstitial infiltrate, and focal region of pulmonary consolidation from embolized heartworms
Treatment complications can make heartworm disease particularly challenging. Following are the most common complications the author has encountered from heartworm treatment, as well as strategies to minimize them.
1. Pulmonary Emboli
Embolized worms are one of the most dangerous risks following melarsomine therapy. As worms die, they decompose, leaving fragments that become lodged in the distal pulmonary artery and capillary beds and block blood flow (Figure 1). The higher the worm burden and heartworm classification, the higher the risk for life-threatening complications. Clinical signs are most common 10 to 21 days postinjection but can occur as early as 2 days postinjection or as late as 30 days postinjection.1 Sudden coughing, hemoptysis, dyspnea, lethargy, and anorexia are hallmark signs. Pale mucous membranes, pulmonary crackles, fever, leukocytosis, and thrombocytopenia are common. Strict cage confinement, oxygen (if needed), and tapering anti-inflammatory doses of prednisone (0.5 mg/kg q12h for 1 week, 0.5 mg/kg q24h for the second week, then 0.5 mg/kg q48h for 1-2 weeks) are recommended if signs develop.2
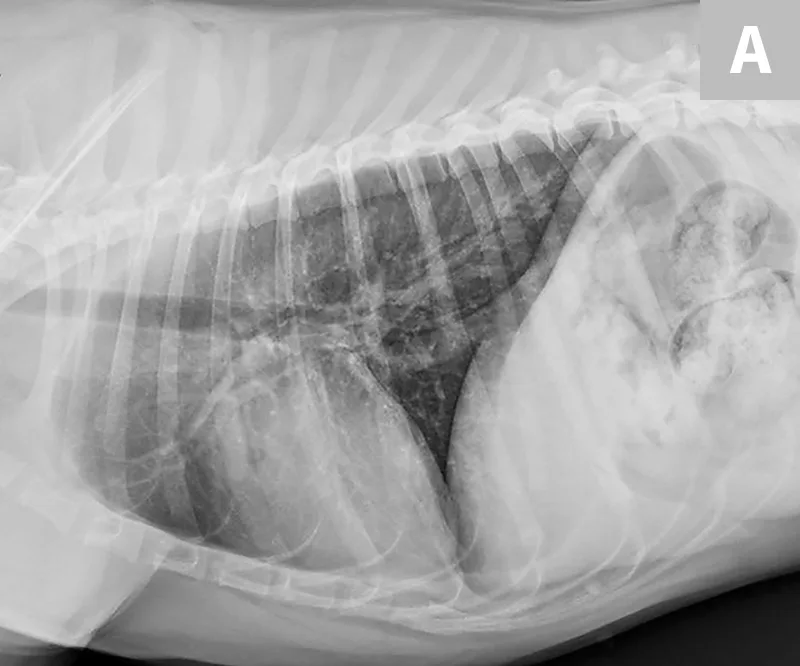
Radiographs before (A) and 11 days after (B) melarsomine injection showing increased overall pulmonary infiltrate with focal region of pulmonary consolidation from embolized worms (black arrow). A progressive increase in cranial pulmonary artery size can be seen (gray arrow). Images courtesy of Clarke E. Atkins, DVM, DACVIM
Before treatment, patients should be stabilized to maximize lung function and improve their ability to handle dying worms. Anti-inflammatory doses of prednisone 7 to 14 days before treatment should be given to patients with significant pulmonary infiltrate or respiratory signs (eg, coughing, tachypnea); right-sided heart failure should be treated and stabilized.
Exercise increases blood flow to damaged, blocked vessels and leads to worsening lung injury, increased pulmonary vascular resistance, pulmonary hypertension, and, potentially, right-sided heart failure. Therefore, strict exercise restriction is essential to minimize the severity of cardiopulmonary damage.3,4 Restriction should begin the day of diagnosis and extend throughout the entire treatment and recovery period, with the most extreme restriction lasting 4 to 6 weeks after each melarsomine injection.2 Restriction may vary depending on patient and owner needs but ideally involves cage confinement or restriction to a single room with just short leash walks to eliminate, particularly for more severe cases.
