
Yonkers, an 8-year-old, 108-lb (49-kg) intact male Bernese mountain dog, was presented for blood dripping from the prepuce. His owner reported the blood first appeared after an intact female dog in the household came into heat the previous week.
Physical Examination
On physical examination, Yonkers was bright, alert, and responsive. Vital parameters and thoracic auscultation were within normal limits. Serosanguineous discharge was present at the preputial opening. Palpation of the penis through the prepuce did not appear to elicit pain. The prepuce was retracted, and the penile and preputial epithelium appeared normal except for a light coating of serosanguineous discharge. A free-catch urine sample was collected. Although the urine stream was normal without interruption, the urine was grossly hematuric.
A digital rectal examination was performed, but the prostate could not be palpated within the pelvic canal, even with simultaneous application of caudodorsal pressure to the ventral abdomen. Other than the cranioventrally displaced prostate, there were no palpable abnormalities within the pelvic canal.
Diagnostics
Differential diagnoses for hemorrhagic preputial discharge include os penis fracture, urethritis, cystitis, benign prostatic hyperplasia, and prostatitis. Os penis fracture was unlikely because pain was not elicited with palpation and manipulation of the penis; radiography was not performed. Urinalysis results (bacteriuria, pyuria, hematuria; Table 1) were consistent with cystitis; however, primary cystitis could not be definitively diagnosed without concurrent evaluation of prostatic fluid because prostatic secretions normally empty into the bladder during sexual rest.
Table 1: Urinalysis Resultsa
a Abnormal values are in bold.
Semen was obtained via manual stimulation, and the ejaculate was collected in 3 fractions. The third fraction should be solely composed of prostatic fluid; the first and second fractions have prostatic fluid mixed with other components.1 Although all 3 fractions were hemorrhagic, only the third fraction was analyzed microscopically. Erythrocytes, epithelial cells, neutrophils (some with engulfed rod-shaped bacteria), and free rod-shaped bacteria were found. In addition, bacterial culture and susceptibility testing revealed Escherichia coli susceptible to most antibiotics tested (Table 2).
Table 2: Bacterial Culture Antibiotic Susceptibility Results
CBC and serum chemistry profile results were within normal limits, except for mildly elevated ALP (220 U/L; reference interval, 2-150 U/L). Transabdominal ultrasound showed an enlarged, heteroechoic prostate with multiple anechoic and hyperechoic foci, indicating a diagnosis of prostatitis (Figure).
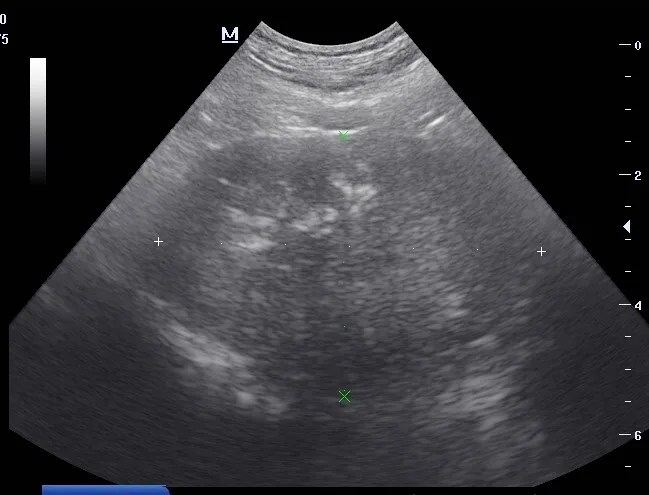
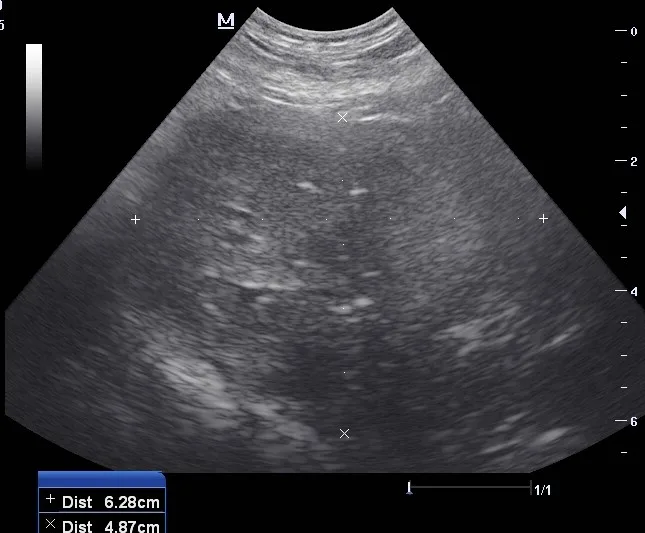
Ultrasound images of the left (A) and right (B) prostate lobes. The prostate was enlarged and heteroechoic with multiple anechoic and hyperechoic foci.
DIAGNOSIS: CHRONIC PROSTATITIS
Treatment & Long-Term Management
Treatment for chronic prostatitis should include administration of antimicrobials (to treat infection) and reduction of prostatic hyperplasia (to eliminate the predisposing condition). Antimicrobial selection should be based on culture and susceptibility testing and penetration into prostate tissues (see Antimicrobial Considerations).2 When results are unavailable or pending, empirical treatment should include coverage for E coli, as E coli is the leading cause of bacterial prostatitis.
