Pancreatitis in Cats
Cynthia R. Ward, VMD, PhD, DACVIM (SAIM), University of Georgia

Pancreatitis in cats lacks distinctive clinical signs and diagnostic criteria, making it difficult to differentiate from other diseases, and is caused by inflammation of the exocrine pancreas that results in premature activation of trypsin in pancreatic acinar cells.1,2 Trypsin activates normally quiescent proenzymes in cellular zymogen granules, resulting in inflammation, increased vascular permeability, edema, and necrosis. Inflammation can be severe and may result in systemic inflammatory response syndrome, multiple organ dysfunction, and death.3,4
Pancreatitis is commonly classified as either acute (based on infiltration of neutrophilic inflammatory cells) or chronic (based on fibrosis).1,2 Monitoring of clinical disease progression, including rechecking diagnostic test results, often dictates classification; histopathology and biopsy are rarely used. A continuum of disease is most likely, and cats can be presented at any stage of the spectrum.
Incidence is unknown because pancreatitis can be difficult to diagnose, especially in the presence of more easily recognized concurrent diseases. One study examined histopathology in cats presented for necropsy regardless of cause of death2; 67% of cats had some degree of acute pancreatic inflammation, even though 45% of those were clinically normal. This prevalence is higher than what has been found in previous studies, suggesting pancreatitis may often go unrecognized.
Pancreatitis in cats is part of triaditis, a complex of diseases that also includes inflammatory bowel disease and cholangitis/cholangiohepatitis.5 Because clinical signs of these diseases overlap, pancreatitis can be difficult to recognize as a separate disease entity.
Pancreatitis has been reported to be associated with hepatic lipidosis6,7 and has a complex association with diabetes mellitus. Although it is unclear whether the underlying disease is diabetes mellitus or pancreatitis, they are linked, and hyperglycemia causes pancreatic neutrophil infiltration and serum feline pancreatic lipase immunoreactivity (fPLI).8-10
History & Clinical Signs
Pancreatitis is challenging to diagnose in cats because clinical signs can be vague. Unlike presentation in dogs, cats rarely exhibit abdominal pain, have a history of dietary indiscretion, or ingest high-fat meals. The most common clinical signs are inappetence, lethargy, dehydration, and vomiting1,3,11; icterus and weight loss are also possible.
Cats may be presented with clinical signs (eg, diarrhea from inflammatory bowel disease, severe icterus from cholangitis/cholangiohepatitis or hepatic lipidosis) consistent with concurrent diseases that are more easily diagnosed than pancreatitis. Cats with concurrent diabetes mellitus may have polyuria, polydipsia, or polyphagia. Those with previously controlled diabetes may develop insulin resistance or ketosis in response to emergent pancreatitis.9
Diagnosis
Nonspecific clinical signs and comorbidities associated with pancreatitis in cats necessitate evaluation of many factors (eg, clinical signs, routine blood work, specific serum pancreatic testing, imaging) to provide the most effective treatment. Common CBC abnormalities include anemia (regenerative or nonregenerative), lymphopenia, neutrophilia, and thrombocytopenia. Elevated ALP and ALT, hyperbilirubinemia, hypokalemia, hyperglycemia, and hypocalcemia can be seen on serum chemistry profile.1,3,4,12 Hypocalcemia is associated with a severe, necrotizing form of pancreatitis that may require aggressive treatment.13
Serum amylase and lipase activities have been shown to be nonspecific for pancreatic damage and do not provide diagnostic benefit1; however, fPLI is thought to be pancreas specific and is released when pancreatic tissue is damaged. Measurement of fPLI is the most useful laboratory test for antemortem diagnosis12,14-16 and is commercially available as an external quantitative assay and as a semiquantitative in-clinic assay that gives a normal or abnormal result. There is good correlation between test results, but sensitivity and specificity are limited.12,14,15 The external quantitative assay may be most sensitive in cases of acute pancreatitis. Sensitivity and specificity of serum fPLI are ≈79.4% and 79.7%, respectively.14
Abdominal ultrasonography is increasingly important for diagnosing pancreatitis via identification of pancreatic enlargement, changes in echogenicity, free fluid surrounding the pancreas, and hyperechogenicity of peripancreatic fat (Figures 1 and 2). Results of a study demonstrated good correlation with fPLI elevations.16
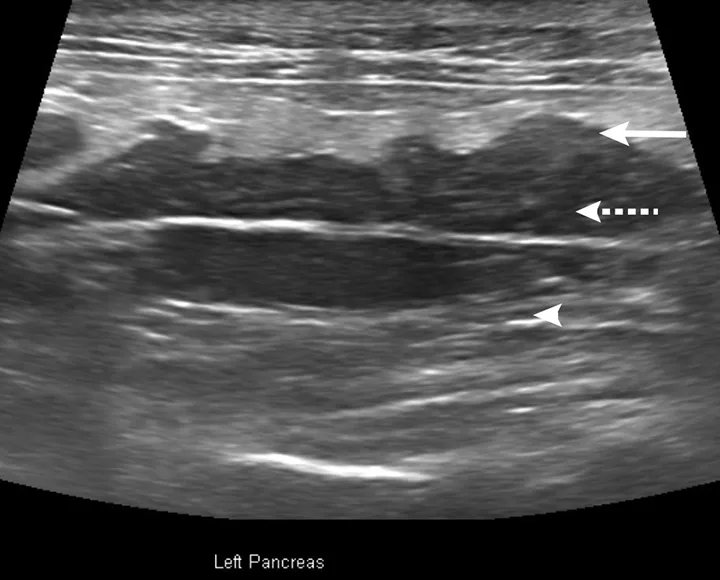
Abdominal ultrasound of a cat with acute pancreatitis and triaditis. Hypoechogenicity of the pancreas (dashed arrow), hyperechoic mesentery (steatitis; arrowhead), and irregular, lobulated pancreatic margins (arrow) are visible.
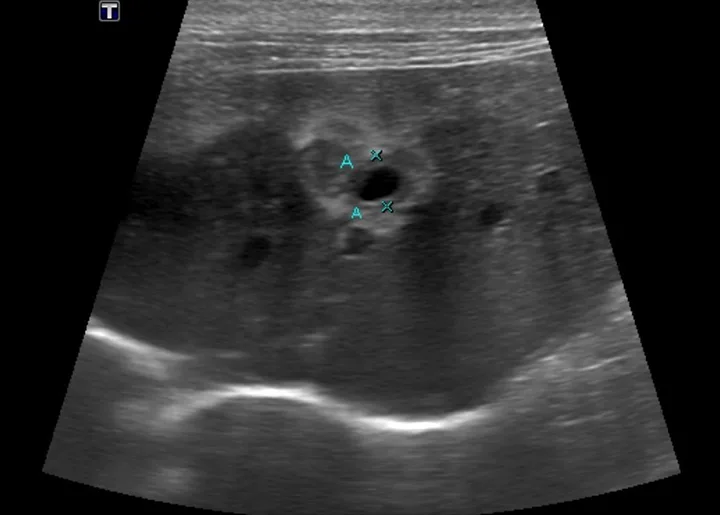
Ultrasound of the liver and common bile duct in a cat with acute pancreatitis and triaditis. Hypoechogenicity of the liver and an enlarged common bile duct (As; 5 mm measured by Xs) with thickened walls are visible.
Treatment & Management
There is no specific treatment for feline pancreatitis. Successful management centers around fluid therapy, nutritional support, pain control, and correction of concurrent clinical abnormalities.
Inpatient
Patients with acute disease, including those with fever, tachypnea, tachycardia, systemic inflammatory syndrome, or circulatory shock, should be hospitalized and aggressively treated.
Crystalloid fluids are a mainstay of treatment, providing perfusion of the inflamed pancreas as well as cardiovascular support. Treatment goals should include replacement of circulating fluid volume and maintenance of pancreatic perfusion to prevent necrosis. Colloids can be added to provide oncotic support, and fresh frozen plasma can be added to replace coagulation factors. Initial resuscitation can involve a combination of crystalloid and colloid fluids. Electrolyte abnormalities (eg, hypokalemia, hypocalcemia) should be anticipated and treated when identified.
Analgesia is important, but pain can be difficult to identify in cats. Narcotics, including parenteral and transdermal fentanyl (4 µg/kg/hour transdermal patch [12 µg/hour patch or 25 µg/hour patch in larger cats] or 1-5 µg/kg/hour CRI; Schedule II), are usually most effective. Buprenorphine (0.01-0.03 mg/kg buccally; Schedule III) can be used initially while fentanyl reaches therapeutic effect, usually within 12 to 24 hours.
Vomiting should be controlled to facilitate patient comfort and minimize fluid loss. Multiple antiemetic agents are often necessary to control emesis. Maropitant (1 mg/kg SC every 24 hours or 2 mg/kg PO every 24 hours) has antinociceptive effects in addition to antiemetic properties and can be used alone or with a 5-HT3 receptor antagonist (eg, ondansetron, 0.5 mg/kg IV loading dose, followed by 0.5 mg/kg/hour CRI for 6 hours or 0.5-1 mg/kg PO every 12-24 hours; dolasetron, 1 mg/kg IV or PO every 24 hours).
Because diabetes mellitus is a common comorbidity, glucose should be closely monitored and maintained in a normal range. Even mild hyperglycemia should be corrected with small amounts of insulin (regular insulin, 0.1 U/kg IM every 6-8 hours) to help prevent further damage to the pancreas and diabetes mellitus as a sequela to pancreatitis.
Prednisolone can be beneficial for treatment and/or prevention of chronic pancreatitis because of anti-inflammatory and antifibrotic activities. Standard treatment protocols are not available; recommendations have been made for anti-inflammatory (0.5-1 mg/kg PO every 24 hours) and immunosuppressive dosages (1-2 mg/kg PO every 12 hours).17 Development of diabetes mellitus is a potential adverse effect; cats receiving prednisolone should undergo frequent serum glucose evaluations. Serum fPLI can be measured to detect resolution of inflammation. Cyclosporine (5 mg/kg PO every 24 hours) can be used in cats that do not tolerate prednisolone.
It is crucial to provide adequate nutrition early, as pancreatitis can lead to hepatic lipidosis. Appetite stimulants (eg, mirtazapine, 1.88-3.75 mg per cat PO every 24 hours or 2 mg per cat transdermal on ear pinna every 24 hours) are effective in cats. Cyproheptadine (1 mg per cat PO every 12 hours), a histamine H1- and 5HT-receptor antagonist, can also be used but has limited efficacy.
In cats that remain anorexic, feeding tubes can be used to deliver enteral nutrition. Nasoesophageal tubes can be placed in cats that can maintain an upright position. Esophagostomy tubes, which can be placed as soon as the cat can be anesthetized, allow administration of a larger variety of foods and can be managed at home on a long-term basis. Hydration can be maintained via water supplementation through the tube.
Outpatient
Cats that are hemodynamically stable and presented with chronic weight loss, occasional vomiting, hyporexia, and lethargy can be treated on an outpatient basis. Emesis and pain should be controlled, and nutritional support should be provided. Early placement of feeding tubes allows control of nutrition and hydration at home. Pet owners may administer SC fluids to control hydration status in cats that do not have feeding tubes. Cats should be monitored for appetite so appropriate nutrition is maintained; appetite stimulants (eg, mirtazapine) can be used as necessary.
Prognosis & Prevention
Accurate prognostic numbers are not available because pancreatitis is difficult to diagnose and often confused with other diseases.
The etiology of pancreatitis is unknown; thus, prevention strategies are limited. Prednisolone may have some preventive activity, although its use for this purpose is controversial. Diabetes mellitus, hepatic lipidosis, inflammatory bowel disease, and cholangitis/cholangiohepatitis may contribute to pancreatitis and can affect control of pancreatic inflammation. Affected cats should be monitored for concurrent disease to prevent recurrence of pancreatitis.
Unlike in dogs, pancreatitis in cats has no link with high-fat diets; therefore, a low-fat diet is not likely to prevent disease. Dietary modification for treatment and/or prevention may include a novel protein or hypoallergenic diet to control inflammatory bowel disease.