Optic Neuritis
Thomas Chen, DVM, DACVO, University of Tennessee
Anansa Persaud, DVM, Long Island Veterinary Specialists, Plainview, New York
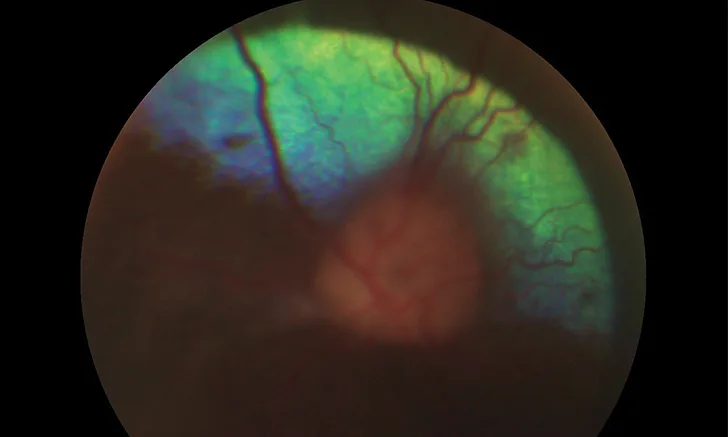
Optic neuritis in a dog. The optic nerve and its associated blood vessels are hazy with indistinct borders, as the vessels are elevated relative to the retinal blood vessels surrounding the nerve.
Optic neuritis is a rare but serious condition that can result in acute blindness or visual deficits in one or both eyes.1,2 Prompt diagnosis and treatment are necessary to recover vision, and evaluation for neurologic, infectious, and/or neoplastic disease may also be warranted.1,3,4
Clinical Signs
In cases of bilaterally affected animals, owners often report suspected vision loss based on a clinical history of the pet bumping into walls or objects, missing treats, or having difficulty with stairs. Astute owners of pets with unilateral disease may report more subtle changes (eg, visual deficits, anisocoria with the dilated pupil in the affected eye).
Absent menace responses, with absent pupillary light reflexes and mydriatic pupils, are usually noted on ophthalmic examination.1,5 Further vision testing (eg, visual placement testing, maze) can help confirm lack of vision.
A thorough fundic examination is crucial for including optic neuritis in the list of diagnostic differentials. The optic nerve head most often appears swollen, hyperemic, or elevated (Figure 1). Chorioretinitis with associated focal retinal detachment or edema, hemorrhage, or white or gray foci can also be present adjacent to or near the optic nerve head. Rarely, inflammation can also occur posterior to the optic nerve head (retrobulbar) and therefore cannot be appreciated except with advanced imaging (eg, MRI).5
Diagnosis
Optic neuritis is often diagnosed by confirmation of blindness and pupillary light reflex deficits and visualization of an abnormal optic nerve head on fundic examination. Other important rule outs for blindness can include diffuse retinal detachment (in contrast to focal detachment proximal to the optic nerve head) and sudden acquired retinal degeneration syndrome. Retinal detachment can also be diagnosed on fundic examination, whereas sudden acquired retinal degeneration syndrome can only be confirmed with an electroretinogram. Performing a complete neurologic examination and obtaining a thorough history are also recommended to assess for concurrent neurologic signs that might be suggestive of meningoencephalitis.
Causes
Optic neuritis in dogs is most often the result of immune-mediated and/or inflammatory brain disease, which together comprise approximately 80% of optic neuritis cases in a study of 96 dogs.1 Other causes in dogs include infection or neoplasia. Optic neuritis in cats occurs secondary to infectious6-9 or neoplastic causes,5 with no reports of immune-mediated causes or incidence rates for all causes in cats.
Immune-Mediated
Immune-mediated optic neuritis appears to be the most common diagnosis in dogs.1,5 The optic nerve is a direct extension of the CNS; therefore, inflammatory brain disease can extend to or focally involve the optic nerves, usually bilaterally. Meningoencephalitis of unknown etiology (MUE; or, when confirmed histologically, subtyped more specifically as granulomatous meningoencephalitis [GME]) is one such condition10 and has been categorized by neurologists as ocular GME when inflammation involves the optic nerves, either alone or with concurrent MUE/GME signs.11
In contrast, veterinary ophthalmologists have historically considered optic neuritis (in patients without concurrent neurologic clinical signs) a separate clinical entity from MUE.2 A difference in signalment in canine patients with isolated involvement of the optic nerves has been reported; MUE patients were typically female small-breed dogs, whereas isolated optic neuritis patients were often male medium-to-large–breed dogs.1 The exact relationship or difference between the syndromes, if it exists, has not yet been definitively determined.
Whether a manifestation of MUE or isolated immune-mediated optic neuritis, definitive diagnosis often requires an MRI and CSF tap while also ruling out other infectious or neoplastic diseases; however, many owners often decline advanced imaging or CSF taps due to cost or availability.1
Infectious Disease
Infectious diseases, with tropism for or involvement of the CNS, have also been reported to cause optic neuritis. Infectious optic neuritis usually manifests as an extension of more generalized or multifocal meningoencephalitis or from ocular and orbital involvement. Fungal disease in particular can involve the orbit or neighboring areas (eg, nasal or sinus cavities) and may result in subsequent involvement and inflammation of the optic nerve.1,12 Viral diseases (eg, distemper, tick-borne encephalitis virus, feline infectious peritonitis) affect the nervous tissue directly or indirectly via damage from host immune responses. These diseases can also result in uveitis (both anterior and posterior) or chorioretinitis (not necessarily associated with the optic nerve), the presence of which should raise clinical suspicion of infectious disease as compared with immune-mediated meningoencephalitis.