A split 3-dosage protocol can reduce the severity of complications from dying worms.5 The first injection kills approximately 50% of worms, then the lungs are able to recover for one month before the other half of the worms are killed. If the lungs have not fully healed at this point, the second and third injections can be delayed until signs have resolved.6
2. Rapid Microfilarial Death
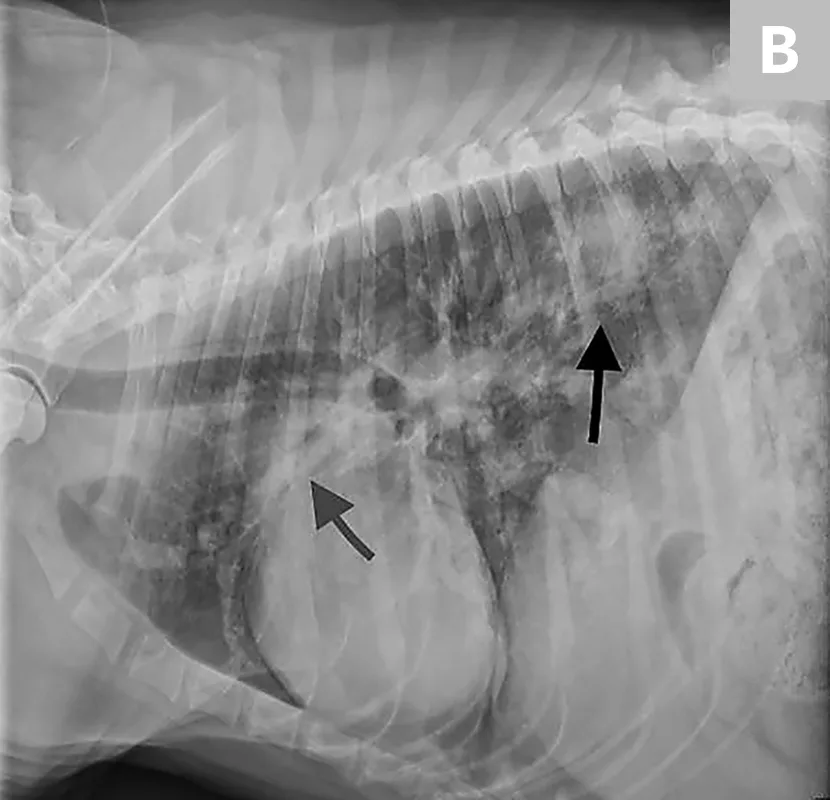
Rapid microfilarial death (Figure 2) can cause signs ranging from mild lethargy, ptyalism, inappetence, and nausea to more severe hypotension, tachycardia, tachypnea, and collapse. If these signs develop, supportive care with IV fluids and soluble glucocorticoids (eg, dexamethasone sodium phosphate [0.25 mg/kg IV slowly over 2-4 minutes]) is indicated. Rapid microfilaricidal treatment with high-dose (ie, 50 μg/kg) ivermectin is no longer recommended by the American Heartworm Society2; instead, a combination of doxycycline (10 mg/kg q12h for 4 weeks) with a monthly macrolide preventive is recommended to kill microfilariae at a slower rate with less potential for complications.2 Within 5 to 9 months, most dogs will become amicrofilaremic. Because milbemycin oxime kills microfilariae much more rapidly than do ivermectin, selamectin, and moxidectin, the latter 3 have a lower risk for microfilarial death complications and are preferred in dogs that are microfilaremic.6 In microfilaremic dogs, administration of glucocorticoids (eg, prednisolone [1 mg/kg PO], dexamethasone [0.25 mg/kg IV]) with or without antihistamines (eg, diphenhydramine [1 mg/kg IV or IM]) is recommended one hour before, and possibly again 6 hours after, administration of the first dose of preventive; patients should be monitored for potential adverse effects for the first 8 to 12 hours.2,6
Single microfilaria in a blood smear
3. Incomplete Adulticide Efficacy
Closing the gap in treatment so that all stages present are susceptible can help prevent persistent heartworm infection postadulticide therapy. Melarsomine kills adults and mature L5 larvae that are at least 4 months postinfection. Macrolide preventives reliably kill L3 and L4 larvae that are present up to 2 months postinfection; thus, there is a 2-month gap when immature L5 larvae are not sensitive to either preventive or melarsomine and can later develop into adult heartworms. Allowing 2 to 3 months to lapse after preventive treatment before administering melarsomine can help close this gap and allow all stages present to be sensitive to melarsomine and prevent treatment failure.2,6
Melarsomine is not 100% effective, and not all worms are killed in every patient. The extended 3-dose treatment protocol has a higher efficacy than the 2-dose protocol.6,7 The American Heartworm Society recommends the 3-dose protocol for all dogs treated for heartworms, regardless of stage, because of its higher efficacy and lower risk for pulmonary complications.2 This may involve greater cost for the owner and a longer period of exercise restriction, but the potential benefit for the patient outweighs this added cost and inconvenience.
Improved sensitivity of tests over time has allowed clinicians to detect smaller worm numbers (as few as 1-3 female worms). Typically, the worm burden is still significantly reduced in persistently positive animals. The decision for retreament should be made on a case-by-case basis, depending on patient age, activity level, worm burden, and history. A geriatric, low-energy dog would likely tolerate a few persistent worms better than would a young, active dog, and the latter would benefit more from retreatment.
