Top 5 Classifications of Blindness
Ron Ofri, DVM, PhD, DECVO, Hebrew University of Jerusalem
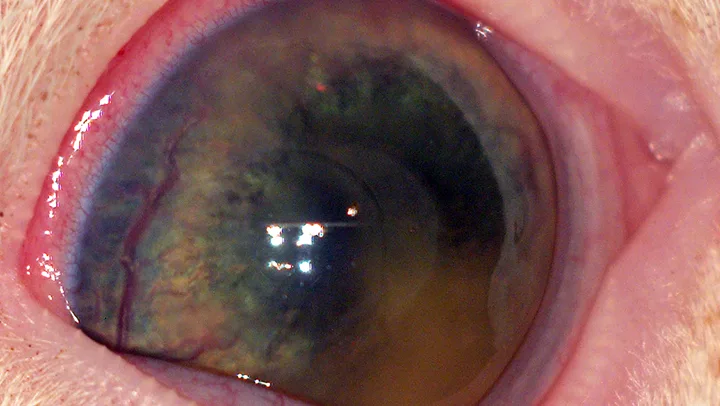
Uveitis in a 4-month-old kitten diagnosed with feline infectious peritonitis. The large hypopyon covers the entire pupil, which makes vision impossible in this eye.
Acute blindness is a most distressing event for both patient and owner. Clients naturally want to know whether vision can be restored. Fortunately, in many cases, the answer is yes; however, owners and veterinarians should bear in mind that acute blindness may frequently be a manifestation of systemic disease. Therefore, even patients that do not regain vision should undergo a comprehensive examination to establish an ophthalmic and systemic diagnosis; the latter may have profound, long-term implications for the patient’s health.
As with any patient, the examination should begin with a thorough history. Inquire whether the blindness is acute or gradual-onset, as this may help differentiate between acquired and inherited causes of blindness. Acute blindness is frequently a result of acquired causes, whereas progressive vision loss is usually because of inherited causes.1 Although owners frequently report sudden loss of vision, ophthalmic examination may show signs associated with progressive disease. In such cases, careful questioning should reveal that the blindness was noticed upon a change in environment (eg, visiting friends); the animal presumably has been blind for a long time, but the gradual onset of the disease enabled it to learn to navigate at home.1
Next, inquire whether the blindness was associated with preferential night vision loss. An early behavioral sign of many inherited, degenerative diseases of the outer retina (commonly known as progressive retinal atrophy [PRA]) is night vision loss because rods are affected before cones.1
Finally, ask whether there are other signs of illness. Blindness may be caused by numerous systemic or neurologic diseases, which are frequently accompanied by additional clinical signs. Therefore, a complete physical examination and thorough neurologic assessment are indicated in each case of blindness.1 These are followed by a comprehensive ophthalmic examination. Based on its results, the blind patient can be classified into one of the following 5 categories.
1. Light Does Not Reach the Retina
Simply put, if you cannot (ophthalmoscopically) see the retina, the retina cannot see you. Opacity anywhere along the optical pathway of light from the cornea to the retina will cause vision to be lost or diminished.1 Common causes of opacity include severe corneal pigmentation, infiltration or edema, loss of aqueous humor transparency because of hyphema or hypopyon, and advanced cataracts. Patients presenting with severe corneal pigmentation or infiltration should be examined for corneal disease. In cases of severe corneal corneal edema, the clinician should consider corneal ulcers, uveitis, and glaucoma. Hypopyon is most often caused by a systemic inflammatory or infectious disease (Figure 1), whereas hyphema may be caused by systemic hypertension, coagulopathies, trauma, infectious diseases, and/or diseases causing anemia or thrombocytopenia. Patients with cataracts should be referred to a veterinary ophthalmologist for possible surgery.
Severe pain and blepharospasm, an extremely miotic pupil, and vitreous haze from inflammation or bleeding may also cause blindness. In patients with severe blepharospasm, consider potential causes of pain (eg, corneal ulcers, foreign bodies, eyelid or eyelash abnormalities). Patients with severe miosis or vitreous haze should be evaluated for intraocular disease.
2. Ophthalmoscopic Examination Is Abnormal, but Pupillary Light Reflex (PLR) Is Present
Early ophthalmoscopic signs of PRA are subtle and limited to the retinal periphery. As the disease progresses, however, the 2 classical ophthalmoscopic signs—tapetal hyperreflectivity and attenuation and loss of retinal blood vessels—become increasingly noticeable. However, the PLR is usually present even in advanced stages of the disease, though it may be diminished and the pupils may be abnormally dilated. The PLR will be completely lost only in terminal stages of the disease, when the entire retina has atrophied (Figure 2). Most patients are presented to veterinarians before reaching this stage. There is no effective treatment for retinal atrophy.2

