Top 5 Causes of Erythrocytosis in Dogs & Cats
Elizabeth Flaherty, DVM, Companion Care Vets, Redhill, Surry, United Kingdom
Lisa M. Pohlman, DVM, MS, DACVP, Kansas State University
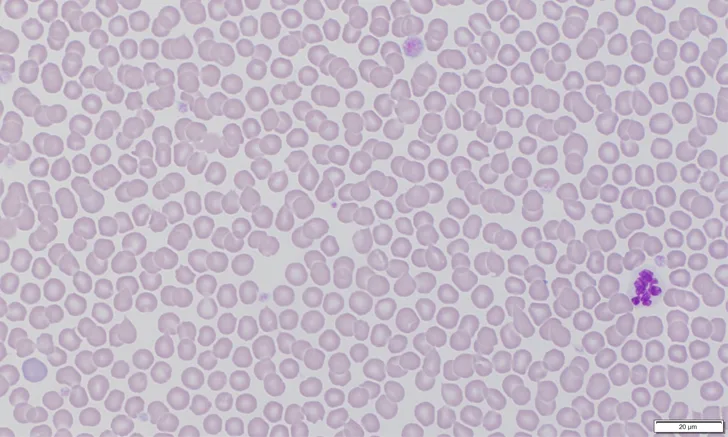
Erythrocytosis (ie, polycythemia) is an increase in erythrocytes in the peripheral blood; is characterized by increased hematocrit, hemoglobin, and RBC concentration; and can be relative or absolute (Figure).1
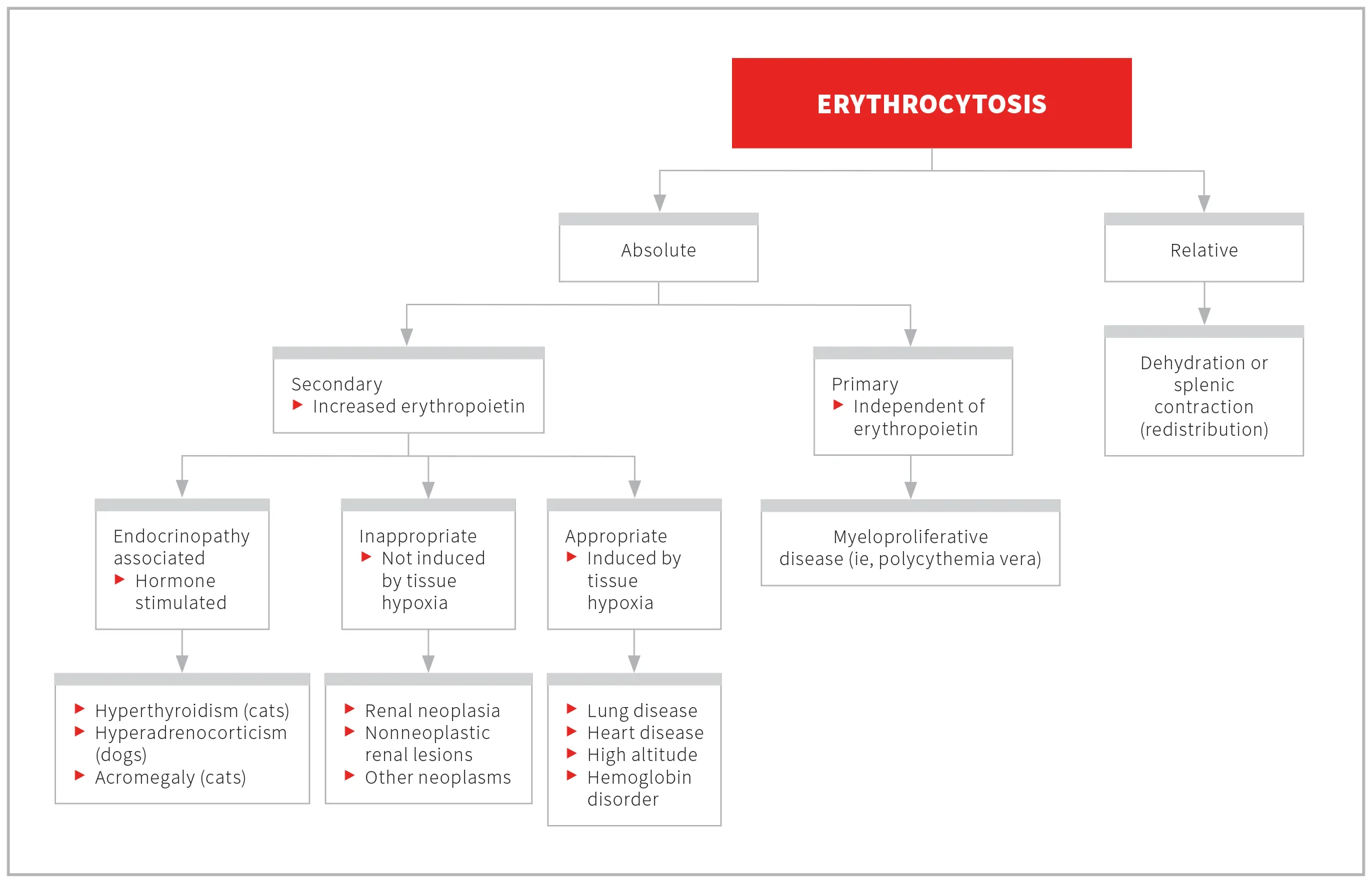
Approach to classifying erythrocytosis1,6
Relative erythrocytosis is an increased hematocrit not caused by an increase in total body RBC mass.1 Examples include hemoconcentration secondary to dehydration and redistribution caused by epinephrine-induced splenic contraction.2,3
Absolute erythrocytosis is caused by an absolute increase in total body RBC mass and can be primary or secondary.1,4 Primary absolute erythrocytosis is present when there is increased RBC proliferation in the absence of increased erythropoietin and is most indicative of a neoplastic myeloproliferative condition (ie, polycythemia vera) in veterinary patients.4 Secondary absolute erythrocytosis results from increased concentrations of erythropoietin that stimulate erythroid hyperplasia in bone marrow and increase RBC production and can be appropriate, inappropriate, or endocrinopathy-associated.1,2,4-6 Secondary appropriate absolute erythrocytosis is induced by tissue hypoxia. Secondary inappropriate absolute erythrocytosis is due to uncontrolled erythropoietin secretion, not induced by tissue hypoxia.1,2,4,5
Clinical signs of erythrocytosis are secondary to hyperviscosity caused by increased RBC mass and depend on the degree and duration of hematocrit increase. Signs may include erythematous to cyanotic mucous membranes, dark-colored blood, dilated episcleral vessels, increased capillary refill time, tachycardia, tachypnea, neurologic disturbances secondary to hypoxic injury from increased blood viscosity (eg, weakness, lethargy, ataxia, seizures, blindness, behavior changes), vomiting, abdominal or lumbosacral pain, thrombosis, microvascular injury, polyuria, polydipsia, and bleeding (eg, melena, epistaxis, hematochezia, hematuria, hematemesis) as a result of decreased blood flow and consequential sludging of blood in small vessels that can lead to congestion, distention, and ultimately thrombosis, tissue hypoxia, and vessel rupture.6-11
Following are causes of erythrocytosis listed in order of most to least common, according to the authors.
1. Dehydration & Splenic Contraction (Relative Erythrocytosis)
Dehydration
Dehydration causes hemoconcentration and decreased total intravascular fluid volume without decreased erythrocytes,7 resulting in an artifactual increase in hematocrit due to hemoconcentration.1
Clinical evidence of dehydration during physical examination can help identify erythrocytosis due to dehydration. Uncomplicated cases may have concurrent prerenal azotemia with urine specific gravity that indicates urine is concentrated and there is increased serum total protein.7 Sodium and chloride may also be increased, depending on the tonicity of the fluid lost.1
