Seizure Management in Dogs
Natasha Olby, VetMB, PhD, Diplomate ACVIM (Neurology), North Carolina State University

Profile
Definitions1, 2
Epileptic seizures are transient, involuntary events that result from paroxysmal, hypersynchronous neuronal discharges.
Epilepsy means recurrent seizures of any cause.
Primary (idiopathic) epilepsy: no underlying cause is identified and it is presumed to be genetic.
Secondary (symptomatic) epilepsy: seizures are a result of an abnormality within the brain (eg, brain tumor).
Cryptogenic or probable symptomatic epilepsy: seizures believed to be secondary but an etiology is not identified.
Reactive seizures result from an extracranial metabolic abnormality or toxicity such as hypoglycemia.
Cluster seizures: more than one seizure in 24 hours.
Status epilepticus: continuous seizures lasting for more than 30 minutes, or 2 or more seizures with incomplete recovery between seizures.
Diagnosis
There are numerous different causes of seizures. These are listed in Table 1, along with the most appropriate diagnostic test. Breeds of dog known to suffer from hereditary epilepsy are listed in Table 2.
Table 1: Differential Diagnoses and Definitive Diagnostic Tests for Seizures
* It is likely that genetic tests for inherited epilepsy will emerge in the next decade.
BP = blood pressure; Ca = calcium; CSF = cerebrospinal fluid; CT = computed tomography; EC = extracranial; IC = intracranial; MRI = magnetic resonance imaging; UA = urinalysis; US = ultrasound
Table 2: Breeds of Dog with Either Proven or Suspected Hereditary Epilepsy *
* Societies for many other breeds report epilepsy as a health problem. However, it is unclear how many of these dogs have received a diagnostic workup and had other causes for their seizures ruled out.
Treatment
Aim
Limit seizure frequency while avoiding adverse effects of AEDs.
When to Start Treatment
In view of the adverse side effects of AEDs, treatment is typically initiated when seizures occur more than once a month, or in clusters, or are associated with unacceptable postictal signs or with status epilepticus.
If an underlying cause of seizures is identified that could increase intracranial pressure (eg, brain tumor), treatment is initiated immediately as a seizure could be fatal.
Inpatient or Outpatient
Patients with cluster seizures or status epilepticus should be hospitalized for treatment. They can be released when they have been free of seizures for more than 24 hours.
Client Education
Clients should be informed that:
Seizure control is rarely perfect and as to what constitutes an acceptable seizure frequency for their pet.
Their pet may be unpredictable in the postictal phase of a seizure.
It is important to maintain a seizure diary.
AEDs have side effects and how to monitor for them.
They should never abruptly withdraw an AED because of the risk of causing refractory seizures.
Many AEDs are controlled drugs and must be stored carefully out of reach of children.
Drug Therapy
AEDs used are listed in Table 3 along with the suggested dose rate and range of therapeutic blood levels if known.2, 3, 4
First-line drugs are phenobarbital or potassium bromide.
Table 3: Drugs Used to Treat Epilepsy in Dogs
Phenobarbital2, 3, 5
Effective, inexpensive, readily available, and allows rapid control of seizures.
Contraindicated in animals with liver disease or those receiving drugs that inhibit cytochrome P450 (eg, ketocon-azole, cimetidine, chloramphenicol).
Side effects include PU/PD; polyphagia; sedation (transient at initiation of treatment, persistent at high blood levels); hepatoxicity (not reported in cats, more likely with blood levels > 35 µg/ml in dogs); blood dyscrasias (idiosyncratic reaction usually seen within the first 6 months of administration); induction of the cytochrome P450 enzyme system, causing increased metabolism of substances broken down with this system; and physical dependence.
Prior to starting treatment with phenobarbital, obtain a baseline evaluation of liver function by performing pre- and postprandial serum bile acid tests.
Check blood levels of phenobarbital 10 to 14 days after starting therapy or changing doses. Recent work has shown that blood samples for measurement of phenobarbital level can be taken at any time of day once steady state has been reached. However, some neurologists still prefer to measure trough levels.
Optimal blood levels are between 15 and 35 µg/ml. Doses need to be adjusted only if seizure control is poor or there are unacceptable side effects.
Doses can be adjusted according to the following equation:
Desired concentration/actual concentration × dose (mg) = new dose (mg)
Animals on phenobarbital should be monitored every 6 to 12 months:
Check seizure diary
Check phenobarbital blood levels
Check CBC and chemistry panel
An elevation in ALP is expected in dogs on phenobarbital.
Causes for concern about hepatotoxicity include a sudden dramatic elevation in ALT or a decrease in albumin, glucose, cholesterol, and/or BUN. If these changes occur, pre- and postprandial bile acid tests should be performed and potassium bromide therapy started with the ultimate aim of decreasing or even discontinuing phenobarbital therapy.
