Surgical Repair of Traumatic Diaphragmatic Hernia
Daniel J. Lopez, DVM, University of Guelph
Ameet Singh, DVM, DVSc, DACVS (Small Animal), University of Guelph
Traumatic diaphragmatic hernia is an uncommon, underdiagnosed, and potentially life-threatening condition with a documented incidence of 6% in cases of blunt trauma.1
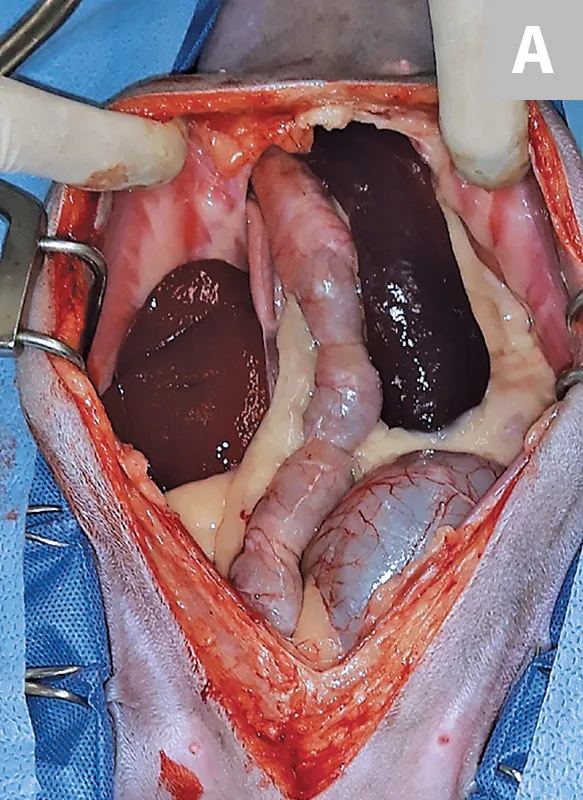
Figure 1 (A) Diaphragmatic hernia involving herniated liver, small intestine, colon, spleen, and mesentery in a 6-year-old spayed domestic shorthair cat.
Diaphragmatic hernia (Figures 1 and 2) has been categorized as acute (<14 days) or chronic (≥14 days) in the literature.2-4 In acute cases, initial stabilization of the patient and recognition of other underlying injuries are crucial. Higher mortality rates have been documented in animals with concurrent soft tissue injuries or in those with both soft tissue and orthopedic injuries.2

Diagnosis
Any patient with blunt trauma should undergo thoracic radiography to evaluate the integrity of the diaphragm and to identify other potential traumatic injuries such as pulmonary contusions, pneumothorax, pleural effusion, pneumomediastinum, or rib fractures (Figure 3). However, the integrity of the diaphragm and thoracic contents may be difficult to interpret, and additional modalities (eg, thoracic ultrasonography, CT; Figure 4) may be necessary for definitive diagnosis.5

