Pelvic Fractures
Kamran Babamohammadi, DVM, Animal Surgical Center, East Meadow, New York
Matthew D. Johnson, DVM, MVSc, DACVS (Small Animal), ACVS Fellow of Minimally Invasive Surgery (Small Animal Orthopedics), University of Florida

Background & Pathophysiology
Pelvic fractures comprise 20% to 32% of all fractures in dogs and cats,1-5 with vehicular trauma being the most common cause of pelvic fractures in small animals.3,5,6 Most pelvic fracture patients have polytrauma injuries, including fracture or luxation of the extremities (25%-56%), pulmonary trauma (10%-29%), hemoabdomen (15%-33%), cardiac arrhythmia (9%), spinal or neurologic trauma (6%-20%), and urinary tract injury (2%-39%).4,7-10 There is no breed predisposition associated with vehicular trauma, but dogs and young intact male outdoor cats are commonly affected.11,12
There are many different types of pelvic fracture configurations, and nearly half of pelvic injuries in dogs and cats involve fractures of the ilium.3,4,7,8 Clinically significant fractures involve the weight-bearing axis of the pelvis that includes the ilium and acetabulum (Figures 1-3). Although not a fracture, sacroiliac luxation is potentially significant because the sacroiliac joint is a component of the weight-bearing axis of the pelvis. Unilateral or bilateral fractures or luxations may occur, and it is common for patients to have a combination of pelvic injuries.3,4,7,13
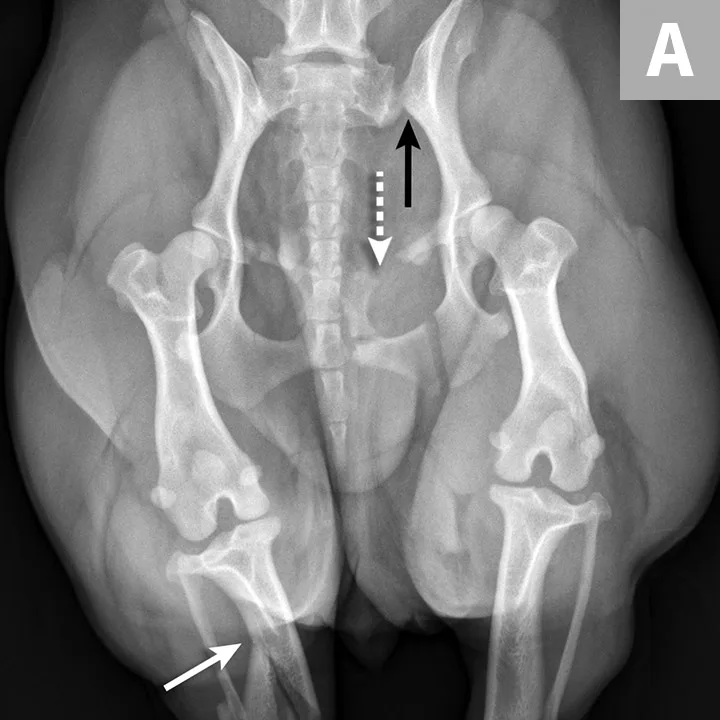
FIGURE 1A
An 11-year-old intact female Welsh corgi with injuries of the weight-bearing axis of the pelvis. Ventrodorsal (A) and lateral (B) projection images show a left sacroiliac luxation with cranial and ventral displacement (black arrow). Pubic fracture with lateral displacement (dashed arrow) and an oblique tibial fracture (white arrows) were additional comorbidities. The tibial fracture was treated surgically with an internal plate fixation, and the pelvic injuries were managed conservatively.
