The term cardiac arrhythmia encompasses all cardiac rhythms other than a normal sinus rhythm, including both bradyarrhythmias (ie, abnormally slow heart rate) and tachyarrhythmias (ie, abnormally fast heart rate).
Cardiac arrhythmias can be benign or life-threatening. The following reviews 5 of the most common cardiac arrhythmias identified in dogs and cats and outlines recommended treatment protocols.
1. Sinus Arrhythmia
Sinus arrhythmia results from variations in vagal tone associated with respiration; the overall heart rate is normal, but the rate rises on inspiration and slows on expiration. This can be common in dogs, which normally have a high resting vagal tone. Brachycephalic breeds appear predisposed to sinus arrhythmia because of increased breathing effort.
In cats, sinus arrhythmia is less common, as the feline heart rate is more sympathetically driven, especially when a cat is at the clinic. If sinus arrhythmia is identified in a cat, the patient may have excessive vagal tone from pathology in the intracranial, intraocular, respiratory, GI, or (less common) urogenital systems.
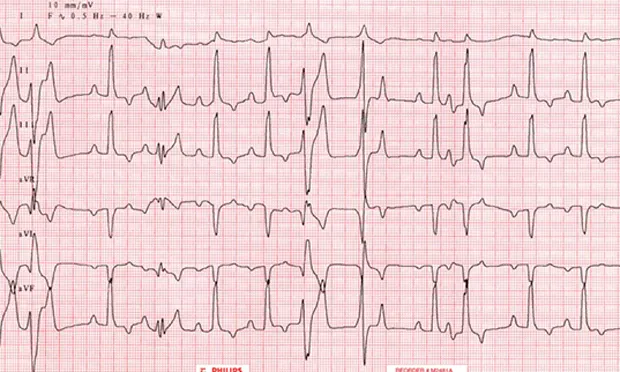
The ECG characteristics of sinus arrhythmia are a normal heart rate and a regularly irregular sinus rhythm, with more than 10% variation in RR intervals (Figure 1A).
An atropine response test can help differentiate true conduction disturbance (eg, sick sinus syndrome) from vagally mediated sinus arrhythmia. Patients with high vagal tone should have a complete response to atropine and a resultant sinus tachycardia (heart rate >160 bpm; Figure 1B), whereas patients with sick sinus syndrome may not respond or may respond only partially to atropine (Figures 1C and 1D). The authors typically administer 0.04 mg/kg of IM atropine, wait 20 to 30 minutes, and then recheck the heart rate via ECG or auscultation.
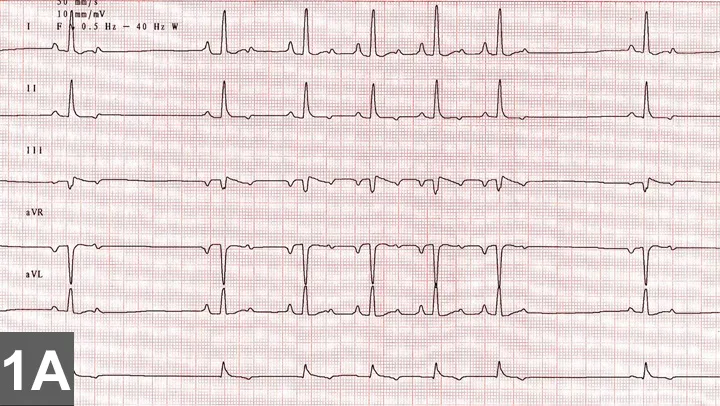
FIGURE 1A
Six-lead ECG illustrating sinus arrhythmia in a healthy dog. The 4 beats in the middle are at a faster rate (100 bpm) than the sinus beats (~60 bpm; paper speed, 50 mm/sec; sensitivity, 5 mm/mV).
