The Role of the Glucose Curve
Definition: The glucose curve (GC) portrays the temporal changes in blood glucose that occur throughout the day. For diabetic patients, the GC is analyzed in response to administration of exogenous insulin.
The GC is used in diabetic patients to represent the time–action profile (a pharmacodynamic property) of insulin on the circulating blood glucose concentration.
The GC reflects the global physiologic effects of insulin on serum glucose but does not discriminate between individual insulin effects.
Serum glucose, at any single time point during the GC, represents the sum effects in the rate of:
Exogenous insulin absorption
Intracellular uptake of exogenous and endogenous insulin
Insulin degradation and elimination
Intestinal glucose absorption
Endogenous glucose production
Tissue glucose uptake and utilization.
IndicationsThe GC is indicated when a pharmacodynamic assessment of a patient’s response to exogenous insulin administration is needed. Other uses may apply in hypoglycemic animals or hospitalized patients.
The GC is frequently included as part of a long-term monitoring strategy to assess glycemic control in diabetic dogs and cats. In theory, an accurate time–action profile of an individual patient’s insulin dose can be obtained by using the GC. The information provided by the GC can aid in evaluating the efficacy of insulin therapy and assessing future insulin needs. Clinicians should be familiar with the advantages and disadvantages of the GC as a diagnostic tool for evaluating diabetic control.
See Poor Glycemic Control in a Diabetic Dog
Examination & AssessmentA complete patient history and physical examination should be carried out before performing a GC; patient information gathered from history and examination will be needed to fully interpret the GC result.
Ancillary laboratory evaluations may be indicated:
Periodic laboratory evaluation (eg, complete blood count, serum biochemical profile, and urinalysis) may assist in diabetic monitoring and can alert the clinician to the presence of comorbid diseases.
Fructosamine level can provide information about long-term glucose control to complement information obtained from the GC.
The need for additional testing (eg, urine cultures, thyroid function tests, and adrenal function tests) can be determined on an individual basis.
ApplicationThe GC is most useful for determining a patient’s response to a dose of exogenous insulin. The patient should be previously acclimated to the administered insulin dose.
In clinical settings, the GC is typically used for monitoring insulin therapy in previously diagnosed diabetic dogs. The GC is not usually used to diagnose diabetes mellitus or to evaluate suspected insulin-resistant states.
Several protocols for performing the GC on dogs and cats have been described:
Acceptable methods include curves performed in the hospital or at home. In these settings, samples may be obtained, respectively, by veterinary personnel or by the pet owner.
In-hospital curves may use an indwelling venous catheter method or repeat venipuncture method to obtain samples.
Home sampling is usually performed using a lancet to obtain capillary blood, but venous sampling may be appropriate in some circumstances.
See Home Monitoring of Diabetic Patients
Testing of samples is usually performed using a portable glucometer.
Continuous blood glucose monitoring (CBGM) is becoming more common as a method to perform the GC in veterinary patients. Real-time CBGM uses a wireless subcutaneous sensor and a portable receiver to provide glucose measurements every 5 minutes for up to 72 hours.
Many clinicians perform a 12- to 18-hour GC, depending on insulin type and dose frequency. The shorter GC is more practical than a 24-hour curve for many veterinary practices.
Regardless of the method chosen, personnel must be trained to carry out the GC using a consistent protocol. Familiarity with the advantages and disadvantages of the selected method will improve the diagnostic performance of the GC and minimize treatment decision errors that can arise from inaccurate GC results.
Sampling Techniques
Some clinicians use small-gauge needles or disposable lancets to obtain small-volume venous blood samples (< 0.1 mL/sample) for glucose measurements every 1 to 2 hours. A venous sampling catheter may also be placed in the patient to minimize patient stress and facilitate the frequent sampling needed to complete a GC. In the past decade, published and anecdotal reports have suggested that owners of diabetic pets can be instructed in proper capillary blood sampling techniques, allowing owners to perform the GC at home.
ComplicationsThe GC procedure is safe and has a very low complication rate. Potential complications include:
Injury associated with venous catheter placement or sample acquisition
Phlebitis or dermatologic injury to the area for sampling due to repeated venipuncture samples
Hypoglycemia due to exogenous insulin administration (but not due to the GC procedure).
Failure to adhere to the patient’s insulin protocol may produce a GC that does not reflect the patient’s normal situation. Insulin administered at an incorrect dose, injected into a different skin site, or variation in the time of administration are potential errors that can affect GC accuracy. Feeding a different diet during the GC may have similar detrimental effects on the quality of the data. Variability in the GC arises from several sources, including:
Human error (in acquiring or analyzing the sample)
Laboratory error
Biologic variability (due to variations in insulin absorption, physiologic responses, dietary intake, or concurrent pathologies).
An indirect complication of the GC is the intrinsic variability of the glucose readings on a day-to-day basis.
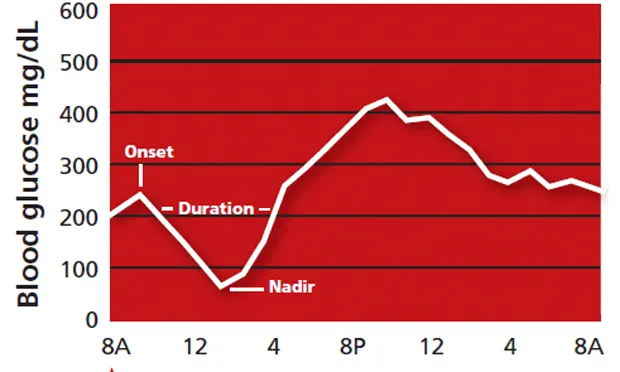
Evaluation & InterpretationFeatures of the curve that should be evaluated when possible are shown in Figure 1. Salient features include the time of insulin onset, duration of effect, and peak insulin effect (the glucose nadir).
Periods of subclinical hypo- or hyperglycemia may be detected over the period of the GC. The GC should be ended if clinical signs or severe biochemical hypoglycemia develop. As illustrated in Figure 1, the period of hyperglycemia that follows a period of hypoglycemia, whether caused by a physiologic counter-regulatory response or the administration of exogenous glucose, obviates the need for additional sampling because additional data provide no useful information.
A 24-hour glucose curve: Clinical information that can be gleaned from the GC includes onset of insulin action, duration of insulin efffect, and glucose nadir. Time of onset is determined by the first glucose reading that is less than the preinjection value; duration of insulin effect is measured from the onset time until the glucose value equals or exceeds preinjection glucose level; glucose nadir is the lowest glucose concentration detected during the GC.
The results of the GC must be interpreted in light of other clinical parameters:
Recent patient history and presence or absence of clinical signs of diabetes
Physical examination, especially body weight and condition, and presence or absence of diabetic complications
Laboratory tests, especially the fructosamine level.
When interpreting the GC, keep in mind its potential drawbacks. If the GC result is inconsistent with the overall clinical picture, it should be scrutinized carefully before it is accepted. Interpretive errors are more likely when too much weight is given to just one of the parameters used to evaluate a diabetic patient.
Future ConsiderationsDevelopment of less invasive and continuous methods to accurately and precisely determine blood glucose concentrations will improve diabetic monitoring and may replace the GC as it is currently performed.
Relative Cost$$–$$$: Costs of performing a GC vary with the method chosen (intermittent direct sampling versus continuous glucose monitoring), sampling frequency, and the machine used to measure blood glucose.
For related articles, please see the following:Switching to Another Insulin: What & HowBlood Glucose MonitorsAdvances in Glucose Monitoring