Repairing Diaphragmatic Hernia
WHAT YOU WILL NEED
• Oxygen• Thoracic radiographs• A ventilator or an anesthetist to hand-ventilate during surgery• Pulse oximetry• Capnometry or blood gas analyzer• Assistant• Self-retaining Balfour retractor• Thoracostomy tube• Nonabsorbable monofilament suture• Nonabsorbable mesh (in the rare cases that there is insufficient tissue to close the defect)• If a median sternotomy is indicated:- Sagital saw to cut sternebrae- Orthopedic wire, wire cutters to close
Diaphragmatic hernias in companion animals can be acquired or congenital. Acquired hernias most frequently result from blunt thoracic or abdominal trauma. Both acquired and congenital hernias may be clinically inapparent for years or may cause acute, life-threatening emergencies. Displacement of abdominal organs into the thorax can result in hypoventilation because of compression of the lungs, effusion of fluid due to liver entrapment, or loss of negative intrathoracic pressure. Whether the defect in the diaphragm is acute or chronic, traumatic, or congenital in nature, there are several key principles to consider when repairing the hernia.
Procedure PearlRepairing diaphragmatic hernia is often not a surgical emergency and can wait until other problems are addressed; however, surgery should not be delayed in animals that are severely dyspneic or that may have strangulated bowel within the diaphragmatic defect.
Patients with blunt trauma frequently have multiple, systemic injuries. Stabilizing patients before surgical repair of diaphragmatic hernia is essential. Diaphragmatic hernia is often not a surgical emergency and repair can wait until other problems are addressed. Surgery should not be delayed in animals that are severely dyspneic or that may have strangulated bowel within the diaphragmatic defect. Patients with intrathoracic gastric displacement may have acute, severe reduction in thoracic volume because of gastric dilatation, and this may be accompanied by avascular necrosis of the stomach wall. Therefore, surgery should not be delayed in these patients.
Diagnosis of diaphragmatic hernias is most easily accomplished with thoracic radiographs. The presence of bowel loops (A) or other abdominal organs within the thorax is diagnostic for diaphragmatic hernia. Sensitivity of radiographic detection of diaphragmatic hernias can be increased by performing a positive-contrast gastrointestinal study using barium. Alternatively, a positive-contrast peritoneogram can be done by injecting sterile, water-soluble contrast material into the abdominal cavity (about 2.2 ml/kg diluted with an equal volume of sterile saline).
Procedure PearlOn radiography, the presence of bowel loops or other abdominal organs within the thorax is diagnostic for diaphragmatic hernia.
A positive test occurs when contrast material can be observed within the thoracic cavity. The contrast agent is apparent in the pericardial sac (B; arrow) of this congenital peritoneopericardial diaphragmatic hernia. Holding the animal with the hindlegs elevated may facilitate movement of contrast matter through the hernia. The diaphragmatic rent may be sealed by omentum; thus, a negative result of this study does not rule out diaphragmatic hernia. Ultrasonography may also be useful to detect abdominal viscera within the thorax.
Anesthetic induction is a critical time for patients with diaphragmatic hernias. Hypoventilation is a major concern. If significant pleural effusion is present, perform thoracocentesis before induction of anesthesia. Administer oxygen for 5 minutes before induction. After induction, the patient may require assisted ventilation. Closely monitor ventilation with capnography or pulse oxymetry. Blood gas analysis, if available, can aid in ventilatory management.
Procedure PearlAnesthetic induction is a critical period. Preoxygenation, rapid induction, intubation, and ventilation are indicated. Vigilant patient monitoring at induction and throughout the surgery with capnography or pulse oximetry is vital.
Perioperative, prophylactic antibiotics are indicated, especially if nonabsorbable mesh may be implanted (see Step 12). Cefazolin (22 mg/kg, IV) is generally appropriate and administered 30 minutes before and every 2 hours during surgery.
Procedure PearlBlind digital dissection is often effective in breaking down adhesions, but this needs to be done gently.
Procedure PearlAntibiotics should be continued postoperatively only if there is an indication (e.g., break in aseptic technique, spillage of bowel contents, compromised liver parenchyma).
Prepare the patient for a routine abdominal ventral midline incision from xiphoid to pubis. The prepared area should include the caudal thorax in case a caudal median sternotomy must be done to break down intrathoracic adhesions that can form in the presence of chronic hernias. Preparation of the caudal thorax also allows aseptic placement of a thoracostomy tube.
Make a routine ventral midline abdominal incision beginning near the xiphoid process. Explore the abdominal cavity. Have an assistant, using a self-retaining Balfour retractor, retract the sternum ventrally and cranially; this substantially improves exposure of the diaphragm. Hernias in the diaphragm may be radial (A), circumferential (B), or a combination of the two.
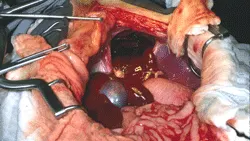
Once the hernia is identified, attempt to reduce the viscera by using gentle traction. In the figure, gentle traction is being used on the intestine in an attempt to reduce the hernia. Because the herniated bowel can have secondary pathologic conditions making it prone to rupture, be sure to avoid iatrogenic damage to viscera from applying excessive force to return the organs to the abdomen. Although abdominal organs often readily return to the abdomen, adhesions of the abdominal organs to the pleura or contracture of the hernia opening may prevent easy reduction of organs.
If resistance is felt during reduction of organs, the hernia can be enlarged as shown in the photograph. The incision made to enlarge the hernia should also facilitate and simplify closure (i.e., enlarge the hernia ventrally and away from any transdiaphragmatic structures). Take care not to damage the caudal vena cava, esophagus, or aorta and structures on the thoracic side of the diaphragm when enlarging the hernia.
