Pleural effusion (ie, abnormal accumulation of fluid in the thoracic cavity, outside the lungs and pericardial space) is a common, emergent disease process in dogs and cats. In healthy patients, a small volume of fluid (dogs, 0.3 mL/kg; cats, 0.1 mL/kg) in the pleural space lubricates the visceral and parietal pleura and prevents lung collapse.1 A variety of disease processes (eg, neoplasia, cardiac disease, idiopathic chylothorax, pyothorax, trauma, diaphragmatic hernia, hypoproteinemia, vasculitis, pneumonia, fungal disease, anticoagulant rodenticide toxicosis) can cause abnormal accumulation of fluid in the pleural space.1-12 In addition, lung lobe torsion has been reported as an underlying condition in dogs, and FIP and asthma have been reported in cats.1-12 Pleural effusions can be distinguished based on cellularity, protein content, cytologic appearance, and additional biochemical features (eg, triglyceride levels) and may be characterized as pure or modified transudates, exudates, chylous effusions, hemorrhagic effusions, and/or neoplastic effusions.
Presentation & Physical Examination
Patients with pleural effusion are commonly presented for respiratory signs (ranging from mild tachypnea to severe respiratory distress) but may also be presented for lethargy, exercise intolerance, hyporexia/anorexia, or other systemic signs of illness. Physical examination findings may include a short, shallow, or restrictive breathing pattern, as well as muffled lung and heart sounds, pallor or cyanosis, abdominal effort, an outstretched head or neck, and/or orthopnea.
Diagnostics
The diagnostic test of choice for identification of pleural effusion is point-of-care ultrasound (POCUS) using thoracic focused assessment techniques that minimize patient restraint and stress.3,4,6,11,13-15 Thoracic radiography can be used if focused ultrasound is unavailable; however, care should be taken to minimize stress in patients with respiratory distress by administering a mild, short-acting sedative (eg, butorphanol, 0.2-0.4 mg/kg IV, SC, or IM16), using fear-free restraint techniques, and/or obtaining a single-view radiograph (lateral or dorsoventral) to allow quick diagnosis. Three-view thoracic radiographs should be obtained following thoracocentesis and patient stabilization.
Stabilization
Initial, rapid stabilization is crucial. Oxygen therapy via flow-by tubing or oxygen cage should be provided immediately to patients with respiratory distress. Stabilization of hemodynamically unstable patients may require fluid resuscitation with or without a vasopressor (eg, norepinephrine, dopamine, dobutamine). Thoracocentesis provides therapeutic (eg, stabilization of patients with respiratory distress) and diagnostic (eg, fluid analysis, cytology with possible culture) benefits and should be performed early (see Step-by-Step).
Referral
Timely referral to a specialty or tertiary care facility is generally recommended for advanced diagnostics and therapeutics with or without inpatient care. Prior to transport, patients with diagnosed or suspected pyothorax may be given targeted therapy with broad spectrum antibiotics (ampicillin/sulbactam, 22-30 mg/kg IV every 8 hours, and enrofloxacin, 5 mg/kg IV every 24 hours in cats, 10 mg/kg IV every 24 hours in dogs),17,18 and patients with diagnosed or suspected congestive heart failure may be given furosemide (2 mg/kg IV).19 Medical transport (transport with veterinary technical staff or via pet ambulance service) with oxygen support may be necessary if thoracocentesis does not stabilize respiratory distress.
Prior to transport, the intended referral center should be contacted to confirm the facility is accepting case transfers, ensure preparation for the patient’s arrival, and discuss prognosis and estimated cost of inpatient care and diagnostics. Prognosis and cost details should be communicated to the pet owner. The owner should understand that pleural effusion is often secondary to significant underlying disease, which may be chronic or recurrent and require long-term treatment; prognosis for long-term survival is guarded.