4. Injection Site Reactions
Significant irritation can occur at the injection site, causing pain, swelling, tenderness, seroma formation, and reluctance to move. Care should be taken to follow the recommended technique and inject deep in the muscle belly to avoid superficial or subcutaneous injection and leakage. Administering butorphanol before the injection can help reduce discomfort, and the sedation may also help ensure proper technique. Hypersalivation, panting, vomiting, diarrhea, anorexia, and weakness have also been reported following injection.6,8
5. Caval Syndrome
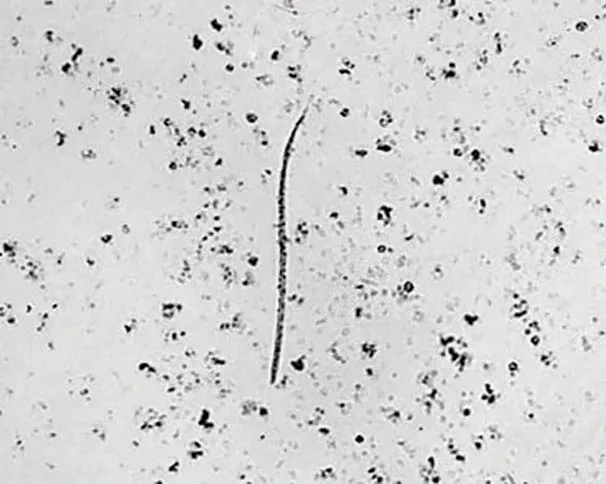
When large numbers of worms mature over a short period of time, the right heart chambers and vena cava can become engorged with worms (ie, caval syndrome), leading to severe right-sided heart dysfunction, pulmonary hypertension, intravascular hemolysis, hemoglobinuria, disseminated intravascular coagulation, shock, and multiple organ failure (Figures 3 and 4).
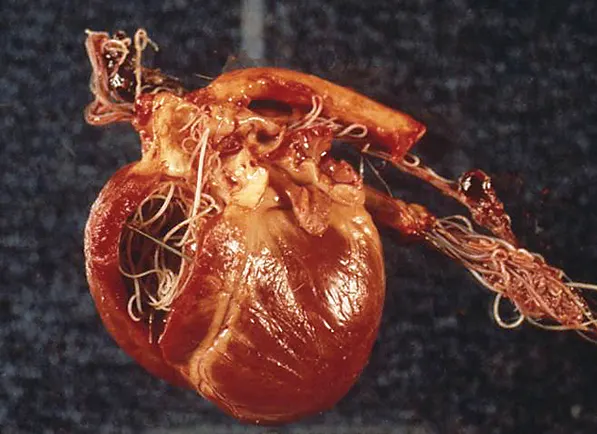
Gross image of a dog with caval syndrome. Image courtesy of Clarke E. Atkins, DVM, DACVIM
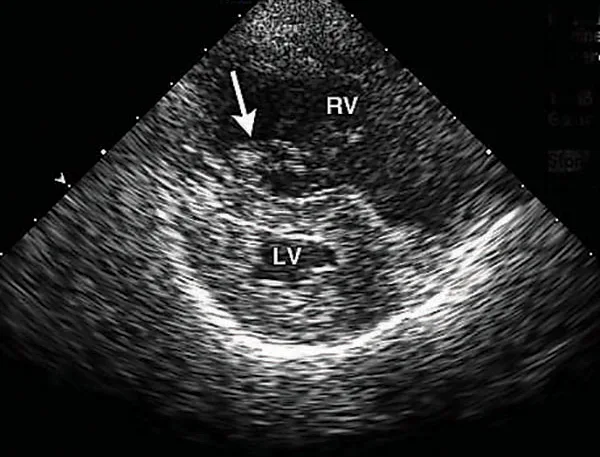
Echocardiogram of a dog with caval syndrome showing large worm burden (arrow) in the right ventricle, severe right ventricular hypertrophy, and septal flattening. Image courtesy of Clarke E. Atkins, DVM, DACVIM
Prompt extraction of the worms to remove the obstruction is essential for survival and typically involves referral to a specialist with proper tools (eg, long alligator forceps, horsehair catheter, basket retrieval device).9 During extraction, care must be taken to avoid excessive intracardiac or vessel damage, as well as laceration to the worms themselves, which can cause sudden antigenic release from macerated heartworms and fragment emboli. Without prompt worm retrieval, most dogs live only a few days; with worm retrieval, survival rates up to 60% to 71% have been reported, although outcomes are likely highly dependent on the clinician’s expertise.10 Melarsomine therapy is usually needed to kill the remaining worms.