2. Atrial Fibrillation
Atrial fibrillation is caused by multiple reentrant circuits in the atria that can fire at rates up to 500 to 600 bpm. The atrioventricular (AV) node acts as a gatekeeper and determines how many of these impulses are propagated through to the ventricles. Giant-breed dogs (eg, Irish wolfhound) can develop lone atrial fibrillation, wherein they do not have underlying structural heart disease based on ECG assessment. More commonly in dogs and almost exclusively in cats, atrial fibrillation is associated with significant heart disease and atrial enlargement because a critical mass is required to support the 5 or 6 reentry circuits necessary for atrial fibrillation propagation. The atria in giant-breed dogs (and humans and horses) can potentially support atrial fibrillation, whereas cats and most other dogs must have significant atrial dilation as a result of cardiac disease to achieve the critical mass.
The ECG characteristics of atrial fibrillation are lack of P waves and irregularly irregular supraventricular rhythm, with or without tachycardia (heart rate >160 bpm; Figure 2A).
In dogs, the goal of treatment is typically to slow the ventricular response rate to a target heart rate of approximately 140 to 160 bpm as assessed by ECG (Figure 2B). This is best accomplished with a combination of extended-release diltiazem preparation and digoxin.1
Although some prefer use of a β-blocker, β-blockers and calcium-channel blockers can have negative inotropic effects and thus should be used cautiously and slowly up-titrated when there is concurrent heart failure or systolic dysfunction. In cases of lone atrial fibrillation, medical or electrical cardioversion (ie, conversion back to normal sinus rhythm) can be attempted; however, this requires general anesthesia, and survival or improved quality of life has not been definitively demonstrated in humans or dogs. Many patients with lone atrial fibrillation have fairly slow ventricular response rates and do not require medical therapy. Cats with atrial fibrillation are generally treated with either a calcium-channel blocker or a β-blocker, using caution in the face of congestive heart failure or systolic dysfunction.
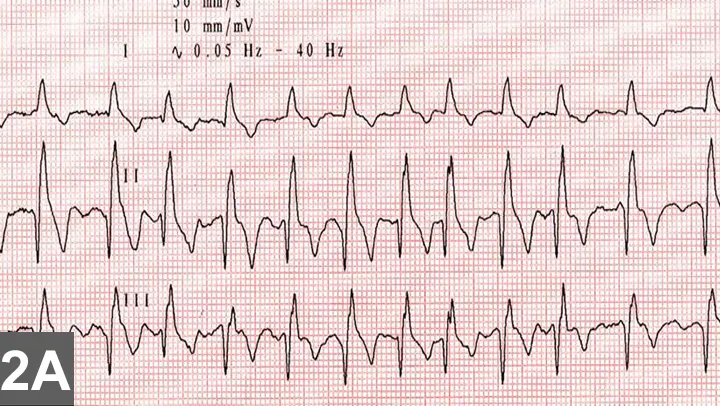
FIGURE 2A
Three-lead ECG from a Doberman pinscher with dilated cardiomyopathy. There is uncontrolled atrial fibrillation. The fast heart rate, lack of discernible P waves, and irregularity are all characteristic of atrial fibrillation. In this patient, the QRS complexes are wide because of left ventricular enlargement. Because of heart orientation in deep-chested animals (eg, Doberman pinschers), left ventricular enlargement often creates a widened QRS complex (instead of a tall R wave). Heart rate ranges from 230300 bpm (paper speed, 50 mm/sec; sensitivity, 10 mm/mV).
3. Ventricular Tachycardia
Ventricular tachycardia (VT) is a potentially life-threatening arrhythmia that can result in sudden death. VT can occur in patients with primary cardiac disease such as arrhythmogenic right ventricular cardiomyopathy (common in boxers) or dilated cardiomyopathy (common in Doberman pinschers). Ventricular arrhythmias can also be hereditary and can occur in patients with a structurally normal heart.
The ECG characteristics of VT include wide and bizarre QRS complexes without any associated P waves in addition to tachycardia (heart rate, >180 bpm; Figure 3A).