In dogs, optic neuritis has been reported with distemper virus, tick-borne encephalitis virus, ehrlichiosis, Toxoplasma gondii or Neospora caninum infections, and fungal disease (eg, aspergillosis, cryptococcosis, histoplasmosis, blastomycosis).1,13-20 In cats, T gondii infections, feline infectious peritonitis, and systemic fungal disease (ie, histoplasmosis, cryptoccosis) have been reported with optic neuritis.6-9,17,21
Infectious disease testing should be conducted based on clinical suspicion from history and signalment (eg, unvaccinated animal, use of tick preventives), geography (for fungal disease), tick exposure, and exploratory bloodwork.
Neoplasia
Primary optic nerve tumors, including optic nerve meningioma and gliomas, have been reported, although they are rare.1,5,22,23 Orbital neoplasia can also affect the optic nerve. In a case series involving 53 neoplastic cases, carcinomas were seen most commonly (30%), followed by sarcomas (20%), lymphoma (15%), and presumptive meningiomas (17%).5 Carcinomas and sarcomas were noted to occasionally arise from neighboring areas of the orbit (ie, frontal bone or sinus, nasal cavity, maxilla) that extended into the orbit with involvement of the optic nerve.
Extension of Orbital Disease
Optic neuritis may also occur secondary to orbital inflammation, including retrobulbar cellulitis and/or abscessation, which can be associated with infection, neoplasia, foreign body, or dental disease.5,8,19,24-28 If inflammation is severe or near enough to the optic nerve, compression or inflammation of the optic nerve can result in subsequent blindness. Clinically, these conditions can be observed as change in the position or placement of the eye (eg, enophthalmia, exophthalmia), protrusion of the third eyelid, and/or difficulty or pain on opening of the mouth, with periocular swelling and inflammation. Optic neuritis secondary to orbital or retrobulbar inflammation can be unilateral depending on the laterality of the primary disease (eg, unilateral in bacterial retrobulbar cellulitis).
Treatment & Prognosis
Ultimately, treatment of optic neuritis depends on the underlying cause. Because immune-mediated causes largely predominate, treatment typically involves short-term immunosuppressive doses of steroids (Figure 2). Partial or full return of vision was noted in approximately 30.6% (22/72) of dogs in one study1 and 64% (7/11) of dogs in another.4 Return of vision 1 to 2 weeks after initiating therapy for acute blindness has been noted (author experience).
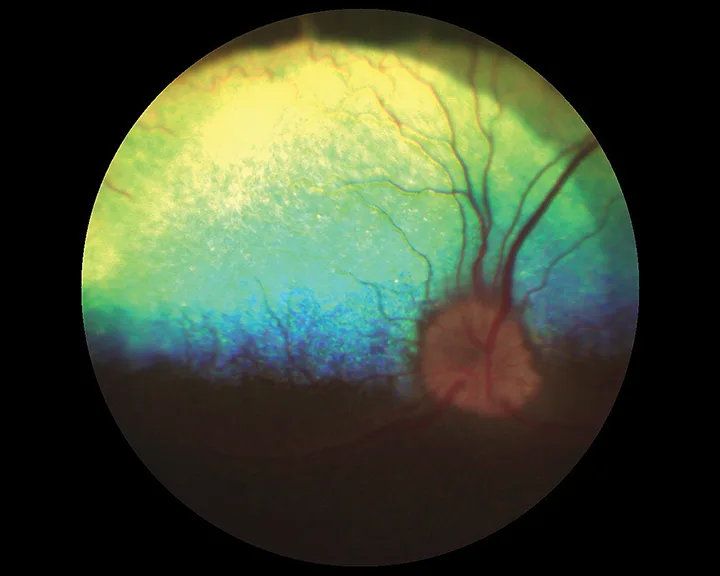
Same dog as in after a month of prednisone and cytarabine treatment. The margins around the optic nerve are still indistinct but much improved. Vessels overlying the nerve can be clearly seen and are in the same plane as the surrounding retinal blood vessels.
Recurrence has been noted in 2 cases at 15 and 18 months after successful treatment and at 2 weeks after tapering steroids.1 For optic neuritis that is suspected to be occurring secondary to MUE, treatment recommendations by neurologists generally entail life-long administration of steroids and/or immunomodulatory agents.11
Immunosuppressive doses of steroids can be detrimental if an underlying infection is present and may mask clinical signs or delay diagnosis if an underlying neoplastic disease is present. Any indication of orbital disease should be closely investigated before initiating steroidal treatment. Ideally, infectious disease should be ruled out, with specific testing conducted before initiating steroidal treatment, and an MRI and CSF tap performed to definitively rule in immune-mediated optic neuritis. However, if regaining vision is a priority and immune-mediated disease is suspected, empiric treatment with steroids can be initiated, as long as owners are educated regarding the risks.
Specific treatment for infectious disease or neoplasia will vary depending on the causative or suspected causative agent. Prognosis varies depending on CNS involvement and severity of primary disease but, for vision, is generally considered poor.