Neutropenia and/or thrombocytopenia could be due to phenobarbital and a full diagnostic workup of these problems should be performed immediately. If no cause is found, phenobarbital therapy should be discontinued and an alternative AED started.
Total thyroxine and free T4 levels are often low in dogs on phenobarbital due to increased rate of metabolism. Hypo-thyroidism should only be diagnosed in such animals if they have signs consistent with this disorder.
Potassium Bromide2, 3, 5
KBr is effective when used in combination with phenobarbital to control refractory seizures in dogs.6
KBr can be used as a single agent if seizure frequency is low or if phenobarbital use is contraindicated (eg, animals with liver disease or blood dyscrasias).
Contraindications include excessive sedation or PU/PD, renal disease, and history of pancreatitis or hyperlipidemia. If rapid control of seizures is needed (eg, animal presenting with cluster seizures), KBr is not an appropriate choice. Some neurologists feel KBr should not be used in animals with secondary epilepsy.
Side effects include PU/PD, polyphagia, gastrointestinal irritation, and lethargy. Administering KBr mixed with food may decrease GI irritation.
Severe intoxication can result in a wide variety of CNS signs, including pelvic limb weakness and ataxia, that progress to stupor. Blood levels can be decreased using an intravenous saline infusion.
There is a possible association between KBr use, hyperlipidemia, and pancreatitis.
KBr has a long half-life (15 to 68 days) that is influenced greatly by the amount of salt in the diet. The diet should therefore remain constant. Typically, the half-life ranges between 20 and 40 days.
Therapy can be started by loading over the course of one or five days or simply starting at the maintenance dose (Table 3), depending on how quickly therapeutic serum levels are needed.
Desired serum levels range from 1000 to 3000 mg/L. The blood level at which sedation and ataxia are seen varies widely between individuals, but these side effects are likely to occur with blood levels > 3000 mg/L when used as monotherapy and > 2500 mg/L when used in combination with phenobarbital.
Blood levels should be checked approximately 3 months after starting maintenance therapy and every 6 to 12 months thereafter. If a loading dose was used, measure blood levels immediately after loading and again in 1 to 3 months to ensure they are remaining constant.
Changes in dose can be calculated using the following equation2: Target blood level (mg/L) - actual blood level (mg/L) × 0.02 = amount to be added to daily dose (mg/kg)
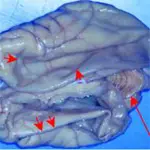
The brain of a dog diagnosed with hydrocephalus. The cerebellum is normal in appearance (long arrow), but the cerebral cortex is very thin.When the cranial cavity was opened, the dilated lateral ventricles collapsed, causing the thin layer of cortical tissue to fold in on itself (short arrows).
Refractory Epilepsy
In some cases, KBr and phenobarbital do not provide adequate seizure control, or cause unwanted side effects including sedation and hepatotoxicity.
The first step is to get control of seizures by adding a third drug (Table 3).2, 3, 4 Select a drug with a different spectrum of side effects and a different mechanism of action.
Once control has been achieved, one of the drugs can be slowly decreased to try to limit the side effects.
AEDs should always be decreased gradually: reduce the dose of one drug by 10% to 20% per 1 to 4 weeks (depending on the circumstances) until either the unwanted side effects have resolved or seizure control deteriorates.
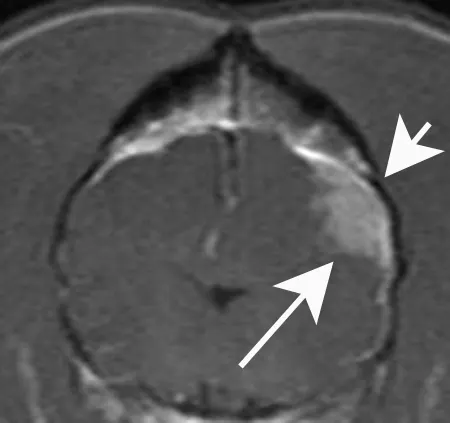
A transverse postcontrast T1- weighted MRI of the brain of a dog with a meningioma that caused seizures. The tumor is clearly evident as a homogeneously enhancing mass (long arrow). Note that the skull directly over the mass is increased in thickness (short arrow), a common finding with meningiomas.
Agents to Be Added On
Benzodiazepines
Oral diazepam is ineffective as a maintenance drug in dogs.
Clorazepate is a benzodiazepine that can be used for seizures in dogs (Table 3).2
Felbamate (Felbatol-Medpointe Pharmaceuticals)
Has been used in dogs as monotherapy for partial seizures in addition to add-on therapy in refractory epilepsy.7
Does not cause sedation.
Is metabolized by the liver (cytochrome P450) and causes hepatotoxicity and aplastic anemia in humans. These side effects have not been reported in dogs as yet, but felbamate is contraindicated in dogs with liver disease.
Should be monitored with a CBC and serum biochemistry panel after 1 month and then every 3 months.