Although no treatment has been proven to prevent sudden death in patients with VT, antiarrhythmic therapy is used especially if the patient is a breed predisposed to sudden death, the patient is symptomatic, and/or malignant characteristics are present on VT (eg, rapid heart rate [>180 bpm]) or R-on-T or polymorphic QRS complexes are present (Figure 3B). The most common medications used for ventricular arrhythmias include IV lidocaine (acutely administered), sotalol, and PO mexiletine. Sotalol and mexiletine can be compounded into a liquid formulation for titration of doses, if necessary. In cases of significant systolic dysfunction, mexiletine can be used at 4 to 8 mg/kg PO q8h. This same dose can be added to sotalol when ventricular arrhythmias persist despite administration of maximal doses of sotalol. Other medication combinations (amiodarone, flecainide, propafenone, procainamide) may be needed for patients that are refractory to conventional therapy. Implantable defibrillators are occasionally required to treat high-risk patients.
An accelerated idioventricular rhythm should not be confused with VT. Accelerated idioventricular rhythm can also be referred to as slow VT because of the similar appearance on ECG, but the heart rate is generally less than 180 bpm (Figure 3C). Accelerated idioventricular rhythms are often seen in patients with systemic disease (eg, gastric dilatationvolvulus, pancreatitis, hemangiosarcoma, immune-mediated hemolytic anemia) rather than primary cardiac disease. Antiarrhythmic therapy is often unnecessary, as this type of arrhythmia is not typically hemodynamically compromising and is often self-limiting with treatment of the primary disease.
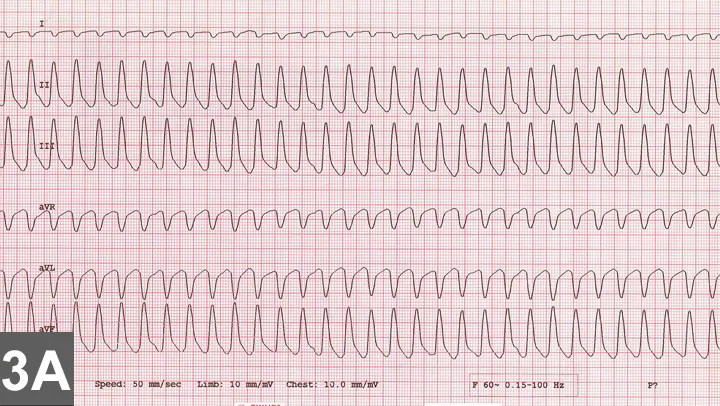
FIGURE 3A
Six-lead ECG in a boxer with arrhythmogenic right ventricular cardiomyopathy. There is monomorphic VT at an extremely fast rate of ~350 bpm (paper speed, 50 mm/sec; sensitivity, 10 mm/mV).
4. Premature Beats
There are 2 main categories of premature beats: supraventricular premature contractions (including atrial premature contractions [APCs], AV junctional premature contractions) and ventricular premature contractions (VPCs). The many possible causes of these abnormal heartbeats include electrolyte abnormalities, systemic disease, and cardiac disease. Premature contractions are likely more common as patients age.
The ECG characteristics of APCs include premature P waves associated with supraventricular-appearing QRS complexes. The P wave may be superimposed on the preceding T wave and, therefore, difficult to identify (Figure 4A). The ECG characteristics of VPCs are wide and bizarre premature QRS complexes without associated P waves. The QRS complexes may have a single morphology (Figure 4B) or multiple different morphologies (polymorphic) within the ventricles (Figure 4C).
Antiarrhythmic therapy is not necessary for APCs. Treatment of single VPCs is not typically necessary but should be considered if there are couplets (two VPCs in a row) or runs (three or more VPCs in a row), particularly if the coupling rate is rapid, there is R-on-T or the ventricular ectopy is polymorphic in appearance, or the patient is symptomatic from hemodynamic compromise (eg, history of weakness, syncope). Common antiarrhythmic medications include sotalol and/or mexiletine.