CT evaluation of the abdomen and thorax in an approximately 2-year-old spayed crossbreed dog (positioned in dorsal recumbency) with elevated liver enzymes and suspected portosystemic shunt. Many small intestinal loops can be visualized, and the spleen is within the thoracic cavity. Chronic diaphragmatic hernia was diagnosed. (Ribs edited out for visualization)
Surgical Repair
Based on recent reports, definitive surgical repair (ie, herniorrhaphy) can be performed as soon as the patient demonstrates cardiovascular stability; previously, waiting at least 24 hours after presentation was recommended.2,3,6 However, patients with pulmonary contusions may benefit from delayed surgery, which can allow for resolution of pulmonary inflammation and hemorrhage (ie, contusions) and thus make the patient a better anesthetic candidate. Emergency surgery may be necessary in cases in which a herniated stomach distends (with or without volvulus) and results in respiratory distress that cannot be managed with thoracocentesis and/or oxygen support (Figure 5).7 In chronic diaphragmatic hernia patients, adhesions between abdominal contents and thoracic structures should be anticipated. In such cases, the surgeon should be prepared to perform a median sternotomy (following initial laparotomy) to improve exposure for adhesiolysis.
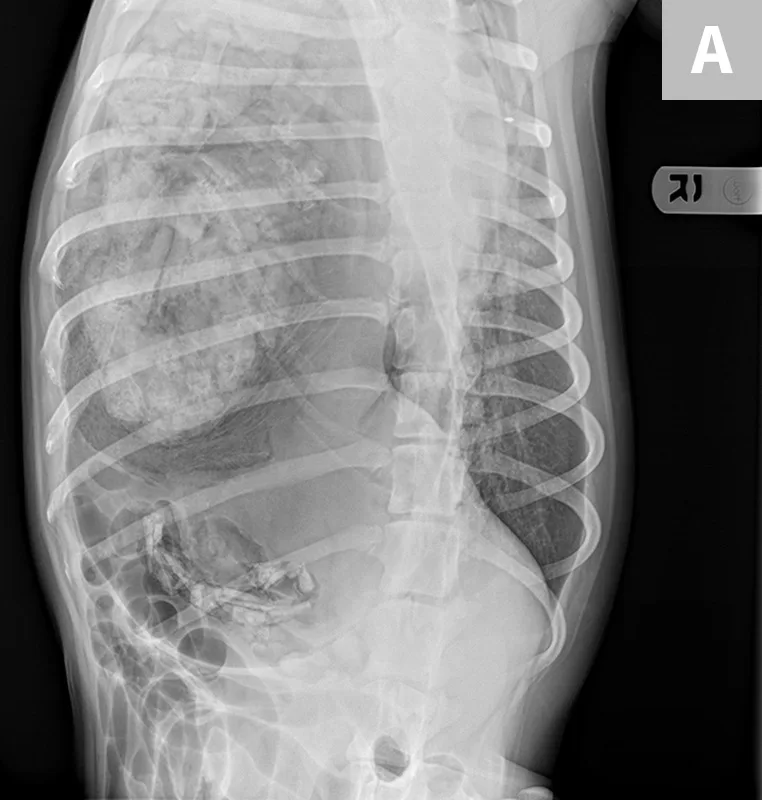
Figure 5 (A) Dorsoventral and (B) right lateral radiographs of a 1-year-old spayed dog with acute-onset respiratory distress resulting from gastric dilatation in the left pleural cavity. The dog had a history of trauma approximately 1 month before presentation. The stomach is dilated, and a large amount of gas and food content can be seen in the left hemithorax.
Step-by-Step
DIAPHRAGMATIC HERNIORRHAPHY
WHAT YOU WILL NEED
Recommended for Median Sternotomy (if needed)
Standard surgical instrument kit
Balfour retractor
Thoracostomy tubes or a thoracic drainage catheter
Bone saw
Osteotome and mallet
Orthopedic wire

