Top 5 Anesthetic Complications
Kate Cummings, DVM, DACVAA, MedVet
Lois Wetmore, DVM, MS, ScD, DACVAA, Tufts University Cummings

Anesthetic management of small animal patients relies on thorough patient assessment, diligent anesthetic monitoring, and supportive care into recovery. Five complications that commonly occur during anesthesia include hypotension, hypothermia, abnormal heart rate (eg, bradyarrhythmias, tachyarrhythmias), hypoventilation, and difficult recovery (eg, prolonged duration, dysphoria, pain). Being prepared to treat anesthetic complications offers the best outcome.
1. Hypotension
The minimum acceptable mean arterial pressure for anesthetized small animals is 60 mm Hg.1,2 Blood pressure monitoring can be obtained indirectly with the use of Doppler and oscillometric devices or directly from a cannulated artery.
Some anesthetic drugs contribute significantly to hypotension. Inhalants cause a dose-dependent decrease in cardiac contractility and systemic vascular resistance.2-4 Acepromazine and propofol cause vasodilation.1,2 Using the lowest effective dose of an injectable agent and/or reducing the vaporizer setting will be the most beneficial in minimizing hypotension during the anesthetic event.
Alternative causes of hypotension that should be considered include blood loss, dehydration with inadequate volume replacement, other drugs (eg, angiotensin converting enzyme inhibitor), anaphylaxis, and histamine release.
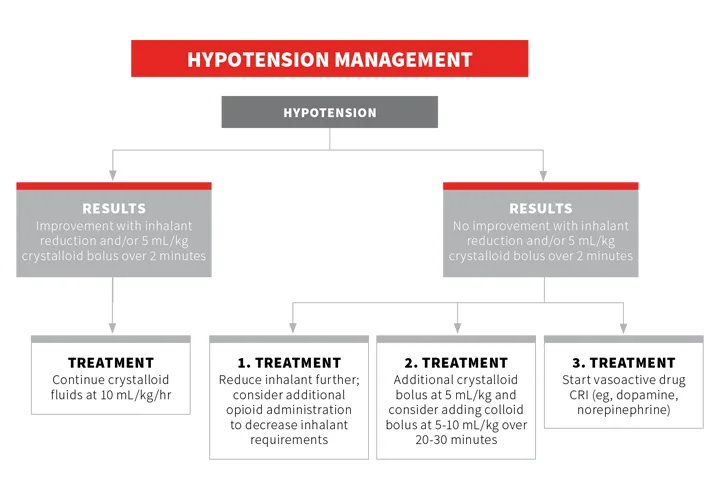
Therapies to address and respond to hypotension should incorporate a reduction in anesthetic depth when possible and/or crystalloid or colloid bolus(es); when refractory hypotension exists, intervention with vasopressors or positive inotropes should be considered (see HypotensionManagement).2-4
2. Hypothermia
A drop in temperature occurs during anesthesia as normal thermoregulation is disrupted and heat production is reduced.2,4 Direct anesthetic causes of hypothermia include α-2 adrenergic agonists via action at the α-2C receptor and opioids via action at opioid receptors in the hypothalamic thermoregulatory center.2 Acepromazine, inhalants, and induction agents such as propofol and alfaxalone decrease temperature because of vasodilation and/or as a result of slowing metabolism.1 Additional causes of hypothermia include IV fluids, shaved fur, open body cavities, high fresh gas (O2) flow rates, and surgical preparation solutions.
Hypothermia is known to have negative consequences on coagulation and overall immune function and can lower inhalant anesthetic requirements.5 During anesthesia, hypothermia can result in decreased drug requirements as metabolic rate is reduced.1,2,6,7 Bradycardia can also be a consequence of moderate-to-significant hypothermia caused by a reduction in automaticity of the sinoatrial and atrioventricular nodes.4,5 It is the author’s impression that anticholinergics (eg, glycopyrrolate, atropine) are often ineffective at treating such bradycardia when core body temperature is below 94°F (34.4°C).

Thermal injury in a cat after direct contact between the patient’s skin and a warm fluid bag. Burns occur when heating devices (eg, warm fluid bags, electric blankets) are placed in direct contact with patient skin or when insulation material (eg, towel, drape, hair) between the device and the patient becomes saturated with fluid. Photo courtesy of Dr. Cheryl Blaze.
Efforts should be made to insulate the patient from cold surfaces and sustain body temperature above 98°F (36.7°C). Warming devices that can be used to sustain body temperature or treat hypothermia should ideally be designated for use in veterinary and/or anesthetized human patients, and manufacturer directions for safe use should be followed (Figure 1).
