Severe Generalized Pyoderma in a Puppy
Maria Bell, DVM, Kansas State University
Lisa M. Pohlman, DVM, MS, DACVP, Kansas State University

Primary image courtesy of Elin Maki, Dog Coordinator at Riley County Humane Society
In this case report, the authors use applied cytology to evaluate and treat a shelter puppy with severe generalized pyoderma.
History
An ≈12-week-old male pit bull terrier was surrendered to an animal shelter because of severe skin disease that had worsened significantly over the past 2 weeks (Figure 1).

Shelter intake photo of an ≈12-week-old pit bull terrier puppy with generalized deep and superficial pyoderma. Photo courtesy of Elin Maki
Two weeks before relinquishing the puppy, the owners adopted him from a different animal shelter. The owners said the puppy did not have much hair at the time of the adoption, which the shelter staff had attributed to burns or extended sun exposure. Within days of adoption, the puppy’s skin became ulcerated and shortly after began to ooze and smell. The puppy’s appetite was good, and urination and defecation appeared normal.
Physical Examination
On presentation, the puppy was quiet and depressed but responsive. Temperature was 102.74°F (39.3°C), heart rate 136 beats/min, and respiratory rate 44 breaths/min. Marked, generalized alopecia with diffuse, severe erythema and large, oozing papules and ulcers was present; lesions were more severe over the ventrolateral neck and dorsal carpi. A serosanguineous/purulent exudate covered the majority of the puppy’s body. A thick, crusty, purulent exudate was also present in both ear canals.
Diagnostic Findings
Impression smears were obtained from the ulcerated skin of the ventral neck and dorsal carpi. Deep skin scrapings were obtained from the lateral thorax (bilaterally) and ventral neck. Swabs were obtained from both ear canals, and smears were prepared.
Related Article: Skin Scraping for External Parasites
Cytology
Cytologic evaluation of the stained impression smears (Figures 2 and 3) showed neutrophilic inflammation with intra- and extra-cellular cocci. Many large structures were noted, which ranged in size from ≈150 to 200 µm in length, did not take up the stain (ie, negatively stained), and had elongated, cigar-shaped bodies with 4 pairs of stubby legs attached to the thorax. Similar structures were noted on deep skin scrapings. Ear cytology revealed yeast structures consistent with Malassezia spp and cocci.
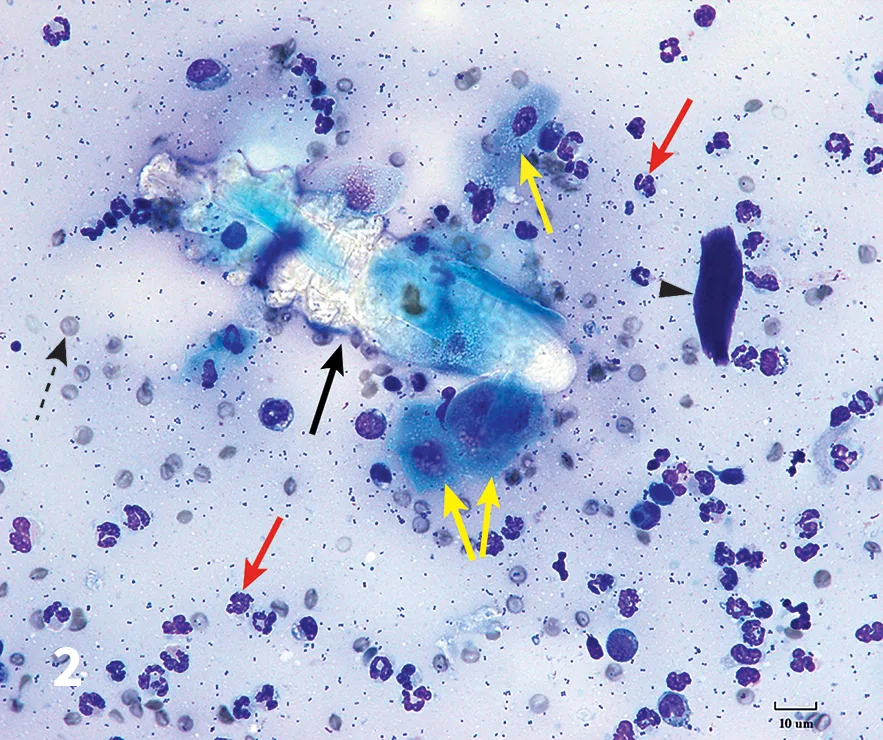
Figure 2.
Impression smear (Modified Wright’s stain) from ulcerated skin of the dorsal carpi. Note the Demodex spp nymph (black solid arrow), neutrophils (red arrows), squamous cells (yellow arrows), red blood cells (black dashed arrow), keratin bar (arrowhead), and bacteria in the background.
Treatment & Outcome
Treatment with ivermectin was initiated at 100 µg/kg PO then increased by an additional 100 µg/kg PO every 3 days to a final dose of 600 µg/kg PO once a day. The puppy’s ears were cleaned and treated with daily topical gentamicin–mometasone–clotrimazole ointment.
Two days after initial presentation, the puppy’s new foster family became concerned about his comfort level, so he was reexamined. Oral meloxicam (initial dose, 0.2 mg/kg, with subsequent doses of 0.1 mg/kg) once a day for 10 days was initiated for pain management. Ivermectin was discontinued because of administration difficulties, and afoxolaner was administered at 68 mg PO once a month for 3 months. Cephalexin was administered at 33 mg/kg twice a day for 4 weeks. The dog was reevaluated every 2 to 4 weeks.

