Oronasal Fistulae at a Glance
Oronasal fistulae present in multiple forms and do not necessarily refer to a mouth–nasal cavity interaction that is associated with a diseased maxillary canine tooth. This image gallery illustrates a variety of clinical presentations of oronasal fistulae and their surgical management in canine, feline, and pediatric patients.
Related Article: Treatment Options for Oronasal Fistulae

Case 1: Repair of a Chronic Oronasal Fistula
Typical appearance of a chronic, nonhealing oronasal fistula following closed extraction of the left maxillary canine tooth (204).

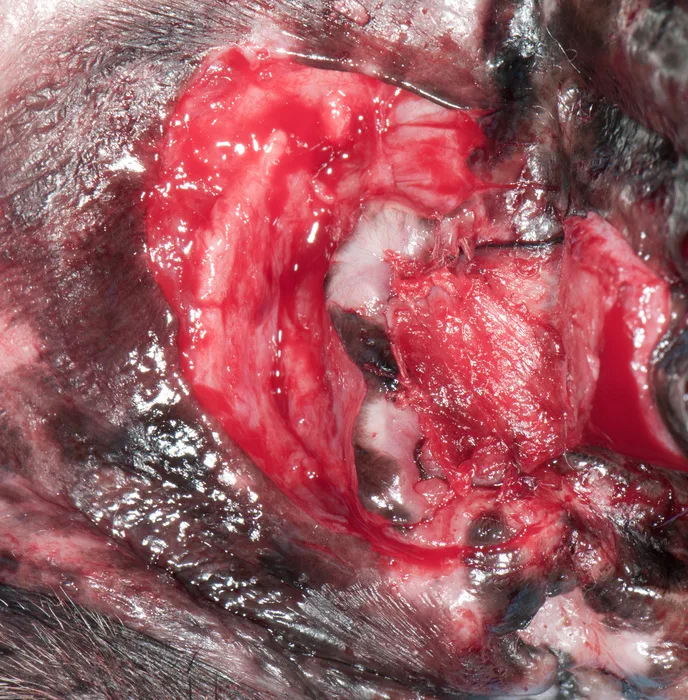
Case 1: Repair of a Chronic Oronasal Fistula
The left maxillary quadrant of a dog following extraction of adjacent third incisor and second premolar because of chronic periodontitis.
Case 1: Repair of a Chronic Oronasal Fistula
Elevation of the single mucoperiosteal pedicle flap using a Freer periosteal elevator created by making a single rostral divergent vertical releasing incision.

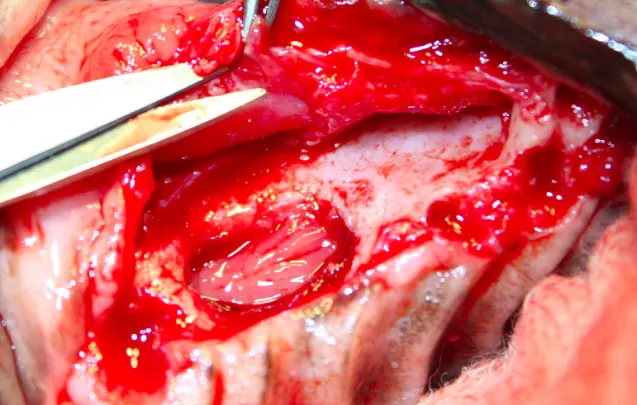
Case 1: Repair of a Chronic Oronasal Fistula
Surgical debridement of the edematous and epithelialized tissue margins is performed.

Case 1: Repair of a Chronic Oronasal Fistula
A periosteal releasing incision is created using a small, sharp iris scissors to ensure a tension-free closure. Note the Adson 1X2 tissue forceps engaging the underside of the flap rather than at the free flap margin. This prevents crushing trauma to the free flap margin, which can impair healing.
Case 1: Repair of a Chronic Oronasal Fistula
The single mucoperiosteal pedicle flap after tension-free closure. A 4-0 or 5-0 absorbable monofilament suture on a small taper needle in a simple interrupted pattern is preferred.

Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
Typical appearance of a nonhealing chronic oronasal fistula following extraction of the left maxillary canine tooth (204). Photograph courtesy of Dr. Jan Bellows
Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
Surgical debridement of the lesional margins is required before revisional surgery. Photograph courtesy of Dr. Jan Bellows

Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
A partial-thickness palatal mucosal hinge flap is created by making two parallel incisions; one rostral and one distal to the defect margins connected palatally by a third incision. Photograph courtesy of Dr. Jan Bellows
Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
The hinge flap is rotated and placed across the defect. The flap edges are then sutured to the buccal surface of the previously debrided gingival collar. Photograph courtesy of Dr. Jan Bellows

Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
The hinge flap is in place covering the defect. Mesial and distal vertical releasing incisions into alveolar mucosae are used to create a separate single mucoperiosteal pedicle flap. Photograph courtesy of Dr. Jan Bellows

Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
After incising and releasing the periosteum that is attached to the flap, the mucoperiosteal flap is advanced over the previously created palatal mucosal defect and sutured with 4-0 polyglactin 910 on a small taper needle in a simple interrupted pattern. This creates a double-layer closure of the oronasal fistula. Photograph courtesy of Dr. Jan Bellows
Case 2: Double-Layer Closure of Nonhealing Chronic Oronasal Fistula
Clinical appearance of the healed double-layer closure of a chronic oronasal fistula 6 weeks post-operatively. Photograph courtesy of Dr. Jan Bellows
Case 3: Traumatic Midline Palatal Defect
Typical appearance of a traumatic midline palatal defect in a cat. The lesion involves the hard and soft palates. Cats that suffer high-rise or high-impact trauma frequently develop similar linear midline palatal defects. Photograph copyright Dr. Alexander M. Reiter
Case 3: Traumatic Midline Palatal Defect
Wound margins are debrided and bilateral incisions are made approximately 3 mm from palatal margins of the dental arcade. Incisions are extended from the maxillary second premolar to the level of the first molar, and the flaps are elevated until freely moveable and able to be apposed with no tension. Palatal mucosa is apposed using a horizontal mattress pattern. Soft palate is closed in two layers. Photograph copyright Dr. Alexander M. Reiter
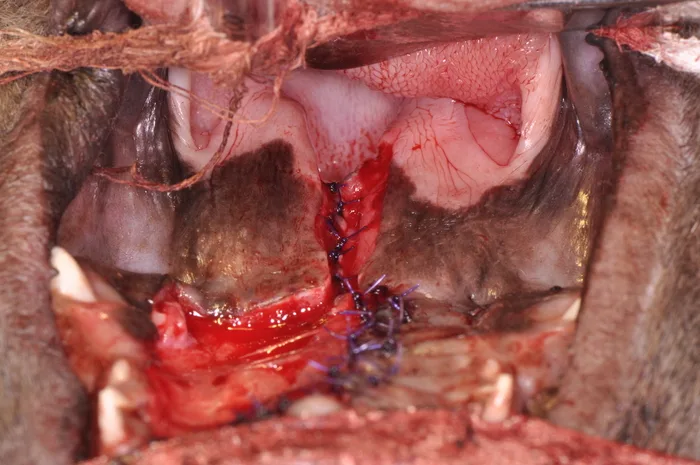
Case 4: Congenital Cleft of the Hard and Soft Palates
Midline congenital cleft of the hard and soft palates in a French bulldog (5 months of age). Photograph copyright Dr. Alexander M. Reiter
Case 4: Congenital Cleft of the Hard and Soft Palates
An indelible marker outlines where incisions are to be made to create a palatal mucosal hinge flap to the left of the defect and to expose palatal mucosa on the right side of the defect. Photograph copyright Dr. Alexander M. Reiter
Case 4: Congenital Cleft of the Hard and Soft Palates
Stay sutures help maneuver the hinge flap into position between the palatal process of the maxilla and the palatal mucosa on the right side. Photograph copyright Dr. Alexander M. Reiter
Case 4: Congenital Cleft of the Hard and Soft Palates
A singe overlapping pedicle flap of the palatal mucosa is created to the right of the defect and sutured to the hinge flap using an alternating horizontal mattress and single interrupted suture pattern. The soft palate must be closed in 2 layers. In this figure only the nasal mucosal layer has been reapposed. Photograph copyright Dr. Alexander M. Reiter
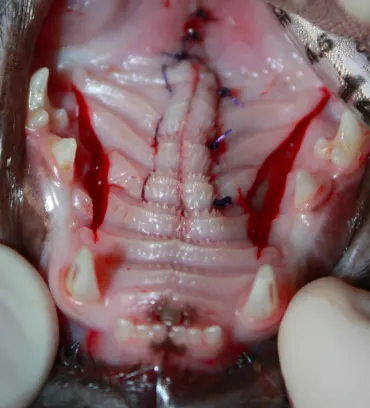
Case 4: Congenital Cleft of the Hard and Soft Palates
Postoperative image of palatal reconstruction. Note the oral mucosa of the soft palate has been reapposed in a second layer using 4-0 absorbable monofilament suture on a small taper needle in a simple interrupted pattern. Flap vitality is maintained by preserving the major and accessory palatine arteries (large and small arrows, respectively). Photograph copyright Dr. Alexander M. Reiter
Case 5: Hard Palate Defect
A traumatic defect of the hard palate in a Pomeranian (3 years of age). Photograph copyright Dr. Alexander M. Reiter
Case 5: Hard Palate Defect
Custom-made palatal obturators created using a vinypolysiloxane negative of the defect. The pink-colored obturator is fabricated with methylmethacrylate, while the off-white obturator is fabricated with bisacryl provisional composite resin. More than one prosthetic is created in the event that the first is lost. Photograph copyright Dr. Alexander M. Reiter
Case 5: Hard Palate Defect
Palatal defect is covered using a palatal obturator fabricated from a bisacryl provisional composite resin. The prosthetic is removed q6mo under sedation for cleaning and irrigation. If the prosthetic becomes loosened or no longer fits, a new obturator can be customized. Photograph copyright Dr. Alexander M. Reiter