Step-by-Step: Thoracocentesis in Patients With Pleural Effusion
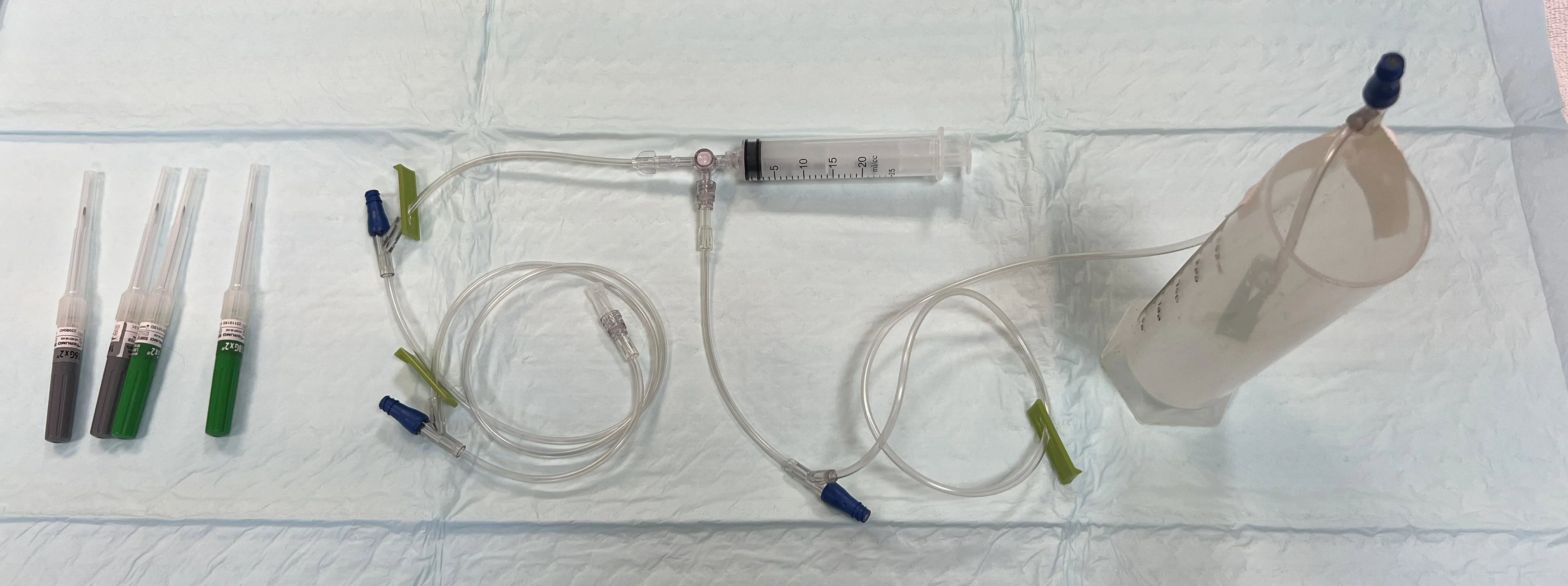
What You Will Need
Clippers
Sterile surgical scrub
Gloves
Hypodermic needle (cats, 22 gauge, 1 inch; dogs, 18-22 gauge, 1-1.5 inch based on patient size), over-the-needle catheter (cats, 22 gauge; dogs, 18-22 gauge), or butterfly catheter (cats or small dogs, 23 gauge)
2 extension sets
3-way stopcock
Collection container
Syringes (6-60 mL based on amount and viscosity of fluid expected, size of needle/catheter, and operator preference)
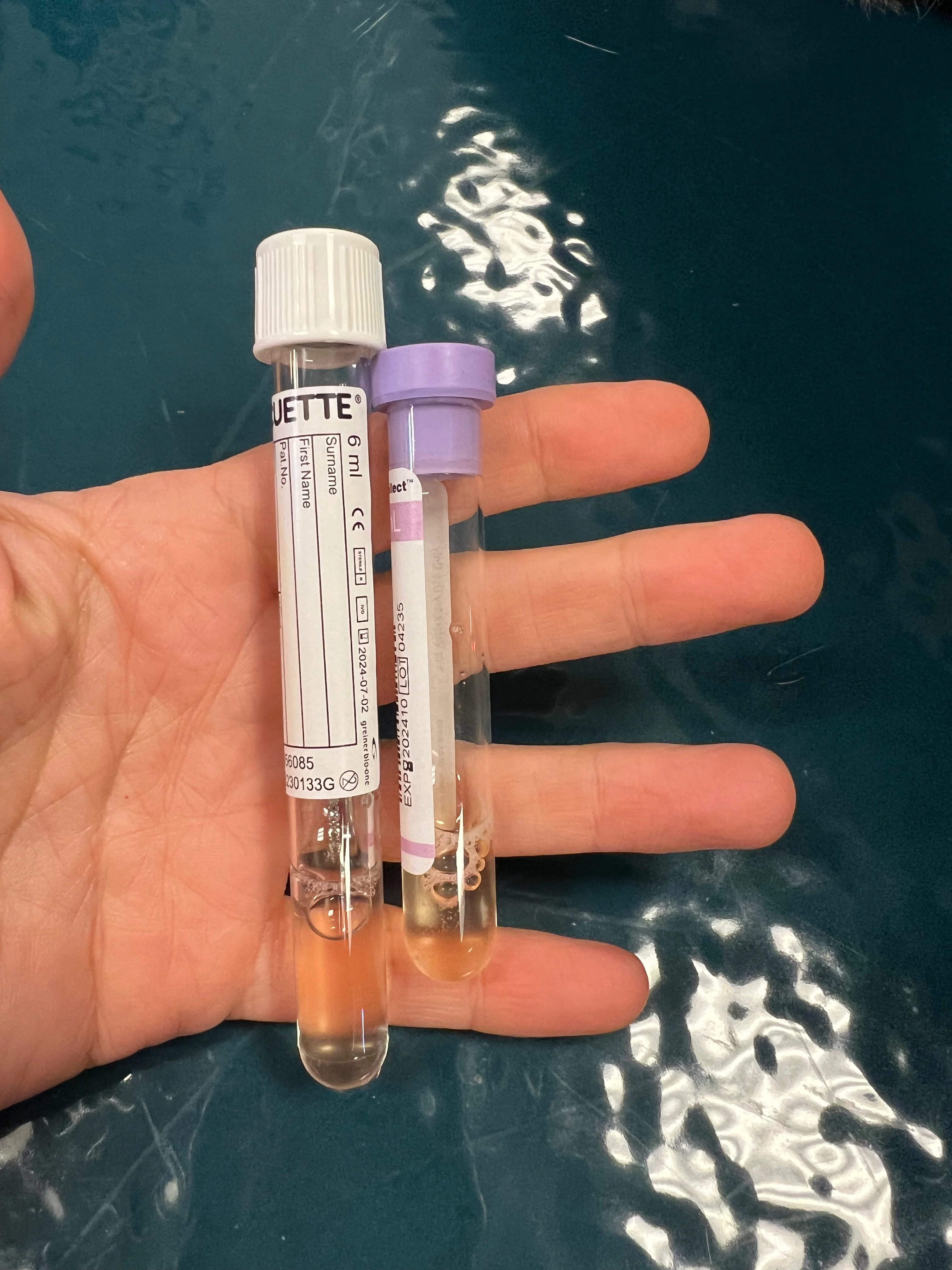
Lavender-top and nonadditive tubes
