Top 5 Antibiotics for Neurologic Infections in Dogs
Joseph M. Mankin, DVM, DACVIM (Neurology), Texas A&M University
Bacterial infections of the CNS can cause a variety of severe focal (eg, seizures, paresis) and multifocal (eg, multiple cranial nerve deficits, diffuse spinal pain) neurologic signs.1 Common bacterial isolates of CNS infections include Staphylococcus spp, Streptococcus spp, Pasteurella spp, and Escherichia coli.2,3
Common sources include extension of otitis media/interna, nasal sinus infection spread across the cribriform plate, diskospondylitis/vertebral osteomyelitis, and translocation from a distant pyogenic focus.4 Although these causes are not uncommon, the literature on appropriate antibiotic therapy for treating bacterial CNS infections in dogs is limited; general therapy recommendations are typically based on the small amount of literature in veterinary medicine as well as extrapolated from human medicine.
In any case of bacterial infection, culture and susceptibility testing should be conducted before beginning therapy; however, because of the difficulties encountered in sampling some parts of the CNS (ie, an anatomically inaccessible location), it may be difficult to obtain a proper diagnostic sample. Even if a proper sample is successfully acquired, clinical signs may progress rapidly before culture and susceptibility results are available; therefore, empirical therapy should be initiated as soon as possible.5 Initial therapy typically consists of a broad-spectrum antimicrobial with effective blood–brain barrier (BBB) penetration. In addition, combination therapy should be instituted to maximize coverage of the potential infectious cause.
The unique characteristics of the BBB limit drug penetration into the CNS, which can make selecting the appropriate antibiotic challenging. The BBB structure limits the movement of certain molecules from the vasculature to the CSF.2 Factors that play a role in BBB permeability include lipid solubility, molecular size, and protein-binding capacity. Lipophilic drugs reach higher concentrations in the brain, as they are able to diffuse across the membrane. Size and protein-binding capacity also play a role; most antibiotics bind to albumin, making it a much larger molecule and limiting the ability to diffuse across the BBB. In addition, the choroid plexus acts as an efflux system and actively removes drugs from the CSF.2 These characteristics must be taken into consideration when choosing an appropriate antibiotic.
The goal of antibiotic therapy is to choose a drug that readily crosses the BBB in active form and in adequate concentrations to have a therapeutic effect. When using time-dependent antimicrobials, the goal is to maintain CSF drug concentrations above the minimum bactericidal concentration for as long as possible. IV therapy should typically be administered for the first 3 to 5 days because CSF concentrations reflect that of the serum concentration2 and, in human medicine, early antibiotic therapy is associated with lower mortality.5,6 In addition, many patients with multifocal CNS signs may not be eating or may have a diminished gag or swallow reflex, which makes IV administration ideal. After the first 3 to 5 days of IV administration, the patient can be switched to an oral formulation.
In the author's opinion, the following antibiotics are feasible choices for treating bacterial infections of the CNS, depending on the underlying cause.
1. Cephalosporins
Most cephalosporins generally have excellent coverage against gram-positive pathogens, and most second- and third-generation cephalosporins have good gram-negative activity.2 Cephalosporins tend to have low lipophilicity and subsequently have poor BBB penetration. However, third-generation cephalosporins are more lipophilic, which allows them to more easily cross inflamed meninges.2 The mechanism of action is time-dependent and requires drug maintenance levels to be above the minimum inhibitory concentration for prolonged periods of time. The low toxicity of these drugs can be beneficial for cases in which high doses may need to be administered for longer periods.
The veterinary literature on cephalosporins that achieve high CNS levels is lacking.
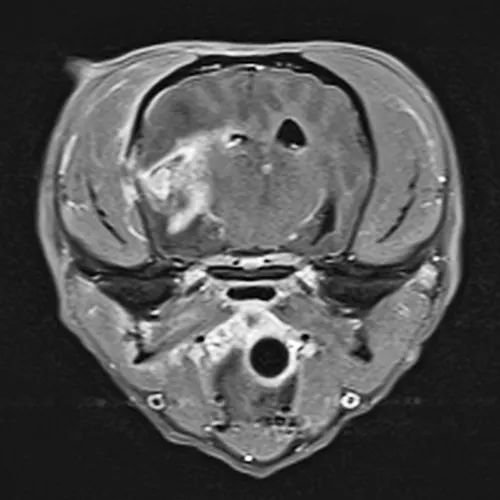
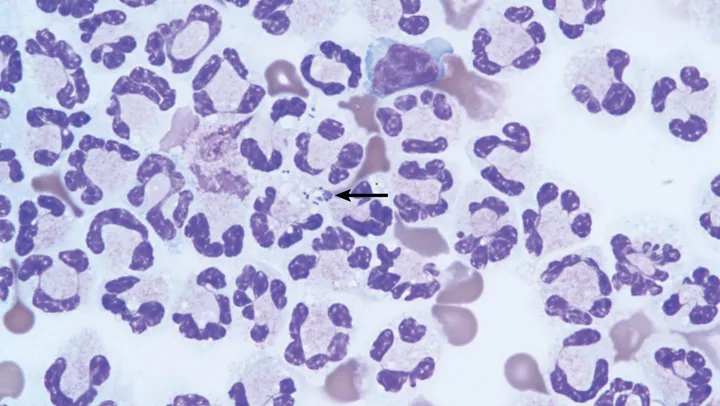
MRI showing postcontrast enhancement of a bacterial abscess and meningitis. There is also evidence of a fracture in the bone immediately adjacent to the abscess.