Terminal, progressive retinal atrophy characterized by complete loss of retinal vasculature, a hyperreflective tapetum, and optic disc atrophy in a 12-year-old poodle. At this stage, the animal has no PLR, but some degree of the reflex is usually present in earlier stages of the disease.
Signs of retinal inflammation (chorioretinitis) should also be visible ophthalmoscopically, and visual deficits occur in affected areas. However, the inflammation is frequently focal or multifocal. Unless the entire retina is affected, partial vision may be maintained by the unaffected retina. In such cases, owners may not notice the visual handicap, and some degree of PLR will be present.
3. Ophthalmic or Ophthalmoscopic Examinations Are Abnormal, & There Is No PLR
There are 3 diseases in which patients are presented with acute blindness and fixed dilated pupils and can be diagnosed following a comprehensive ophthalmic examination:
Glaucoma is associated with numerous clinical signs, most notably pain, buphthalmos, corneal edema, and episcleral congestion. Clinicians should aim to determine if the disease is primary or secondary and offer appropriate treatment.3
Signs of optic disc inflammation (eg, edema, congestion, focal hemorrhage, disc elevation, peripapillary retinal detachment) may be seen in cases of proximal optic neuritis. A common sequela is optic atrophy, in which patients present with a round brown-gray disc (Figure 3). These patients should undergo neurological evaluation.4,5
A detached retina can be seen as a vascular, white-gray veil behind the lens (Figure 4). Varying degrees of intra- or subretinal hemorrhage may be seen. When the fundus cannot be seen (eg, because of severe corneal edema or hyphema), the detachment may be demonstrated by ultrasound. Rhegmatogenous retinal detachments, in which liquified vitreous enters the subretinal space through a retinal hole, are usually primary. No detailed evaluation is required, and patients can be referred to a specialist for retinal reattachment surgery if indicated. Other types of retinal detachments may be caused by systemic hypertension, systemic infections, or vascular diseases. These require a full systemic evaluation. Successful treatment of the primary cause may cause retinal reattachment and restored vision.6,7

Figure 3A Fundus picture of left eye of a 6-year-old dachshund. The optic disc is atrophied. Compare to Figure 2, in which both the retina and optic disc are atrophied, and to the normal right eye (3B).
4. Ophthalmic Examination Is Unremarkable, but There Is No PLR
The 2 leading differential diagnoses for such a presentation are sudden acquired retinal degeneration (SARD) and optic neuritis affecting retrobulbar parts of the optic nerve (which is why the optic disc is normal-looking), up to and including the optic chiasm. The 2 may be differentiated by referring the patient for electroretinographic recording of retinal function, which will be normal in optic neuritis and absent in SARD (Figure 5). The recording has important prognostic implications; there is no proven treatment for SARD, but optic neuritis cases should be evaluated neurologically, as some cases, such as those caused by infectious diseases or granulomatous meningoencephalitis have systemic ramifications, and may be treated successfully.8,9

The normal-looking fundus of a 9-year-old Labrador retriever diagnosed with SARD.
5. Ophthalmic Examination Is Unremarkable, & PLR Is Present
Blind patients with normal PLR and an unremarkable ophthalmic examination are neurological cases. The presence of the PLR means that the lesion is in the distal visual pathways or cortex after the fibers providing afferent innervation to the iris sphincter muscle have diverged from the optic tract. These patients may suffer from congenital, inflammatory, infectious, or metabolic diseases of the central nervous system, and a neurologist should be consulted.5