ECG (if available)
Ultrasound (if available)
Sedation (optional)
Oxygen (optional)
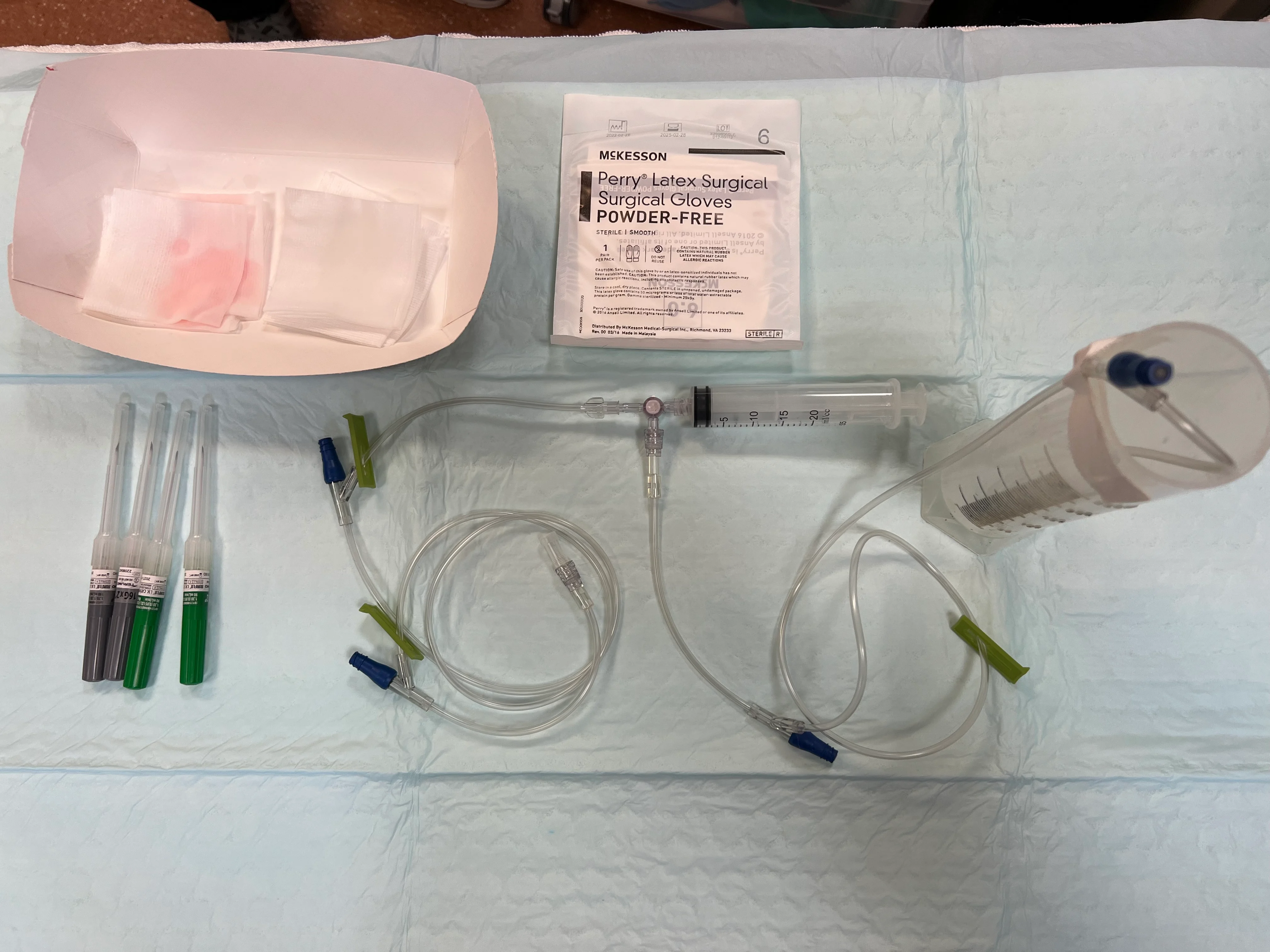
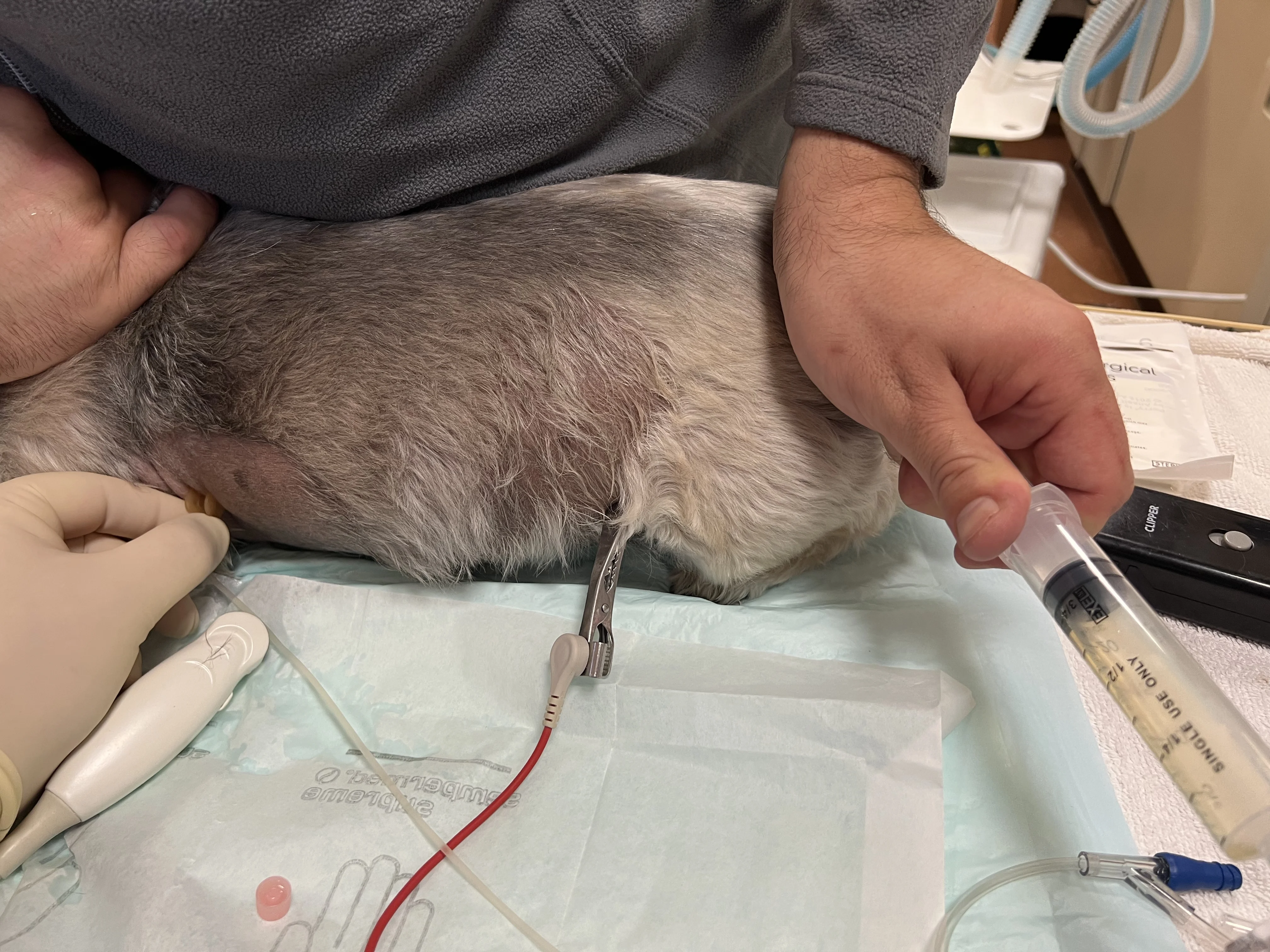
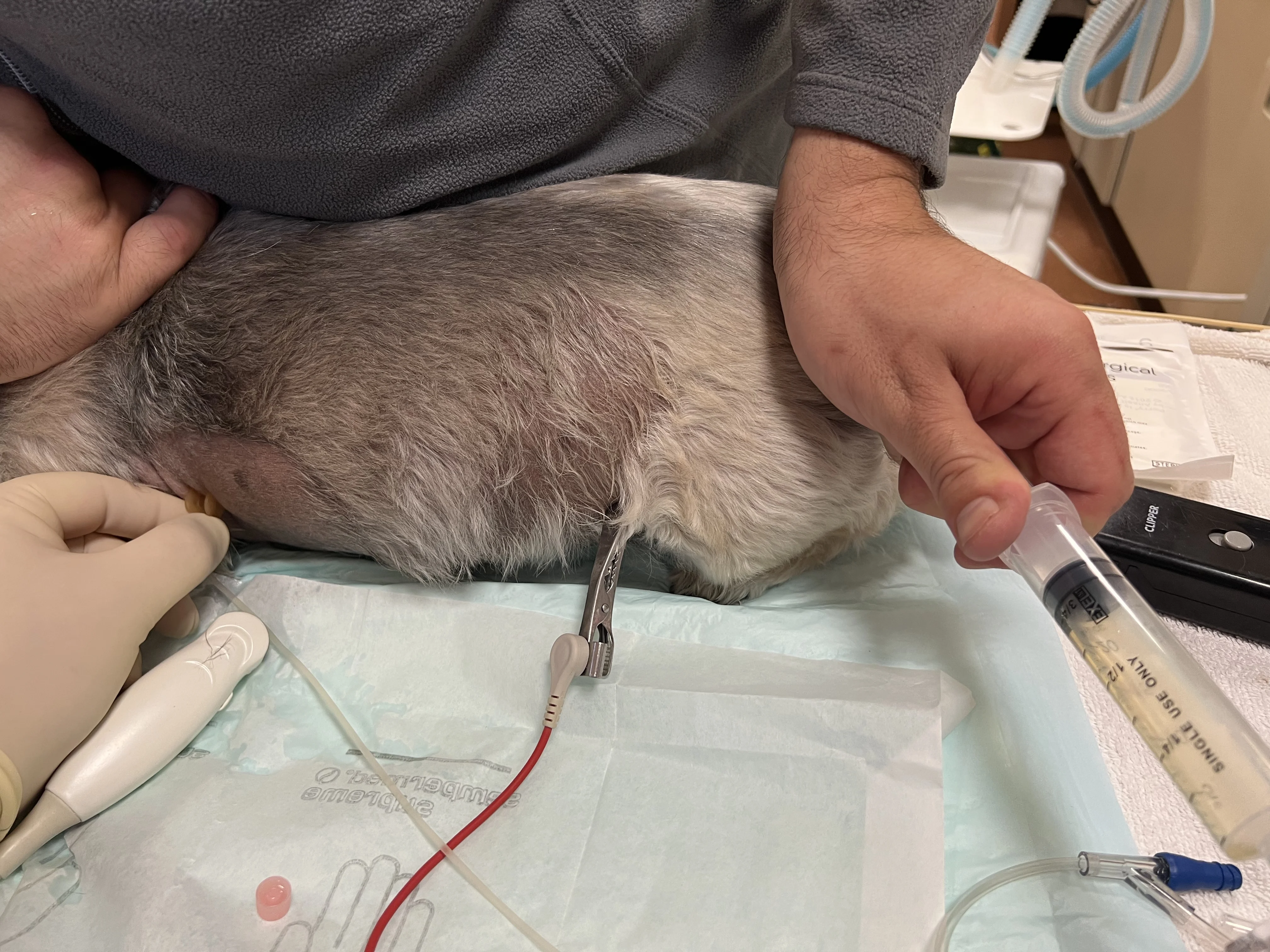
Step 1: Prepare Collection Equipment
Using sterile technique, connect the 3-way stopcock to a syringe and 2 extension sets, with one set connected to the needle and the other taped inside the collection container. Ensure the stopcock is turned off to the patient.
Step 2: Prepare & Position the Patient
Provide sedation and/or oxygen therapy as indicated. Connect ECG leads (if available). Place the patient in the most comfortable and least stressful position (sternal recumbency is most effective in the author’s experience, but the patient can also stand, sit, or be in lateral recumbency).

Author Insight
Three staff members are typically needed to perform thoracocentesis: one to restrain the patient, one to place and stabilize the needle, and one to operate the syringe for fluid collection. Sedation can ease patient stress and discomfort and provide appropriate restraint. In the author’s experience, butorphanol (0.2 mg/kg IV, SC, or IM) with or without midazolam (0.2 mg/kg IV, SC, or IM) can provide adequate, safe sedation in patients in respiratory distress.16,20
Oxygen therapy can be provided via flow-by tubing or an oxygen mask (if tolerated).
Step 3: Prepare the Skin
Clip the fur and aseptically scrub the skin around the needle insertion site(s) while wearing nonsterile gloves.

Step 4: Determine Needle Location
Use POCUS (if available) to direct the anatomic location of the tap.

If POCUS is not available, palpate the ventral third of the thorax to identify the seventh to ninth intercostal spaces.

Author Insight
On ultrasound, pleural effusion appears as an anechoic pocket separating the lung lobes from the thoracic wall.

Step 5: Insert the Needle
Wearing sterile gloves, insert the needle at the cranial aspect of a rib (to avoid the intercostal vessels) with the bevel facing up and at a 45-degree angle to the body wall. Slowly advance the needle until it passes through the body wall. Back the needle out slightly if a gentle scraping sensation is felt on the needle tip, as the needle may be rubbing the lung. If using an over-the-needle catheter, remove the stylet and reattach the catheter to the extension set.
Author Insight
A slight pop may be felt when the needle passes through the body wall.
