Fleur, a 12-year-old spayed domestic shorthair cat, is presented for a one-week history of worsening pruritus. She was diagnosed with hyperthyroidism 6 weeks prior, and treatment with methimazole (2.5 mg/cat PO every 12 hours) was initiated at that time.
History
Fleur is an indoor-only cat. Her appetite is mildly decreased, but she eats regularly. She has no recent history of vomiting, diarrhea, coughing, sneezing, polyuria, or polydipsia. As a kitten, she was diagnosed with ocular keratitis secondary to feline herpesvirus type 1 infection.
Physical Examination
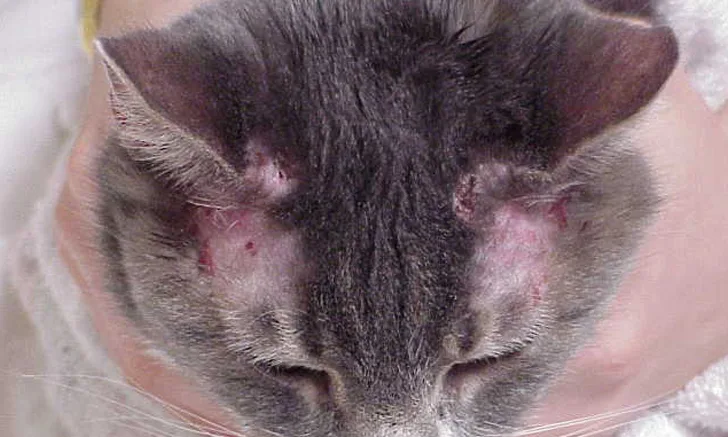
On physical examination, Fleur is bright, alert, and responsive. Temperature, pulse, and respiration are within normal limits. BCS is 4/9. There is a palpable thyroid slip, right-sided thyroid nodule, and grade II/VI parasternal heart murmur. She has bilateral hair loss and facial excoriations with no obvious signs of fleas or other ectoparasites (Figure).
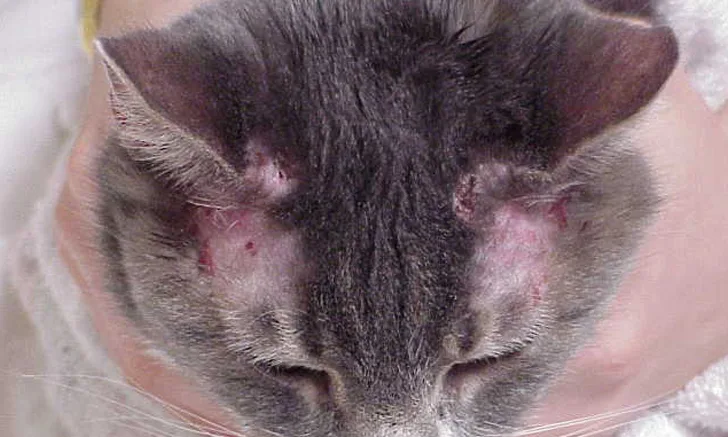
Facial excoriations
How would you diagnose and treat this patient?
Treatment & Outcome
Methimazole is a thyroid peroxidase inhibitor that inhibits thyroid hormone synthesis by interfering with iodine incorporation into tyrosyl residues of thyroglobulin. The primary differential diagnosis for pruritus and facial excoriations in this patient was an adverse effect of methimazole treatment. Other methimazole-related idiosyncratic reactions were assessed via CBC to rule out blood dyscrasias and serum chemistry profile to rule out hepatopathy and evaluate changes in renal function. Urinalysis can help assess renal function but was not performed prior to CBC because of concerns for methimazole-induced thrombocytopenia.
Methimazole administration adjustments (eg, switching to transdermal methimazole, reducing the amount of oral methimazole) can be considered in patients with GI upset secondary to methimazole; however, methimazole should be discontinued if facial excoriations, blood dyscrasias, or hepatopathy occur, as these adverse effects are not related to the dose.
Methimazole was discontinued, and pruritus and facial excoriations resolved. Successful control of hyperthyroidism was achieved via radioactive iodine treatment administered after one month.