Surgical castration of older male dogs may be curative for prostatic hyperplasia and is often recommended. Extra-label use of a long-term gonadotropin-releasing hormone agonist (deslorelin, 4.7 mg SC implant) can reduce prostate size by >50% within 6 weeks but induces reversible infertility.3 Finasteride (0.1-0.5 mg/kg PO every 24 hours; not to exceed 5 mg/DOG every 24 hours) is an inexpensive method for inducing prostate involution and can preserve fertility.4 The owner preferred Yonkers to remain intact and fertile.
Enrofloxacin (13.88 mg/kg PO every 24 hours) was administered for 6 weeks along with finasteride (5 mg total PO every 24 hours5). Enrofloxacin is a zwitterion, which is neither purely acidic nor basic because it consists of one positively charged and one negatively charged ion group,6 and therefore penetrates and accumulates within the prostatic parenchyma. Antimicrobial treatment should continue until the prostate has undergone ≈50% involution, which typically takes an average of 6 weeks from the initiation of finasteride treatment. In patients in which maintaining fertility is not a concern, finasteride treatment should be continued until surgical castration can be performed.
Treatment at a Glance
An antibiotic (eg, enrofloxacin) that can penetrate the prostatic parenchyma should be selected.
Therapy should include medical or surgical prostatic involution.
Prognosis & Outcome
Preputial discharge stopped completely within 2 weeks of initiation of treatment. Follow-up transabdominal ultrasound examination of the prostate revealed ≈50% involution at 6 weeks and ≈90% at 6 months. Yonkers has received finasteride for 2 years and remains clinically normal. Lifelong treatment with finasteride will be needed unless castration is performed.
Discussion
Acute Versus Chronic Prostatitis
Prostatitis in dogs can be acute or chronic. Acute prostatitis is rare and can occur regardless of age or neuter status, but young, intact males are overrepresented. Clinical signs include anorexia, fever, depression, vomiting, and gait abnormalities. Abdominal and/or transrectal palpation may not be possible due to moderate to severe pain associated with the inflamed prostate. CBC results include neutrophilia with a left shift, and urinalysis results typically include pyuria and evidence of bacteria.2 Acute prostatitis most likely has a hematogenous origin or develops secondary to bacterial cystitis. Ultrasound findings include a normal prostate size and hypoechoic parenchyma (compared with the normal homogeneous echodense appearance).7
Chronic prostatitis is common in older, intact dogs with benign prostatic hyperplasia, which is a predisposing condition. Many dogs with chronic prostatitis appear clinically normal.8 Clinical signs are variable and depend on degree of prostatomegaly but most commonly include urethral discharge, hematuria, and tenesmus, which is only present when the prostate is morbidly enlarged.6 Unlike acute prostatitis, systemic signs (eg, fever, depression) and evidence of pain are not present. Preputial discharge can be clear, purulent, or hemorrhagic.9 In a retrospective study, hemorrhagic preputial discharge that could be exacerbated by sexual arousal was the only clinical sign observed in 23% of cases.10 Urinary signs (eg, hematuria, pollakiuria, stranguria, dysuria, pyuria, polyuria) are exhibited by >50% of dogs with chronic prostatitis.8 Laboratory findings are generally within normal limits or inconclusive for prostatic disease. Ultrasonographic appearance of the prostate is coarsely hyperechoic throughout the parenchyma, with regions of heteroechoic echotexture and dystrophic mineralization resulting from fibrosis and chronic inflammation.7
Antimicrobial Considerations
Most antimicrobials effective against uropathogenic bacteria diffuse poorly into prostatic tissue because the blood–prostate barrier prevents diffusion of drugs highly protein bound in plasma from entering prostatic fluid in therapeutic concentrations.4 The ability of an antimicrobial to cross an epithelial membrane depends on its lipid solubility and pKa (ie, pH at which a drug exists equally in ionized and nonionized forms). Only nonionized forms can cross epithelial membranes, and the blood–prostate barrier can only be crossed by lipophilic drugs not highly bound to proteins.6 Drugs with low lipid solubility (eg, ampicillin, penicillin, cephalothin) weakly cross epithelial membranes. Drugs with a basic pH (eg, sulfamethoxazole/trimethoprim, erythromycin) diffuse easily from blood (pH, 7.4) to the more acidic prostatic environment (pH, 6.1-6.5) and become concentrated on the side with the greatest ionization/charge (eg, acidic canine prostatic fluid).2,11
When surveyed, 30% of clinicians indicated they would prescribe amoxicillin/clavulanate, a drug with poor penetration into prostate tissues.12 Chloramphenicol and enrofloxacin (fluorinated quinolone) are lipophilic and not highly protein bound. Both can readily cross epithelial membranes regardless of their pH because of their zwitterion characteristics2; however, chloramphenicol is not effective against gram-negative bacteria (eg, E coli).
Take-Home Messages
Prostatic disease cases can be challenging. A prostatic fluid sample should be evaluated in intact male dogs presented with hematuria.
Chronic prostatitis can be effectively managed with medication in intact male dogs intended for breeding.
Enrofloxacin is the ideal antimicrobial for treating chronic prostatitis because it readily penetrates prostate tissues and is bactericidal against most gram-negative and gram-positive bacteria.
Listen to the Podcast
Dr. Kutzler digs deeper into the diagnosis and treatment of chronic prostatitis in this episode of the podcast.