The patient 3 months after start of treatment for generalized demodicosis with secondary, severe, deep, and superficial pyoderma. The dog had 2 consecutive negative skin scrapings 2 weeks apart.
At 90 days after treatment initiation, the puppy’s erythema, oozing, and alopecia were completely resolved (Figure 4). Two consecutive skin scrapings performed 2 weeks apart were negative. The puppy was neutered and placed for adoption.
Related Article: Treatment of Demodicosis in Dogs & Cats
Discussion
Small numbers of Demodex spp mites are considered normal in skin flora and do not typically cause clinical disease. Canine demodicosis occurs when large numbers of Demodex spp mites proliferate uncontrollably in the hair follicle and sebaceous glands. Mites are transmitted to puppies from the dam within 3 days of birth and spend their entire life cycle on their new host.
Clinical disease is not considered to be contagious but may be triggered by immunosuppression.1 Specifically, juvenile-onset, generalized demodicosis is believed to result from an inherited defect of the cell-mediated immune system, the main pathogenic mechanisms of which include rupture of the cutaneous barrier, inflammation, secondary (often severe) bacterial infection, and a type IV hypersensitivity reaction.1
Small numbers of Demodex spp mites are considered normal in skin flora and do not typically cause clinical disease.
However, not all mechanisms are present in every patient.1 The proposed theory of T-cell exhaustion is manifested by low production of supportive cytokines (eg, IL-2, IL-21) and increased production of suppressive cytokines (eg, IL-10 and transforming growth factor β).1 Also, many affected dogs have low numbers of circulating CD4+ lymphocytes.1
Changes in the up- and downregulation of cytokines combined with the observation that clinical disease does not usually recur following treatment (indicating recovery of T-cell function with time) support an immunopathologic hypothesis.1 The exact genetic link has not yet been determined, but it is strongly recommended that affected dogs not be bred.1
Related Article: Deep Skin Scrape
Historically, demodicosis treatment has been based around the use of amitraz dips.2 However, these dips are messy, and owner compliance can be low. Oral ivermectin may be administered, but dosing can be difficult and adverse events may occur, particularly in sensitive breeds. Treatment with moxidectin, topical imidacloprid–moxidectin, or milbemycin has been effective in some cases of generalized demodicosis.2
Two drugs recently introduced to the market, afoxolaner and fluralaner, have potentially made demodicosis treatment considerably easier and safer. Both are members of the isoxazoline class of long-acting systemic insecticides and acaricides, which act through selective noncompetitive GABA receptor inhibition.2 These drugs also bind to L-glutamate–gated chloride channels in muscle and nerve cells. A single dose of fluralaner has been proven effective for elimination of Demodex spp mites.2 In this case, afoxolaner was chosen based on availability.