Clinical Signs
Pelvic fractures are generally secondary to a traumatic event. A thorough initial physical examination is essential to identify significant comorbidities. Careful orthopedic and neurologic examinations are also necessary to assess the full extent of injuries. Patients with pelvic fractures may be presented as weight-bearing or non-weight–bearing, depending on the extent of injuries. Additional injuries to the distal limbs can include fractures, lacerations, degloving injuries, and bruising. Patients with pelvic fractures can have peripheral nerve damage related to the close anatomic locations of nerves to the pelvis and sacrum. The lumbosacral trunk is most often affected; however, injury or entrapment of the sciatic nerve is most common.3
Comorbidities (eg, traumatic diaphragmatic, inguinal, or abdominal wall hernias; intra-abdominal injuries) should be investigated. In a study of 83 dogs with pelvic fractures, the occurrence of intra-abdominal injury was 35.2%, with hemoabdomen being the most common finding.8 Another study found pelvic fractures in 5 of 26 dogs with traumatic body wall hernia.14 In a study of traumatic diaphragmatic hernia, up to 13% of cats and 33% of dogs had orthopedic comorbidities that included pelvic fractures, which were often repaired in a second surgical procedure after diaphragmatic hernia correction.15
Lower urinary tract injuries are common in patients with a pelvic fracture,7 and urethral trauma or avulsion and urinary bladder rupture are possible. In a study, 39% of pelvic fracture patients had trauma to the urinary tract that included urinary bladder rupture, urethral tears, and/or urethral avulsion.9
Diagnosis
Pelvic fracture can be suspected based on patient history and clinical examination findings; however, definitive diagnosis requires orthogonal radiography. Lateral and ventrodorsal orthogonal radiography is the diagnostic of choice for identifying pelvic fractures.3,16,17 An oblique ventrolateral radiograph may be helpful in preventing superimposition of the femoral heads in fractures involving the acetabulum.<sup18 sup>
CT is recommended to increase the sensitivity of diagnosis and prognosis for injuries (eg, acetabular fractures, sacral fractures with neurologic deficits, complex pelvic fractures).17
Thoracic radiography is recommended to rule out traumatic pleural and pulmonary injuries and diaphragmatic hernia in all trauma patients.3,4,7 Abdominal radiography, ultrasonography (diagnostic or abdominal-focused sonography for trauma), cystography, or abdominocentesis are recommended in patients with suspected abdominal effusion or urinary tract injuries.4,7,8
Treatment & Management
Pelvic fractures in small animals can be treated with conservative or surgical management.
Conservative management is often successful in cats and small breed dogs and is used in ≈75% of cases.6 In a retrospective study of 43 patients with various pelvic fractures and no access to surgical treatment, 95% regained function.19 Patients that are good candidates for conservative management have pelvic fractures with minimal displacement, that are not part of the weight-bearing axis of the pelvic bones, or in which pelvic canal continuity remains. Pelvic fractures consistently heal because of the abundant muscle tissue surrounding the pelvis and extensive blood supply to the pelvic bones.1-3 Conservative management requires cage rest for 2 to 8 weeks, depending on injury severity, patient activity level, patient age (longer convalescence in older patients), and the presence of multiple injuries that may prolong recovery.20 Neurologic deficits may also prolong recovery and require modified activity and restrictions for up to 10 to 16 weeks.7 Regardless of fracture configuration, conservative management can be attempted if proper care (eg, padded, soft bedding; assistance with ambulation and elimination; food and water during recumbency) can be given in the home during the convalescent period and if pain can be managed with oral medications.3,7
Surgical management of pelvic fractures can be determined based on pet owner expectations and fracture configurations (Figures 4 and 5). Factors that influence surgical intervention include ≥45% narrowing of the pelvic canal; acetabular fractures involving the cranial two-thirds of the acetabulum; disruption of the weight-bearing axis (eg, ilial body, sacroiliac luxation); neurologic deficits or intractable pain due to trauma or nerve entrapment; ipsilateral fractures of the ilium, ischium, and pubis that cause instability of the acetabular segment; and other injuries that require early support of pelvic fractures.3,4,6,7,20-22
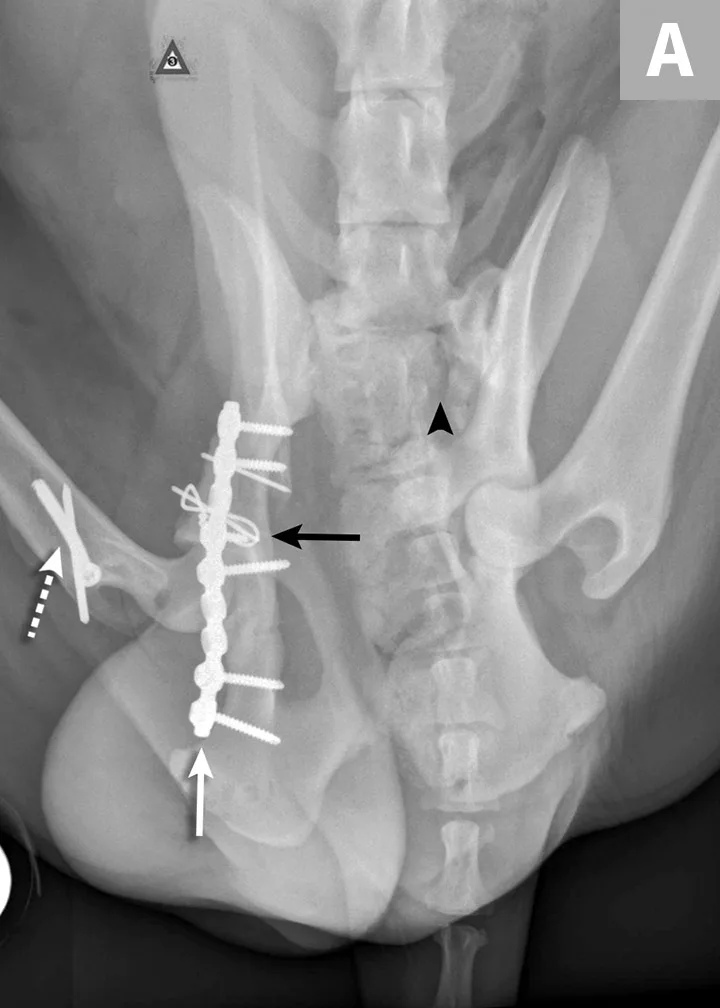
FIGURE 4A
Postoperative ventrodorsal (A) and lateral (B) projection images of the same dog in Figure 2. Fracture reduction was achieved with cross pins and a figure-eight hemicerclage wire (black arrows). Reduction was protected via application of a locking string-of-pearls neutralization plate (solid white arrows). To gain access to the full extent of the fracture, a greater trochanteric osteotomy was performed and stabilized with a positional screw and pin (dashed arrows). The ventrodorsal postoperative radiograph revealed a sacral fracture not previously appreciated (arrowhead). The fracture was successfully treated with conservative management.