Gently break down remaining adhesions. Extending the abdominal midline incision through the xiphoid process or caudal sternum may be necessary. Blind digital dissection is often effective in breaking down adhesions, but this needs to be done gently. Sharp excision of adhesions may be necessary, and adequate exposure is essential if intrathoracic sharp dissection is performed.
After the hernia is reduced, inspect all herniated organs for viability. If the herniated bowel appears dark and necrotic, resection and anastomosis should be performed. Herniated liver lobes often appear congested. If liver lobes appear necrotic, perform a partial hepatectomy. Before closing the diaphragm, check the thorax for continued bleeding from torn adhesions.
Place a thoracostomy tube before closing the diaphragm to allow direct observation of placement of the chest tube. The chest tube can exit across the thoracic wall or be placed through a purse-string suture in the diaphragm and exit the body through the ventral midline abdominal incision. If the hernia is chronic or there is potential for long-term use, the tube should be placed across the thoracic wall. Chest tubes are generally placed through a subcutaneous tunnel approximately 3 intercostal spaces long to limit air ingress around the tube. A purse-string suture should be placed where the chest tube exits the skin. Alternatively, if long-term use is not anticipated and the animal is stable, a small chest tube or red rubber catheter can be placed through a small stab incision in the diaphragm, exiting the abdominal midline incision. A purse-string suture is placed in the diaphragm around the tube. These tubes are not designed for long-term use and are removed by simple traction after the animal has recovered and is stable. Regardless of the exit point, secure the tube to the skin with a finger trap suture. If there is any question about the amount of air remaining in the thoracic cavity postoperatively, take a chest radiograph.
Close the hernia (herniorrhaphy) by using nonabsorbable monofilament suture in a simple continuous pattern (A). Begin closure at the most dorsal aspect of the hernia. Take care to avoid damaging transdiaphragmatic structures. It may be necessary to bolster repair of circumferential tears by first placing circumcostal mattress sutures and then continuing with routine closure. To place circumcostal sutures, the needle is directed around one of the last ribs (B); care is taken to avoid the intercostal artery, vein, and nerve just caudal to the rib. A larger needle may be necessary to provide sufficient length.
Insufficient tissue to close the defect in the diaphragm is rare. However, if necessary, use nonabsorbable mesh to close the defect. Suture the mesh to the diaphragm around its periphery with nonabsorbable monofilament suture in an interrupted mattress pattern. When implanting nonabsorbable mesh, strict adherence to aseptic technique is necessary as chronic fistula formation secondary to infection can occur. Prophylactic perioperative antibiotics are also indicated.
Fluid and air are removed from the thorax via the thoracostomy tube. In chronic hernias, sudden reexpansion of the lungs may lead to pulmonary edema. As long as ventilation and oxygenation are adequate, the lungs can gradually reexpand over several days. Forced pulmonary reexpansion at the time of surgery is generally avoided. A small residual pneumothorax should not compromise adequate ventilation.
Close the abdomen routinely. If a median sternotomy was done, close it with orthopedic wire in a cruciate pattern around the caudal sternebrae.
Postprocedural MONITORINGMonitor the animal closely during recovery. Analgesia is important, and supplemental oxygen may be required. Analgesia can be provided with several different modalities. Nonsteroidal antiinflammatory drugs can be given as long as there are no contraindications (e.g., renal disease, gastrointestinal disease or surgery, coagulopathy). These drugs are inadequate if used alone in the acute postoperative period, but augment balanced analgesia if combined with opioids. Placement of a fentanyl patch (3 to 5 µg/kg) is an easy way to ensure continuous analgesic delivery for 3 to 4 days postoperatively. These patches take about 12 to 24 hours to become effective, so additional analgesics should be administered in the interim. Hydromorphone (0.1 to 0.2 mg/kg, IV/IM Q 4 to 6 H) or morphine (1 to 2 mg/kg IM Q 6 to 8 H) are frequently used. While these drugs may cause respiratory depression, it is usually not a clinical issue.
If hypoxemia is evident on blood gas analysis (PaO2 < 80 mm Hg breathing room air) or pulse oximetry (SaO2 < 90 mm Hg), oxygen supplementation is indicated. Oxygen can be supplemented most easily with a nasal cannula. Insert the cannula into the ventral nasal meatus to a level just cranial to the medial canthus and suture or staple it to the skin. Apply a small amount of lidocaine to the nasal mucosa before insertion for local analgesia. Alternatively, oxygen can be supplied with a face mask, oxygen cage, or tracheal catheter. If hypercarbia is present (PaCO2 > 60 mm Hg), ventilation may be inadequate and mechanical ventilation should be considered.
DIAPHRAGMATIC HERNIA • Chad W. Schmiedt and Dale E. Bjorling
Suggested ReadingChronic diaphragmatic hernia in 34 dogs and 16 cats. Moynihan AC, Berg J, Evans KL. JAAHA 40:51-63, 2004.Diaphragmatic, pericardial, and hiatal hernia. Hunt GB, Johnson KA. In Slater DA (ed): Textbook of Small Animal Surgery, 3rd ed-Philadelphia: Saunders, 2000, pp 471-486.Perioperative survival rates after surgery for diaphragmatic hernia in dogs and cats: 92 cases (1990-2002). Gibson TW, Bryson BA, Sears W. JAVMA 227:105-109, 2005.Radiographic diagnosis of diaphragmatic hernia: A review of 60 cases in dogs and cats. Hyun C. J Vet Sci 76:171-177, 2004.Surgery of the lower respiratory system: Pleural cavity and diaphragm. Fossum TW. In Fossum TW (ed): Small Animal Surgery, 2nd ed-Philadelphia: Mosby, 2002, pp 760-787.