Scrotal Approach to Canine Orchiectomy
Brian A. DiGangi, DVM, MS, DABVP, University of Florida
Matthew D. Johnson, DVM, MVSc, DACVS (Small Animal), ACVS Fellow of Minimally Invasive Surgery (Small Animal Orthopedics), University of Florida
Natalie Isaza, DVM, University of Florida

Both prescrotal and perineal approaches to castration of adult dogs have been described in the literature. The prescrotal technique can be used more frequently because it is easier to exteriorize the testicles and spermatic cords.1 A scrotal approach is preferred for castration of cats, small mammals, large and small ruminants, horses, and pigs.1-6 A scrotal approach for castrating adult dogs has also been used to safely castrate dogs of any age.7,8 In dogs, this approach offers advantages that include improved cosmesis and decreases in anesthetic and surgical times, incision length and subsequent surgical trauma, postoperative discomfort and self-trauma, and scrotal hematoma formation.7-11
In a study comparing postoperative complications of adult dogs castrated through prescrotal and scrotal approaches, no difference in the occurrence of hemorrhage, pain, or swelling was noted 72 hours after the procedure.10,11 The scrotal approach had significantly reduced odds of self-trauma and a 30% reduction in surgical time.10,11 In the authors’ clinical training program, junior and senior veterinary students have performed 984 scrotal castrations in adult dogs between 2010 and 2014. A total of 11 postoperative complications were identified, all the result of factors independent of the surgical approach (eg, postoperative hemorrhage caused by incomplete ligation of the spermatic cord).
Patient Selection
Patients selected for scrotal castration should undergo the same screening as for any other elective surgical procedure; they should be free from severe systemic disease that would prohibit administration of anesthesia, and caregivers must be willing to provide standard postoperative care. Removal of cryptorchid testicles should not be attempted via a scrotal approach; however, in dogs with unilateral cryptorchidism, the fully descended testicle may be removed via a scrotal approach. Other contraindications to the scrotal approach include pyoderma, abscessation, trauma, or ischemia of scrotal tissue.
The postoperative environment should also be assessed. Because of the anatomical position of the canine scrotum, the scrotal incision site could come into contact with the ground when the patient is in a sitting or lying position. A clean, dry environment for at least the first 3 postoperative days is recommended to minimize the occurrence of surgical site contamination (see Contraindications to Scrotal Approach for Elective Canine Castration).
Contraindications to Scrotal Approach for Elective Canine Castration
Bilateral cryptorchidism
Pyoderma, trauma, abscessation, or ischemia of scrotal tissue
Known unsanitary postoperative environment
Benefits & Drawbacks
A scrotal approach to canine castration can be performed on any dog for which prescrotal castration is appropriate. In the authors’ experience, the procedure carries the benefits of reduced time to locate, manipulate, and isolate the testicle prior to the initial incision as well as reduced time in closing the incision. In most cases, incision length is smaller than in prescrotal castrations because of the increased mobility and maneuverability of the testicle in the scrotal (vs prescrotal) position. In addition, the scrotal skin is more elastic, allowing for easier exteriorization of the testicle through a smaller incision as the skin stretches. These improvements in surgical efficiency translate into reduced anesthetic and surgical times, factors well-correlated with reduced risk for surgical-site infections.12,13 The risk for inadvertent ligation or accidental laceration of the urethra during closure of a prescrotal castration is eliminated with the scrotal approach; in addition, less suture is implanted, resulting in decreased procedural cost.
Another benefit of the scrotal approach becomes apparent in the event of incomplete ligation of the spermatic cord resulting in postoperative hemorrhage. As the incision is only partially closed, postoperative hemorrhage is readily identified and can often be addressed through the existing surgical site. Postoperative hemorrhage in a patient that underwent an alternate castration approach is often more difficult to detect until the scrotum begins to swell. The authors have not encountered a case of postoperative hemorrhage in which the spermatic cord retracted into the abdomen and was not retrievable through the original surgical site; this is likely secondary to the comparatively more distal location of spermatic cord ligation with the scrotal approach.
The major disadvantage of a scrotal approach is the likelihood of a small amount of postoperative drainage, which many pet owners would find objectionable. Continuous drainage of frank blood or the presence of blood clots suggests the need for reassessment. Gentle tissue handling, a vasoconstrictive splash block (eg, 1 part epinephrine [1 mg/mL] to 9 parts 2% lidocaine), and a scrotal wrap can help minimize this occurrence (Table). Such drainage should cease by the time the patient is discharged (ie, within a few hours), particularly if patients are hospitalized postoperatively.
Table: Benefits & Drawbacks of a Scrotal Approach for Elective Canine Castration
Related Article: The Case: "Routine" Dog Neuter That Has Gone Awry
Step-By-Step: Scrotal Approach to Canine Orchiectomy
What You Will Need
Small-sized, low-powered, electric clippers
Antiseptic scrub
Sterile surgical castration pack
Surgical drapes
4 Huck towels
4 towel clamps
Operating room scissors
4×4 gauze
Carmalt or mosquito forceps
Needle drivers
Thumb forceps
#10 or #15 surgical blade
Sterile gloves
0, 2-0, or 3-0 monofilament suture
Green tattoo ink and tissue adhesive
Optional:
Clean 3”×3”gauze square and self-adherent bandaging tape
9:1 mixture of 2% lidocaine and epinephrine (1 mg/mL)

