Ocular Pain & Vision Loss in a Golden Retriever
Andrew Christopher Lewin, BVM&S, DACVO, University of Tennessee
Clinical History & Signalment
Trigger, a 6-year-old neutered male golden retriever, was presented for a 48-hour history of blepharospasm, ocular discharge, and excessive tearing in the left eye. His owner reported he had been pawing at the eye and surrounding region over the previous 48 hours. He was lethargic and hyporexic and had bumped into objects several times at home in the previous 24 hours.
Physical Examination
Routine physical examination results were normal, and a complete ophthalmic examination was performed.
Findings in the Right Eye
Menace response, direct pupillary reflex, palpebral reflex, and dazzle reflex were normal. Consensual pupillary reflex was absent. Schirmer tear test was 23 mm/minute (normal, 15-25 mm/minute). Intraocular pressure was 8 mm Hg (normal, 10-20 mm Hg via rebound tonometer). Fluorescein staining was negative for uptake by the cornea.
The cornea was intact with a normal tear film during magnified diffuse and slit-beam examination. Mild conjunctival hyperemia, iridal hyperpigmentation, lenticular nuclear sclerosis, multifocal paraxial regions of pigmentation in a radial arrangement on the anterior lens capsule, and a small amount of visible free pigmented cells in the anterior chamber with mild (trace) aqueous flare (aqueous flare scale, trace to 4+) were also present (Figure 1).
Gonioscopy showed a normal, open iridocorneal angle. Fundoscopy using binocular indirect ophthalmoscopy with a 28-diopter lens revealed a normal fundus.

Conjunctival hyperemia, lenticular nuclear sclerosis, iridal hyperpigmentation, and radially arranged pigmentation visible on the anterior lens capsule in Trigger’s right eye. Image courtesy of Louisiana State University School of Veterinary Medicine Ophthalmology Service
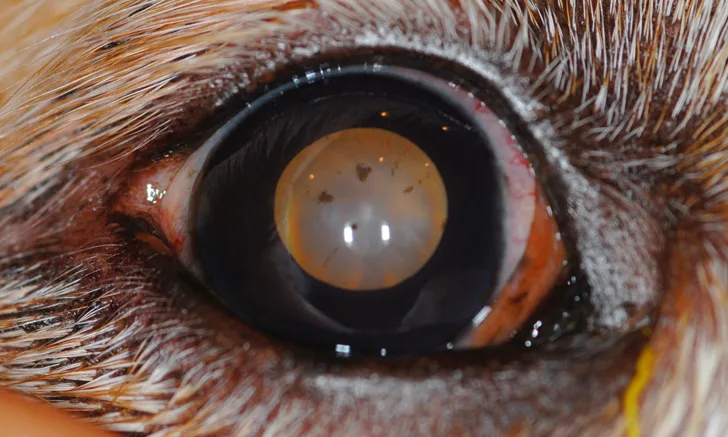
Findings in the Left Eye
Menace response, direct pupillary reflex (midrange pupil [ie, neither miotic nor mydriatic]), consensual pupillary reflex, and dazzle reflex were absent. Palpebral reflex was normal. Schirmer tear test was >30 mm/minute (normal, 15-25 mm/minute). Intraocular pressure was 58 mm Hg (normal, 10-20 mm Hg via rebound tonometer). Fluorescein staining was negative for uptake by the cornea.
The cornea was intact with a normal tear film during magnified diffuse and slit-beam examination. Evidence of epiphora was present at the medial canthus and surrounding facial skin. Marked conjunctival hyperemia, moderate chemosis, severe aqueous flare (3+), mild hyphema obscuring iridal detail, and mild enophthalmos attributed to blepharospasm, leading to elevation of the third eyelid, were also observed (Figure 2).
Intraocular structures were not visible via gonioscopy. Fundoscopy examination using binocular indirect ophthalmoscopy with a 28-diopter lens revealed only the tapetal reflex due to anterior segment abnormalities.

Conjunctival hyperemia, loss of intraocular detail, and elevation of the third eyelid in Trigger’s left eye. Image courtesy of Louisiana State University School of Veterinary Medicine Ophthalmology Service
DIAGNOSIS:
BILATERAL GOLDEN RETRIEVER PIGMENTARY UVEITIS WITH SECONDARY GLAUCOMA IN THE LEFT EYE
Diagnosis
Based on ocular examination findings and signalment, Trigger was diagnosed with golden retriever pigmentary uveitis (GRPU) in both eyes and secondary glaucoma in the left eye.
Evidence of uveitis (ie, iridal hyperpigmentation, free pigmented cells in the aqueous humor, mild ocular hypotony, conjunctival hyperemia, aqueous flare) was detected in the right eye, and, although views of intraocular structures were limited in the left eye, most cases of GRPU are bilateral (59%-89%).1,2 In addition, because there was no evidence of goniodysgenesis in the right eye and there were no concurrent physical examination abnormalities or concurrent ocular findings in the left eye, glaucoma in the left eye was believed to be secondary to GRPU. Diffuse hyphema in the left eye was attributed to chronic inflammation associated with GRPU.
Treatment & Management
GRPU in Trigger’s right eye led to uveitis but not glaucoma. Topical and systemic NSAIDs and topical and systemic corticosteroids were considered to control inflammation (see Treatment at a Glance). The eye was initially treated with topical diclofenac 0.1% ophthalmic solution every 8 hours because inflammation in the eye was mild, and topical NSAIDs are typically associated with few adverse effects.
Topical ocular antihypertensive medications, specialty glaucoma surgery, and surgical salvage were considered for treatment of glaucoma in Trigger’s left eye. Restoration of vision was unlikely given the lack of menace response, pupillary light reflexes, and dazzle reflex. Trigger’s owner decided not to pursue medical management due to the associated poor prognosis for vision and potential for long-term discomfort. The left eye was surgically removed using a closed transpalpebral enucleation technique and submitted for histopathology, which confirmed the diagnosis of GRPU with secondary glaucoma.
TREATMENT AT A GLANCE
Treatment options are limited for GRPU, and the underlying disease process is incompletely understood.
Standard of care for GRPU is topical and/or systemic anti-inflammatory medications.
Long-term treatment is usually required.
Medications to control glaucoma should be administered as needed.
Salvage procedures (eg, enucleation) should be considered for eyes that are permanently blind and painful.
Prognosis & Outcome
The enucleation site healed uneventfully. Vision was maintained in his right eye, which remained apparently comfortable with normal intraocular pressure (10 mm Hg) 6 months later. Topical diclofenac 0.1% ophthalmic solution every 12 hours in the right eye was the only medication continued at the 6-month follow-up. In most cases, long-term anti-inflammatory treatment is recommended. Long-term anti-inflammatory drugs and routine recheck appointments every 3 to 6 months were recommended for Trigger.
Discussion
GRPU (ie, pigmentary uveitis, golden retriever uveitis) is a common, most likely inherited condition in golden retrievers that can vary in severity (see Take-Home Messages).3 In the United States, ≈5% to 25% of golden retrievers are affected.3 The hallmark of the GRPU phenotype is radially oriented pigment on the anterior lens capsule. Mildly affected patients have a small amount of radially oriented pigment deposition on the anterior lens capsule. