Peritoneopericardial Diaphragmatic Hernia in a Cat
Ameet Singh, DVM, DVSc, DACVS (Small Animal), University of Guelph
Keaton Morgan, BVSc, University of Guelph

Joker, a 5-year-old, neutered male indoor Maine coon cat, was referred and presented to the surgical service for acute onset lethargy, hyporexia, and tachypnea. The owners reported that, in the 24 hours prior to presentation, Joker had developed a rapid respiratory rate with significant abdominal effort.
Joker had historically been an active cat but had become listless and begun to hide and avoid mealtimes in the last 24 hours. His owners had adopted him 2 years previously and noted that he frequently exhibited intermittent labored breathing that was not associated with any particular activity or event. Joker was considered an otherwise healthy cat with a historically good appetite and occasional vomiting episodes attributed to hairballs. However, on further questioning, the owners also reported that Joker frequently displayed apparent exercise intolerance when playing with the other 2 cats in the household. No coughing, sneezing, or diarrhea was reported.
Physical Examination
On presentation, Joker was quiet but alert and responsive. He was tachypneic (respiratory rate, 60 breaths/min) but had normal lung sounds across all lung fields and no nasal discharge. Cardiac auscultation revealed a muffled heart beat that was otherwise normal in rate and rhythm. Body temperature was normal (101.8°F [38.8°C]). Normal abdominal organs could not be appreciated during palpation. Flow-by oxygen supplementation was provided until diagnostics could be performed.
Diagnosis
Initial CBC and serum chemistry results were unremarkable. A mild stress leukogram characterized by mature neutrophilia (9.35 × 103/μL; reference range, 2.1-8.3 × 103/μL) was the only notable finding.