Cefotaxime (20-50 mg/kg IV q8h) is a third-generation cephalosporin that enters the CSF in therapeutic levels in patients with inflamed meninges7; however, use of this drug is considered extra-label. Other more commonly used third-generation cephalosporins include cefovecin and cefpodoxime; however, there is no published information about CNS penetration with these antibiotics.
2. Fluoroquinolones
Fluoroquinolones are moderately lipophilic, have low-to-moderate protein-binding capacity, and are of low molecular weight. All of these characteristics allow for good penetration into the CNS. Fluoroquinolones are typically used for treating gram-negative aerobic infections and also have bactericidal activity.2 Enrofloxacin (5-20 mg/kg PO q24h7) is a common choice, but marbofloxacin (2.75-5.5 mg/kg PO q24h7) can be substituted.
3. Metronidazole
Primarily used to treat anaerobic infections, metronidazole has bactericidal activity and readily penetrates the CNS. Drug levels in the CNS are high, reaching ≈90% of what is reached in the serum.8 Metronidazole is available in both injectable and oral formulations, which makes it a good choice when treating empirically.2 When administering metronidazole, however, the patient should be carefully monitored for side effects and/or adverse events, as high doses can lead to toxicosis and cause central vestibular signs. Other side effects and/or adverse events in dogs can include depression, mydriasis, proprioceptive deficits, tremors, and/or seizures.7 In patients exhibiting metronidazole toxicity, the administration of diazepam (0.4 mg/kg IV once followed by 0.4 mg/kg PO q8h for 3 days) has been shown to reduce the duration of clinical signs.9 Typically, metronidazole toxicosis is seen in cases with high doses (60 mg/kg/day) or with chronic use at lower doses (30 mg/kg/day).7,9
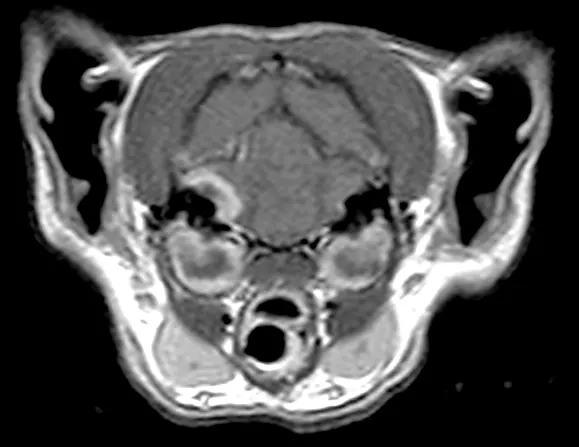
MRI of a patient with bilateral otitis media/interna. There is translocation of the infection across the bone invading the right side of the meninges.
4. Trimethoprim–Sulfonamide Combinations
Trimethoprim–sulfonamide is a drug combination that reaches therapeutic levels in the CNS, regardless of whether the BBB is inflamed or intact. The combination is bactericidal and can be considered as a first-line medication for treating presumed CNS infections.2,7 It has broad-spectrum coverage, with activity against both gram-positive and gram-negative organisms.7 Care should be used in patients with pre-existing hepatic or renal disease, as this drug combination is metabolized by the liver and unchanged when renally excreted. In these patients, a reduced dose could be considered. Patients should also be closely monitored for adverse events such as keratoconjunctivitis sicca and hypersensitivity. For patients receiving this combination long-term, routine Schirmer tear testing should be considered.
5. Ampicillin
Penicillins are a group of antibiotics that have low CNS penetration.7 Although concentrations increase as meningeal inflammation occurs,2 an efflux pump actively removes penicillins from the CNS, which results in lower concentrations. Ampicillin is the exception to this drug class, with high levels of CNS penetration being achieved despite the state of the BBB.2 Oral administration provides less drug absorption as compared with IV administration, so it is often recommended to initiate therapy with IV administration for the first 3 to 5 days then switch to another antibiotic for oral administration.
It is important to note, however, that the prevalence of β-lactamase production by Streptococcus spp and Enterobacteriaceae—leading causes of CNS infections—is high. Ampicillin would not be a good empirical choice in such cases and would only be worth considering when culture and susceptibility results indicate a non-β–lactamase–producing organism.
Conclusion
When choosing an antibiotic for treating a bacterial CNS infection, starting with a broad-spectrum, combination therapy approach is ideal. If the bacteria are isolated, the antibiotic regimen can be adjusted accordingly. If the patient is improving and no isolate is obtained, the current medication plan should be continued. The necessary length of therapy is unknown, but often resolution of clinical signs may take 6 to 8 weeks.10