Erythrocytosis due to dehydration can be treated with fluids to correct the volume deficit. Type and route of fluid administration should be based on the degree of dehydration, the underlying condition causing dehydration, and other metabolic abnormalities.4
Splenic Contraction
Pain, fear, and exercise cause epinephrine release, resulting in contraction of splenic smooth muscle and release of erythrocyte-rich splenic blood into the peripheral circulation.1 Peripheral blood (normal hematocrit, ≈35%-50%, depending on species) mixes with high-hematocrit splenic blood (hematocrit, 70%-80%) to cause erythrocytosis.1 Splenic contraction is a normal, short-term, physiologic response to epinephrine that abates when the stimulus is removed and the patient is calm. Erythrocytosis due to splenic contraction is most common in dogs because dogs have a muscular spleen; however, in experimental conditions, cats showed a 25% increase in hematocrit from splenic contraction.1 Unlike erythrocytosis due to hemoconcentration, serum total protein is in the reference interval in patients with splenic-contraction–induced erythrocytosis.1,2,4 Other signs of catecholamine release (eg, excitement leukogram [ie, mature neutrophilia with concurrent lymphocytosis]) are possible.4
2. Hypoxemia (Secondary Appropriate Absolute Erythrocytosis)
Tissue hypoxia (eg, as a result of adjustment to high altitude, chronic pulmonary disease, cardiac disease, hemoglobin disorders, cardiac shunts, venoarterial shunts) stimulates increased release of erythropoietin, which may lead to secondary appropriate absolute erythrocytosis.1,4,7-9,12,13 This type of erythrocytosis is characterized by erythrocytosis with chronic hypoxemia, which is most often induced by partial pressure of oxygen <60 mm Hg.4,7
3. Erythropoietin-Secreting Neoplasms (Secondary Inappropriate Absolute Erythrocytosis)
Secondary inappropriate absolute erythrocytosis can occur due to increased production of erythrocytes induced by an erythropoietin-secreting neoplasm; this is an inappropriate response because erythropoietin production is increased in the absence of systemic hypoxia.4,7 Most erythropoietin or erythropoietin-like substance-releasing tumors are renal in origin and may include primary renal lymphoma, renal sarcoma, nephroblastoma, renal cell carcinoma, fibrosarcoma, or adenocarcinoma.4,9,13-15 Erythropoietin may also be secreted by tumors of other tissues, including nasal fibrosarcoma, hepatocellular carcinoma, schwannoma, and cecal leiomyosarcoma.2,5,16 Renal tumors may lead to erythrocytosis via paraneoplastic processes that release erythropoietin or an erythropoietin-like substance from tumor cells or via damage to blood flow in the renal parenchymal microvasculature with subsequent erythropoietin release due to local hypoxia.4,7,9,14,15