Two-view thoracic radiographs (Figure 1) were obtained with Joker under mild sedation (butorphanol [0.2 mg/kg IV]). Marked widening of the cardiac silhouette, both in height and width, with loss of delineation of the caudal cardiac margin, was observed. Superimposition of air tubular opacities to the cardiac silhouette were also noted. The liver was not visible at its physiologic position in the cranial abdomen. Considering these radiographic findings, a presumptive diagnosis of peritoneopericardial diaphragmatic hernia (PPDH) was made.
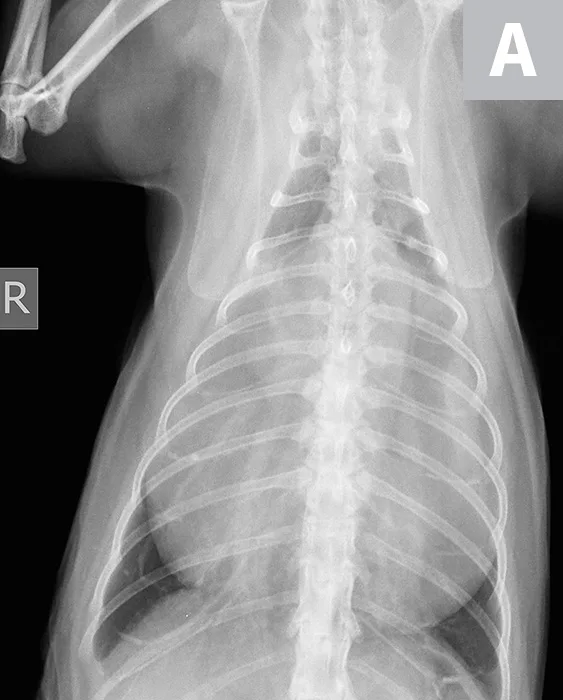
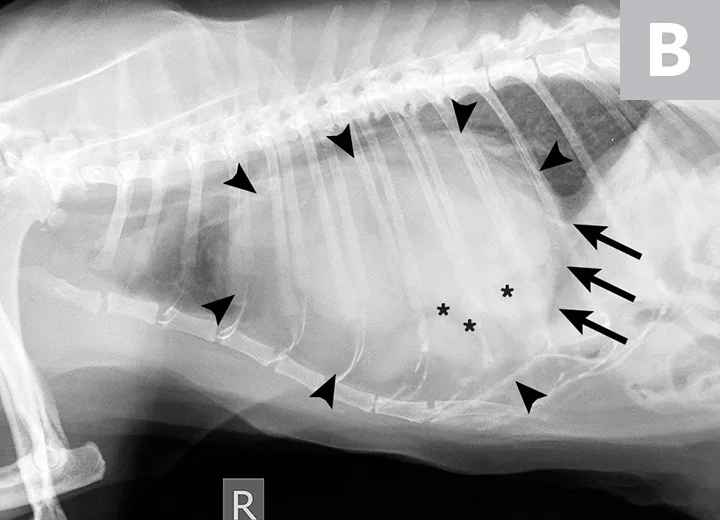
Ventrodorsal (A) and lateral (B) thoracic radiographs demonstrating an enlarged cardiac silhouette (arrowheads) with gas-filled tubular opacities consistent with the GI tract (asterisks) and loss of the caudal cardiac margin (arrows)
Diagnosis: Peritoneopericardial Diaphragmatic Hernia
Treatment & Long-Term Outcome
Joker was kept in a calm environment and continued to receive oxygen supplementation overnight. The following day, he was placed under general anesthesia. He was premedicated with hydromorphone (0.05 mg/kg IV) and acepromazine (0.02 mg/kg IV), induced with propofol (IV) to effect, and maintained with an isoflurane inhalant carried in oxygen. An exploratory laparotomy was performed, and a diagnosis of PPDH was confirmed (Figure 2; see Treatment at a Glance).
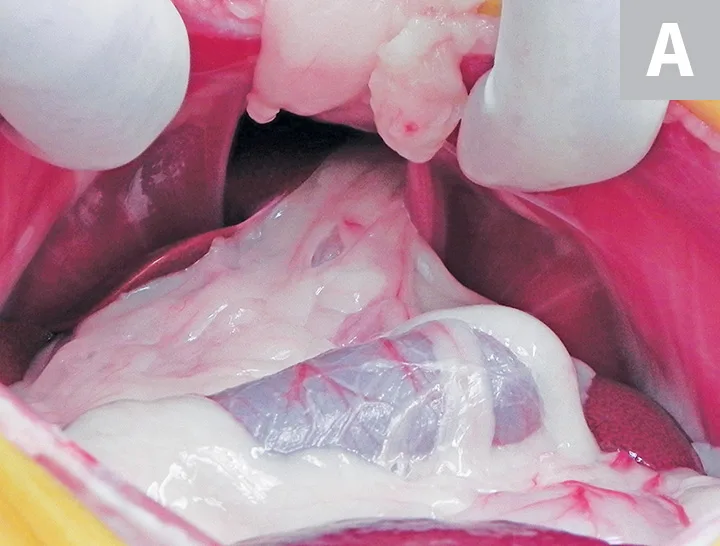
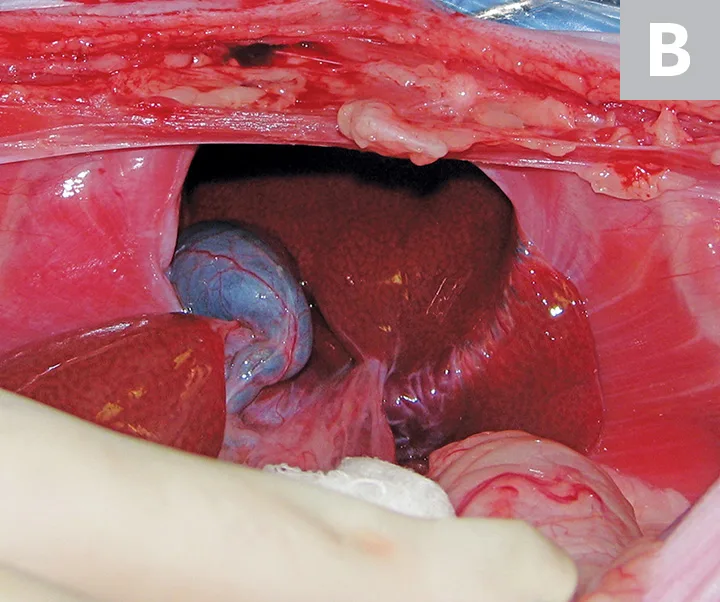
Intraoperative images. The PPDH can be visualized after ventral midline laparotomy and removal of the falciform ligament (A). The PPDH contains the hepatobiliary tract and a portion of the small intestine and omentum. Following reduction of the GI contents and the herniated portion of the omentum, the hernia ring can be visualized, and the hepatobiliary tract remains in the PPDH (B).