Gabapentin (Neurontin-Pfizer)
Is a useful AED because it is excreted renally and does not cause hepatotoxicity.
Of unknown efficacy, although a single report suggests it reduces seizure frequency in refractory cases.8
Rapidly reaches steady state levels, so doses can be adjusted every 1 to 2 weeks in animals that continue to seize.
May cause sedation in some animals.
Is expensive and needs to be administered 3 times a day, if possible.
Levetiracetam (Keppra-UCB Pharma, Inc.)
Does not cause sedation, although the full range of side effects in dogs is unknown.
Efficacy in dogs is currently unknown.
Is expensive.
Topiramate (Topomax-Ortho-McNeil Neutrologics, Inc.)
Is a safe drug in humans, with few adverse effects noted. The adverse effects in dogs have not been reported.
Reports of use in veterinary patients are purely anecdotal at this time.
Shown to have an elimination half-life of 2 to 3.8 hours by pharmacokinetic study in beagles.
Zonisamide (Zonegran-Dainippon Pharmaceutical Co.)
Is a relatively new drug in the U.S., but has been used for a number of years in Japan and Europe.
It is a useful drug in cases of refractory epilepsy according to a single report.9
Has been reported to cause adverse effects in humans including renal calculus formation, sedation, and gastrointestinal disorders. However, little is yet known about the spectrum of side effects in dogs.
Is expensive.
Vagal Nerve Stimulation
Stimulation of the vagal nerve by an implanted device is effective for controlling seizures in humans.
A phase-one clinical trial in dogs using human devices showed that they were safe and decreased seizure frequency in half the dogs evaluated.10
The devices are extremely expensive.
Tx at a Glance
Complete appropriate diagnostic workup.
Assess seizure frequency for need of AEDs.
Start on phenobarbital or KBr.
Check blood levels and response to therapy at appropriate time for drug.
Alter dose according to blood levels, presence of side effects, and seizure control.
Continue to monitor every 6 to 12 months.
If seizure frequency too high and blood levels optimized, add in another drug (either phenobarbital or KBr).
Continue monitoring as before.
If seizure frequency too high or adverse side effects present, add in a third drug.
Once seizures controlled, if adverse effects present, start to taper phenobarbital or KBr slowly to reduce side effects.
Management of Cluster Seizures
Cluster seizures are a common emergency in dogs with refractory epilepsy.2
Repeated visits to the emergency clinic are impractical, very expensive for the owner, and may result in euthanasia.
Owners should be given an individualized plan describing additional therapies they can administer at home and clearly stating when they should seek emergency care.
Use of phenobarbital: An additional full dose of phenobarbital can be administered after a seizure, when the dog is awake enough to swallow. This can be repeated after each additional seizure as long as it is not given more than once per hour. If 3 additional doses have been given in a 24-hour period and the animal has another seizure, veterinary help should be sought.
Use of diazepam: An alternative approach is to use diazepam administered per rectum by the owner. This is particularly appropriate in dogs with prolonged seizures or a tendency to develop status epilepticus. The owner must be carefully taught how to draw up and administer the diazepam. Do not dispense diazepam in a plastic syringe as it is light sensitive and adheres to plastic. The dose is 2 mg/kg in dogs on phenobarbital and 1 mg/kg in dogs that are not being treated with phenobarbital. If 3 doses have been given in a 24-hour period and the dog has another seizure, veterinary help should be sought.2
Follow-up
Patient Monitoring
Epileptic dogs should be monitored every 6 to 12 months depending on seizure frequency and AED therapy.
Maintaining an accurate seizure log in the patient's record is important.
Requirements for monitoring specific to each AED are noted under Drug Therapy.
Nutritional Aspects
One of the most common side effects of AED therapy is polyphagia. Owners must be warned about this and counseled on weight control for their pet.
If a pet's appetite becomes unmanageable, it may be necessary to try a different AED (Table 3).
When using KBr, the salt content of the diet must be kept constant. If a dietary change is necessary, monitor KBr levels monthly over the subsequent 3 months to determine whether a dosage change is necessary.
If dogs develop fasting hyperlipidemia on AEDs, this should be treated using a low-fat diet.
In General
Relative Cost
A full neurologic workup is very expensive. $$$
Hospitalization for management of a cluster of seizures is expensive. $$-$$$ (depending on duration of stay and intensity of management.)
Cost of long-term treatment is extremely variable depending on success of treatment. The cost for the following drugs is listed per month for a 30-kg dog.
Zonisamide: expensive - $$
Felbamate: expensive - $$
Levetiracetam: expensive - $$
Topiramate: expensive - $$
Clorazepate: inexpensive - $
Gabapentin: inexpensive - $
KBr: inexpensive - $
Phenobarbital: inexpensive - $
Cost Key
$ = <$100
$$ = $100-$250
$$$ = $250-$500
$$$$ = $500-$1,000
$$$$$ = >$1,000
(Actual costs will have regional variations)