Step 6: Remove Fluid
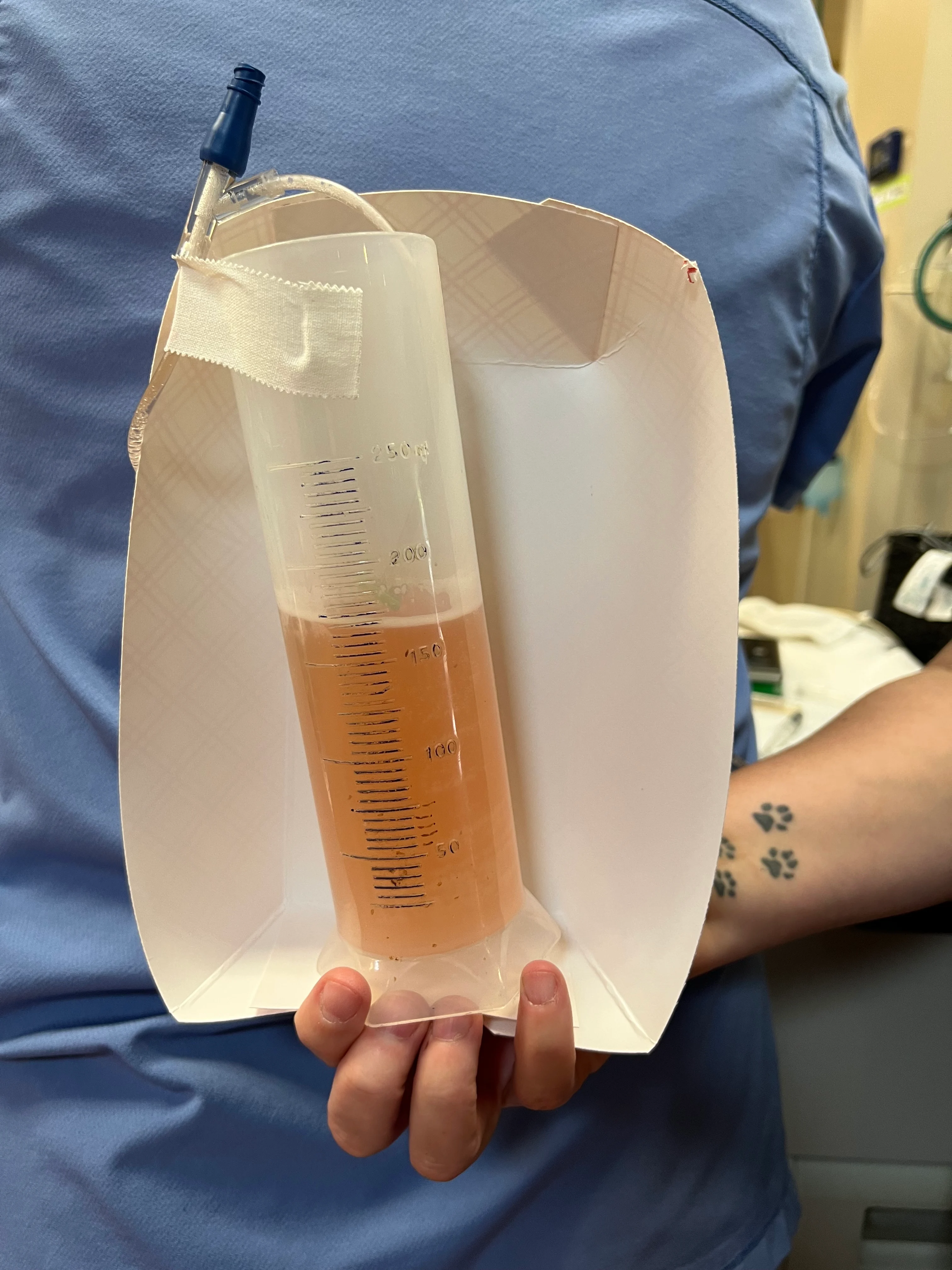
Turn the stopcock so it is open to the patient. Apply gentle negative pressure to the syringe, and allow fluid to fill the syringe. Once the syringe is full, turn the stopcock off to the patient and open to the collection container for evacuation. Repeat this process until negative pressure is obtained and the pleural effusion is removed. Save samples in lavender-top and nonadditive tubes for analysis. If pyothorax is suspected, also save a fluid sample for culture and susceptibility testing.
Author Insight
Unilateral or bilateral drainage may be required. The volume removed from each hemithorax should be quantified and described.
In cases of hemothorax, small-volume thoracocentesis may be needed. If blood is obtained, a small amount should be placed in a container and observed for clotting. If clots are noted, the procedure should be stopped, the location of fluid reconfirmed via POCUS (if available), and/or the needle repositioned (eg, retapping one intercostal space cranial or caudal to the original site, inserting the needle slightly shallower). Blood can be collected in sterile 60-mL syringes and used for autotransfusion, if appropriate (eg, in patients with trauma or coagulopathy); this should be avoided in patients with septic, contaminated, or neoplastic effusions.
Step 7: Post-Tap Assessment
Use POCUS (if available) to assess any remaining fluid. Consider thoracic radiography to assess the remaining fluid volume and allow full evaluation of the thorax for underlying lesions. Recommend POCUS or thoracic radiography to assess for post-tap pneumothorax if breathing does not improve or worsens.

Author Insight
A second thoracocentesis in a different location or on the contralateral side may be necessary if a significant volume of fluid remains.