Thoracic drainage catheter
STEP 1

Position the patient in dorsal recumbency, and anesthetize the patient with general anesthesia. Because of potential respiratory instability, make the transition from induction to intubation quickly and smoothly to minimize hypoxemia and hypoventilation. Use adequate anesthetic premedication and preoxygenation to minimize stress and maximize oxygenation before induction. Vasopressors (eg, dobutamine, norepinephrine) may be required to maintain blood pressure because of decreased intrathoracic venous return from intrathoracic abdominal organs.
Author Insight
Intermittent positive pressure ventilation is recommended because of the reduced pleural space and loss of negative pressure; however, to minimize barotrauma and the risk for re-expansion pulmonary edema, do not exceed a pressure of 15 to 20 cm H cl,ss="intro-deck">2sub>O. cl,ss="intro-deck">8sup>
STEP 2
Administer perioperative antibiotics (eg, cefazolin [22 mg/kg IV]) 30 minutes before making the incision and every 90 minutes thereafter until skin closure. In cases of chronic diaphragmatic hernia, the degree of adhesion formation will be unknown before surgery; therefore, clip, aseptically prepare, and drape the patient from pubis to manubrium for an exploratory laparotomy and median sternotomy in case increased exposure into the thoracic cavity is required.
Author Insight
Ensure an appropriately wide clip of fur is obtained. Drape the prepared area in anticipation of a thoracostomy, transabdominal, or transthoracic tube.
STEP 3
Perform a ventral midline laparotomy from the xiphoid process to the caudal aspect of the abdomen. Remove the falciform ligament to improve exposure of the cranial abdomen, then apply a Balfour retractor. Note the hernia size, location, organ involvement, and type (eg, radial and circumferential). Gently retract the abdominal organs to allow for repositioning into the abdominal cavity, if possible. Use caution, as the abdominal organs may have adhesions in the thoracic cavity.
Author Insight
Diaphragmatic hernia incarceration may occur if contraction of the hernia occurs over time and makes reduction of abdominal contents challenging. The hernia may need to be enlarged with scissors to allow safe retrieval of abdominal organs.
STEP 4
Adhesions may be present in the thoracic cavity in chronic diaphragmatic hernia patients. Break down adhesions using a combination of sharp–blunt dissection, electrocautery, and/or a vessel-sealing device. In a retrospective study, 14 of 50 chronic diaphragmatic hernia patients required resection of portions of the lung, liver, or intestine.4 Therefore, be prepared to perform lung or liver lobectomies (in addition to intestinal resection and anastomosis) due to adhesions.
If adhesion dissection cannot be performed through the diaphragmatic rent, or if increased exposure is required to perform organ resection, a median sternotomy may be needed. Transect the sternebrae longitudinally on the midline from the xiphoid to the second or third sternebra (depending on how much exposure is required) using a bone saw, osteotome and mallet, or, in young animals, heavy scissors.
Author Insight
If lung adhesions are present, performing a partial or complete lung lobectomy is recommended because of the reported complication of persistent pneumothorax from suspected incidental lung laceration during adhesion dissection.4 The authors prefer using a thoracoabdominal stapler for partial or complete lung lobectomy.
STEP 5
Repair the hernia using either long-acting absorbable (eg, polydioxanone) or nonabsorbable (eg, polypropylene) sutures. In chronic cases, use a scalpel blade to freshen the edges of the hernia to promote healing. For diaphragmatic tears that extend toward the cranial vena cava, begin herniorrhaphy dorsally and commence ventrally toward the laparotomy incision. Use a simple continuous or Ford interlocking pattern. In cases of diaphragmatic tears arising from the costal arch of the diaphragm, circumcostal sutures may be necessary to reattach the diaphragm to the body wall.
STEP 6
After completing the herniorrhaphy and returning abdominal contents to the abdomen, ensure viability of contents via complete abdominal exploration. Lavage the abdomen with warm, physiologic saline. Close the linea alba, subcutaneous tissues, and skin.
In some chronic diaphragmatic hernia cases, closure of the linea alba can be difficult because of the chronically decreased abdominal size. If a median sternotomy was made, close it with either orthopedic wire or heavy suture, depending on patient size.
Author Insights
If the abdominal contents are difficult to maintain within the abdomen because of loss of abdominal domain associated with chronic diaphragmatic hernia, organ resection may be required. Perform splenectomy followed by intestinal resection and anastomosis. Organ resection can reduce intra-abdominal pressure and wound tension to limit the risk for vascular compression and ischemia, which can cause abdominal compartment syndrome.9
There are several strategies for re-establishing negative pressure in the thoracic cavity. The authors prefer the use of thoracic drainage catheters because of their size and ease of placement. Drainage catheters should be placed before herniorrhaphy where visualization of the thoracic cavity can be achieved to allow for safe insertion.
STEP 7
Following hernia repair, perform aspiration to re-establish negative pressure of the thoracic cavity.
Postoperative Care
Radiography
Immediate postoperative radiographs should be obtained to document reduction of abdominal contents back into the abdomen and appropriate herniorrhaphy (Figure 6). Radiography is recommended 4 to 6 weeks postoperatively to ensure appropriate healing.

Lateral postoperative image documenting reduction of abdominal contents back into the abdomen and appropriate herniorrhaphy. Residual pneumothorax was apparent in this radiograph and was subsequently evacuated with the thoracic drainage catheter.
Pain Management
A multimodal approach that includes aggressive pain management is recommended. Opioid analgesia and nonsteroidal anti-inflammatory therapy (if there are no contraindications) are indicated.
Arterial Catheter
Measuring partial arterial oxygen concentrations outside of oxygen supplementation can be useful for serial monitoring of alveolar–arterial gradients and may be an early indicator of re-expansion pulmonary edema.
Thoracostomy Tube
Although all recommendations are empirical at this point, caution should be taken to completely and quickly empty the thoracic cavity of air to minimize the risk for re-expansion pulmonary edema. Recommendations for preventing re-expansion pulmonary edema include recovering the patient with a minimal pneumothorax and slow drainage over 8 to 12 hours until negative pressure is achieved.8
Thoracostomy tubes should be left in place for 48 to 72 hours postoperatively to monitor for persistent pneumothorax.
Antibiotic Therapy
Postoperative antibiotic therapy is generally not required following herniorrhaphy for uncomplicated diaphragmatic hernia.
Possible Complications
Possible postoperative complications include pneumothorax, hydrothorax, re-expansion pulmonary edema, abdominal compartment syndrome from loss of abdominal domain, and multiorgan dysfunction syndrome.
Prognosis
Prognosis following herniorrhaphy for both acute and chronic diaphragmatic hernia patients is good and has dramatically improved in recent reports, likely due to improvements in anesthesia and critical care practices.2-4,7