Sacroiliac luxation and sacral fracture are the most common causes of multiple neurologic deficits in pelvic injuries3 and are caused by the location of the lumbosacral plexus ventral to the sacrum. Surgery for sacroiliac luxation depends on several factors, including degree of displacement, bilateral injury, and level of discomfort.21-23 Lag screw placement traversing >60% of the width of the sacrum is the most common surgical technique used for sacroiliac luxation.24,25
Ilial fracture stabilization can be accomplished using several methods individually or in combination; lateral or ventral plate stabilization with locking or nonlocking plates are the most common methods. Sciatic nerve injury can be associated with ilial fracture because of the location of the nerve medial to the ilial body. Care should be taken during fracture reduction and stabilization to avoid iatrogenic trauma to the nerve.26
Most acetabular fractures have traditionally been treated surgically; however, it has been suggested that fractures in the middle to caudal third of the acetabulum can be treated conservatively.3,5,7,13,25,27 Precise reconstruction of the acetabulum is needed for acetabular fracture repair.3,7 Surgical access to the acetabulum requires osteotomy of the greater trochanter to achieve proper exposure. Two- and three-part fractures are most amenable to reconstruction. Stabilization is most commonly achieved via plating, but other techniques have also been described.3,5,7 Femoral head and neck ostectomy is an option for comminuted acetabular fractures or injuries resulting in severe cartilage damage to either the femoral head or acetabulum.3,7
Prognosis
Conservative or surgical management generally provides a good long-term outcome for dogs and cats with pelvic fractures.3,4,7,19,21 Dogs treated with conservative management may show some gait abnormality in the pelvic limbs and changes in the percentage of body weight distribution in all limbs.28 Some degree of osteoarthritis can be seen in most patients with fractures that involve the acetabulum. Narrowing of the pelvic canal ≥45% could increase the risk for chronic constipation or obstipation, which can negatively affect long-term quality of life.4,21 Subtotal colectomy is the preferred treatment for healed pelvic fractures with narrowing resulting in obstipation or constipation that has been present >6 months.4,13,29 Conservative and surgical treatments offer good prognoses for patients with sacroiliac luxation.3,7,19,27
Clinical Follow-Up & Monitoring
All dogs and cats with pelvic fractures need cage rest for 2 to 8 weeks.3,7,30 In the author’s experience, follow-up radiography to look for evidence of shifting fracture segments is recommended in patients not improving within 2 weeks of conservative management, as impingement of the sciatic nerve or pelvic canal narrowing can result. In the author’s clinic, patients managed either conservatively or surgically are re-evaluated with radiography every 4 weeks until fracture healing is confirmed.
Patients with neurologic compromise and positive sensation are expected to have significant improvement over the first 6 to 8 weeks, with full recovery after an additional 12 to 16 weeks or longer.26 Patients presented with no sensation are at high risk for permanent neurologic dysfunction; however, if sensation returns in the first 1 to 2 weeks, prognosis for full or functional recovery is good.26
Rehabilitation modalities (eg, passive range of motion, massage, low-level laser, hydrotherapy) may help improve recovery time.31 Some patients develop short-term constipation, and stool softeners or enemas may be required.
Conclusion
Pelvic fractures are common sequelae of traumatic injury. Comorbidities involving the thoracic and/or abdominal cavities are not unusual. Treatment for pelvic fractures should be determined based on fracture configuration, displacement of fracture segments, patient comfort, and owner expectations and financial concerns.