Small, low-powered clippers appropriate for use in clipping scrotal hair (shown with a 22-gauge, 1-inch, over-the-needle, IV catheter for size comparison)
Step 1
Aseptically prepare the surgical site by clipping an area around and including the scrotum; scrub with an appropriate antiseptic. To ensure a smooth surface and adequate contact of antiseptic with the surgical site, hold the testicles taut against the scrotal skin while performing the scrub.
Care should be taken to avoid dermatitis, or “clipper burn,” while clipping scrotal tissue. It is not necessary to completely remove every hair; clipping should focus on the removal of long, dense hairs that may contaminate the surgical field. When clipping over the scrotum, grasp the testicles away from the body to pull the skin taut and allow adequate contact of scrotal hair with the clipper blade.
Author Insight Use small-sized, low-powered, electric clippers to minimize trauma to the scrotal skin during clipping.
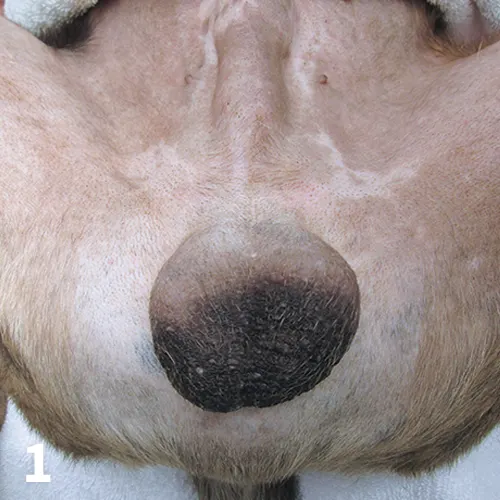
Surgical site clipped for scrotal castration.
Step 2
Once the scrotum is aseptically draped, gently grasp 1 of the testicles and direct it caudoventrally and away from the body to pull the scrotal skin taut over the testicle. Incise the ventral-most surface of the testicle just lateral to the median raphe. Take care to avoid incising the epididymis. An incision approximately one-third of the length of the long axis of the testicle will be required to exteriorize the testicle.
Author Insight If 1 testicle lies more cranially than the other, remove the more cranial testicle first. Doing so takes advantage of the greater mobility of the second, more caudal, testicle when moving it cranially toward the initial incision for exteriorization.