The liver, gallbladder, and a portion of the small intestine and omentum were extracted from the pericardial cavity. No adhesions were found between the herniated structures and the pericardium or myocardium. The defect in the ventral diaphragm was identified and closed using a simple continuous suture pattern. The edges of the defect were not debrided. A red rubber catheter was inserted into the pericardial space during herniorrhaphy.
Following completion of the herniorrhaphy, air was removed from the pericardial sac. Primary herniorrhaphy, which closes the pericardium and peritoneal cavity simultaneously without resulting in pneumothorax from entry of air into the thoracic cavity, is feasible in most cases of PPDH. Intraoperative hypotension was noted and was responsive to vasopressor therapy. No additional intraoperative complications were noted.
Thoracic radiographs were obtained immediately postoperation with the patient still under general anesthesia and confirmed reduction of PPDH. Joker recovered well from surgery and was discharged 48 hours postoperation and after resolution of tachypnea.
Treatment at a Glance
Surgical treatment can result in amelioration of clinical signs, although some owners will elect nonsurgical management in cats without clinical signs or that are geriatric.1 Although conservative management is a viable option, continued clinical signs or even death associated with cardiac tamponade is possible.1,3,4 In addition, the complication rate from surgery is low, so surgery is often performed in many PPDH cases, regardless of whether clinical signs are present.
Surgery involves an exploratory laparotomy to remove the herniated viscera from the pericardium and closure of the congenital defect in the diaphragm with sutures. Adhesions can be present between the viscera and pericardium or myocardium and, if encountered, should be carefully dissected to avoid hemorrhage.3
The most common perioperative complications include hypotension, hyperthermia, hypoventilation, hypoxia, and ventricular arrhythmias (eg, ventricular premature complexes) necessitating the need for careful anesthetic monitoring.1,2
A perioperative mortality rate of 3.2% to 14% has been reported in cats; however, prognosis is generally excellent if the cat survives the perioperative period.1-3
Prognosis & Outcome
At the 6-month follow-up, Joker was free of clinical signs. The owner reported resolution of Joker’s previous exercise intolerance observed with the other cats in the household. There had been no incidence of respiratory distress or development of any GI signs.
Discussion
PPDH is a congenital defect that occurs during embryonic development.1,2 In cats, PPDH is not traumatic in origin as in humans, as there is no anatomic connection between the pericardium and diaphragm.1,2 Surgical treatment of PPDH has an excellent long-term prognosis that generally results in resolution of clinical signs (see Take-Home Messages), as observed with Joker.1-3
Take-Home Messages
The most common congenital cardiac condition diagnosed in cats older than 2 years is PPDH, which allows abdominal viscera to move into the thorax and the pericardial sac.5
An overrepresentation of PPDH in longhair cat breeds has been reported.1-3
Most clinical presentations relate to the respiratory or GI tract, but an incidental diagnosis is also common.1-4
Common physical examination findings include muffled heart sounds, cardiac murmur, pyrexia, tachypnea, empty abdominal palpation, and/or a thin body condition, although no significant findings may be noted on physical examination, as incidental findings are also common.1-3
The best tool for diagnosis of PPDH is thoracic radiography, which can be supplemented with thoracic ultrasonography or CT if available.1,2
Common concurrent diseases include sternal or vertebral anomalies, hypertrophic cardiomyopathy, and chylothorax.1-3
Cases in which all abdominal viscera have herniated into the pericardium have been reported; however, it is more common for only the cranial abdominal viscera (eg, liver, gallbladder, small intestine, omentum, stomach) to be herniated.1-3