Renal tumors should be confirmed because other renal injuries, including pyelonephritis, can also lead to inappropriate secondary erythrocytosis.7 Erythrocytosis related to renal tumors is generally mild to moderate but has been reported as severe in some cases.13 Erythropoietin or an erythropoietin-like substance produced by these tumors can be confirmed with immunohistochemistry detection of erythropoietin mRNA in the tumor cells using reverse-transcriptase PCR.5,16 Treatment includes removal of the erythropoietin-secreting neoplasm and management of erythrocytosis using therapeutic phlebotomy and fluid support with IV crystalloids.13 Myelosuppression with hydroxyurea may be recommended if erythrocytosis is severe enough to require phlebotomies more frequently than every 4 weeks.13
4. Endocrinopathy-Associated Erythrocytosis (Secondary Absolute Erythrocytosis)
Hormones (eg, cortisol in dogs, thyroxine and growth hormone in cats) can directly or indirectly stimulate erythropoiesis. It is important, however, to note that endocrinopathy-associated erythrocytosis is generally mild if present and alone is insufficient to result in clinical signs.6
5. Myeloproliferative Neoplasia (ie, Polycythemia Vera; Primary Absolute Erythrocytosis)
Polycythemia vera, the cause of primary absolute erythrocytosis, is a chronic myeloproliferative disease characterized by an increase in hematocrit or packed cell volume >65%, no increase in erythropoietin concentration, normal blood volume, and normal arterial partial pressure of oxygen.2,10,11 Polycythemia vera most commonly affects middle-aged to older dogs; no sex or breed predisposition has been reported.10 Pathogenesis includes rapid production of an increased number of erythrocytes with normal to prolonged half-life in the blood. In some dogs, a mutant oncogene JAK2 sequence with 2 amino acid changes (ie, V617F, C618L) controls the autoregulation of kinase activity and leads to constitutively active kinase and an increase in erythrocyte production in the absence of erythropoietin.3,10,11 Treatment includes therapeutic phlebotomy and IV hydration with crystalloids to reduce blood viscosity, as well as myelosuppressants (most commonly, hydroxyurea) to lower hematocrit to a normal range.10,11
Mean survival time is ≈5 months in dogs treated only with phlebotomies.10 Survival time can increase to between 8 and 33 months in dogs treated with hydroxyurea following reduced hematocrit (ie, <60%) via phlebotomy and fluid replacement.6,10 Initial administration of hydroxyurea in dogs should be 30 mg/kg PO once every 24 hours (or divided and given every 12 hours) for 1 to 2 weeks, then every 48 hours and tapered to the lowest effective frequency.6,10,17 Intervals longer than 48 hours were found to be insufficient for management of polycythemia vera in dogs in a report.10 Adverse effects of hydroxyurea may include anorexia, vomiting, alopecia, sloughing of nails, and bone marrow hypoplasia.
A similar administration schedule is reported in cats, with a suggested maintenance dosage of 22 mg/kg PO every 48 hours.17 Cats given large doses of hydroxyurea are likely to develop methemoglobinemia and Heinz body hemolytic anemia in addition to adverse effects; lower doses should thus be considered, and patients should be monitored carefully.6