An incision is made just lateral to the median raphe, directly over the first testicle to be removed.
Step 3
Once the initial incision is made, the procedure continues as with any other castration technique. Bluntly (manually) or sharply dissect the spermatic fascia and scrotal ligament until the spermatic cord is isolated from all visible connective tissue. Open, modified-open, and closed castration techniques can all be used with the scrotal approach. After ligation of the spermatic cord and confirmation of hemostasis, replace the cord deep within the scrotum. The number and type of ligatures placed along with suture size and type are all left to surgeon discretion.
Author Insight
When manually disrupting the layers of spermatic fascia and scrotal ligament, take care not to pinch the scrotal tissue to avoid unnecessary discomfort, bruising, and subsequent postoperative self-trauma. In large and/or older adult dogs, a combination of sharp and blunt dissection of the spermatic fascia is recommended.
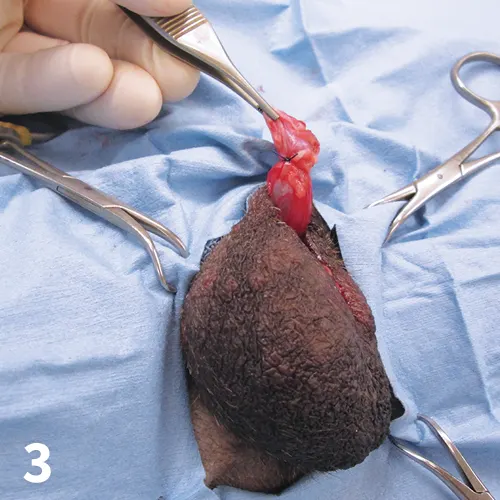
The first spermatic cord is ligated and hemostasis is confirmed. Note that a closed castration is depicted.
Step 4
Grasp the second testicle and hold it directly underneath the site of the initial skin incision. Incise the scrotal septum and spermatic fascia to expose the parietal vaginal tunic. Exteriorize and remove the second testicle as described in Step 3.
At the surgeon’s discretion, the incision may be partially closed by the placement of 1 interrupted suture in the dartos fascia using absorbable, monofilament suture. Care should be taken not to grasp the scrotal skin with thumb forceps while placing the suture and the knot should be inverted. In general, the suture selected for ligation of the spermatic cord is appropriate for closure as described here. The goal of suture placement is gentle apposition of the incision site (not ligation of tissue or complete incisional closure) to promote rapid healing, serve as a barrier against surgical site contamination, and reduce postoperative self-trauma.

The second testicle is directed toward the initial incision prior to incision through the spermatic fascia and exteriorization.
Step 5
Gently, manually invert the incision deep within the scrotal area to serve as an additional barrier to environmental contamination and improve cosmesis. Everting of the incision as is often done after scrotal orchiectomy in other species (eg, cats) is not recommended because of the anatomical position of the canine scrotum.
Because of lack of a visible surgical scar after wound healing, it is important to place a tattoo in the prescrotal region to identify the dog as surgically sterilized. The prescrotal region is preferred to ensure visualization of the tattoo (and recognition of the dog as neutered) should a future surgeon attempt a prescrotal or caudal abdominal approach in suspicion of retained testicles.15 Score the skin with the scalpel blade, place a small amount of tattoo ink within the scored area, pinch the skin closed, and apply a drop of tissue glue to prevent the ink from being licked or transferred into the environment.
Author Insight
Do not attempt to fully close the dartos fascia, intradermal, and/or cutaneous layers of the incision with sutures, as this can lead to discomfort, seroma formation, self-trauma, and postoperative complications.14
Placement of a vasoconstrictive splash block (consisting of 1 part epinephrine [1 mg/mL] to 9 parts 2% lidocaine) prior to closure may provide additional analgesia and help minimize any post-operative drainage.
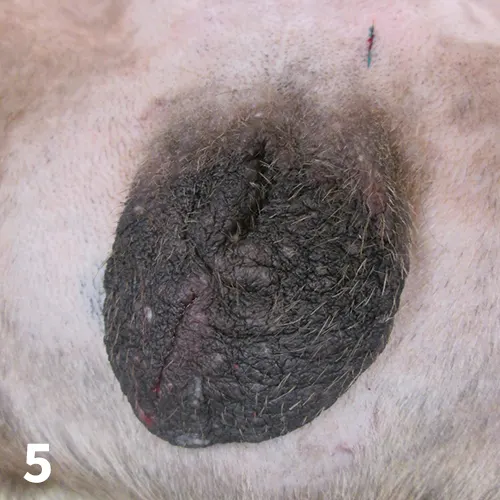
The incision site is inverted and invisible after completion of the procedure. Note the application of a tattoo in the prescrotal region permanently identifying the dog as surgically sterilized.
Step 6
A small amount of serosanguinous fluid draining from the surgical site is expected for the first few hours after the procedure. In large dogs, or those with a pendulous scrotum, place a small piece of clean gauze directly over the surgical site and wrap it securely with self-adhesive bandage material (eg, 3M VetRap). This scrotal wrap will apply compression to reduce any drainage and allow for the collection, quantification, and assessment of any drainage that does occur. Additionally, it can provide hemostasis of scrotal vasculature and prevent environmental contamination and self-trauma.
The scrotal wrap should not be left in place for more than a few hours and, if still in place, must be removed prior to patient discharge to prevent accidental ingestion, pressure necrosis and delayed wound healing, or caregiver injury while attempting to remove the wrap. As with any castration approach, standard postoperative instructions (eg, observing a period of exercise restriction, regular monitoring of the surgical site) are recommended.

A scrotal wrap has been placed to apply compression, collect any postoperative discharge, and protect the surgical site.