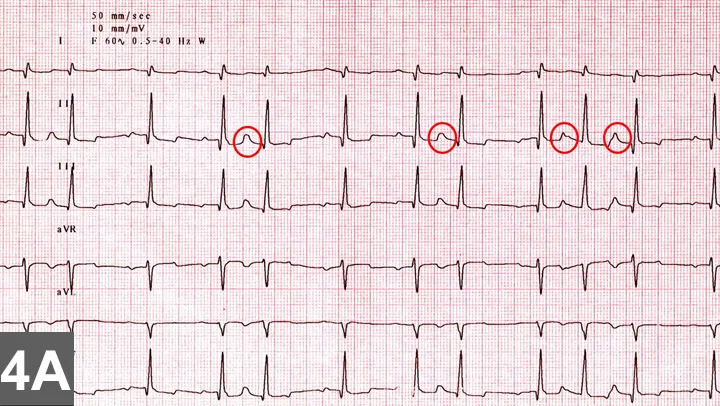
FIGURE 4A
Six-lead ECG in a dog with an auscultated arrhythmia. There is sinus rhythm with 5 single APCs that fall on top of the preceding T wave and change the morphology of the T wave (circled; paper speed, 50 mm/sec; sensitivity, 10 mm/mV).
5. Atrioventricular Block
First-degree AV block is characterized by a prolonged PR interval, with all P waves having an associated QRS complex. Second-degree AV block is characterized by some P waves being blocked, while others are conducted with an associated QRS complex. There are three types of second-degree AV block:
Mobitz type I (Wenckebach): The PR interval progressively lengthens before the blocked P wave (Figure 5A).
Mobitz type II: The PR interval is constant before the blocked P wave (Figure 5B).
High grade: No two P waves are consecutively conducted (2:1 conduction ratio or higher); therefore, it cannot determine whether the PR interval is lengthening before blocked P waves (Figure 5C).
Third-degree AV block, or complete AV block, is characterized by complete dissociation between the atria and ventricles, with an atrial rate independent of a junctional or ventricular escape rhythm (Figure 5D).
Typically first-degree and Mobitz type I second-degree AV block are vagally mediated and will respond completely with sinus tachycardia to an atropine response test as described earlier. The higher-grade AV blocks are usually pathologic in origin, with the most common cause being idiopathic fibrosis of the cardiac conduction system. Although an atropine response test is still recommended, these often fail to respond. In such cases, especially in symptomatic patients, a pacemaker is indicated for definitive therapy. Some patients ventricular escape rates will respond transiently to theophylline (sympathomimetic) or pro-pantheline (antimuscarinic).
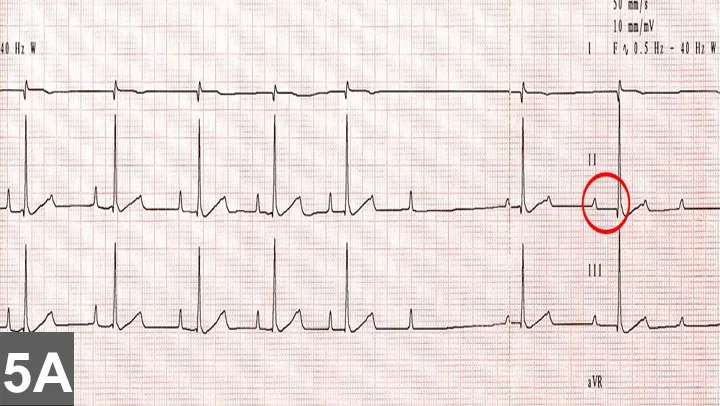
FIGURE 5A
Three-lead ECG in a dog with an auscultated arrhythmia. There is sinus rhythm with episodes of Mobitz type I second-degree AV block. Note prolongation of the PR interval before the last P wave that is blocked (circled) (paper speed, 50 mm/sec; sensitivity, 10 mm/mV).