3. Abnormal Heart Rate
Abnormal heart rate (HR) and arrhythmias are commonly observed during general anesthesia. Monitoring for arrhythmias via electrocardiography is crucial during the perianesthetic period, and in combination with direct auscultation, SpO2, and audible Doppler, comprehensive cardiovascular monitoring is provided.3
Bradycardia generally refers to heart rates <50 bpm in large dogs, <70 bpm in small dogs, and <100 bpm in cats.2,4,6-8 Bradycardias are generally a result of administration of vagotonic drugs (eg, α-2 adrenergic agonists or opioids), stimulation of vagally mediated reflexes (eg, oculocardiac reflex, intubation), hyperkalemia, or consequences of anesthesia, including excessive depth, hypothermia, and hypoxia.4,6-8 When the cause of bradycardia is increased vagal tone, an anticholinergic should be administered (eg, atropine, glycopyrrolate). Bradycardia is an expected reflex following α-2 administration and need not be treated unless hypotension and/or reduced peripheral perfusion become present. In that case, an α-2 antagonist should be administered first and given time to take effect before administering an anticholinergic. If the bradycardia is caused by excessive anesthetic depth, hypothermia, or hyperkalemia, the underlying cause should be corrected.
Tachycardia and tachyarrhythmias generally refer to HRs >200 bpm in cats and >160 bpm in dogs.2,4,6-8 The concern with significant increases in HR during general anesthesia is a reduction in filling time and stroke volume, impairing cardiovascular function.2,7
Anesthetic-related causes of sinus tachycardia are drugs (eg, ketamine, anticholinergics), inadequate depth of anesthesia, pain, or response to surgery, hypoxia, hypercapnia, or hypotension. Additional patient factors to consider include hyperthyroidism, heart disease, anemia, shock, pheochromocytoma, and anaphylaxis. Treatment of sinus tachycardia should focus on the cause. For example, in an animal that is painful, additional analgesia should be provided.
Intermittent and isolated ventricular premature complexes can be normal and harmless in healthy dogs and cats undergoing anesthesia. Intervention is generally not required unless irregular heart beats become more frequent (>20 irregular bpm), cause a reduction in BP, or transition to ventricular tachycardia. Again, treatment should focus on the source, but in the face of ventricular tachycardia, lidocaine is the primary therapy, followed by procainamide for refractory cases.2,7 Care should be taken to always dose reduce lidocaine in cats (see Table) given higher susceptibility to toxicity.
Table. Therapeutic Intervention for Anesthetic Complications
*Dose may create or worsen second degree AV block; if block does not resolve within 2–3 minutes, an additional dose of anticholinergic should be administered (0.005 mg/kg)
** Authors do NOT recommend use of a lidocaine CRI in cats.
4. Hypoventilation
Hypoventilation is generally drug-induced. Opioids, propofol, alfaxalone, and inhalants can result in a dose-dependent drop in respiratory rate; acepromazine and benzodiazepines can cause minimal respiratory depression.2,4,6,7 Other causes include impaired respiratory muscle effort (eg, rib fractures, pleural space disease, obesity) and upper airway obstruction common with brachycephalic airway syndrome and tracheal collapse. Ventilatory monitoring is best accomplished with the use of capnography with a normal end-tidal carbon dioxide of 35–45 mm Hg.2 This in combination with pulse oximetry provides more complete information of gas exchange at the level of the lung.
Normal respiratory rates for dogs and cats often vary based on size and positioning with most dogs breathing at 6–10 breaths/minute and cats at 16–20 breaths/minute. In a patient that is not spontaneously ventilating while under anesthesia, depth indicators should be assessed. If deemed adequate, the inhalant should be decreased. Intermittent manual and/or mechanical ventilation may need to be considered until spontaneous ventilation resumes.
5. Difficult Recovery
Patients should have continued close monitoring during the recovery period, as most anesthetic deaths occur during the postanesthetic period.8 Two of the more common recovery complications are 1) delayed recovery (>30 minutes since termination of gas anesthesia) and 2) rapid recovery with dysphoria with or without apparent pain.
A prolonged recovery often occurs from hypothermia or excessive drug effect. To correct hypothermia, appropriate measures should be taken to warm the patient. If a reversible anesthetic agent (eg, opioid, benzodiazepine, α-2 agonist) was used, drug reversal should be considered with the provision that adequate analgesia remains available.
In contrast to a delayed recovery, a rapid recovery often results in a subjectively distressed experience for the patient. Providing a quiet environment for recovery is important for the dysphoric pet. One must determine if the patient is having a rough recovery because of pain or dysphoria and/or agitation from residual effects of anesthetic drugs.3
With dysphoria alone, time often resolves clinical signs, but thrashing and fractious patients that remain restless (>5 minutes postextubation) may need administration of low-dose acepromazine or an α-2 adrenergic agonist. In animals that undergo long, potentially invasive surgical procedures, pain can contribute to a challenging recovery. In a painful patient, additional analgesia should be provided.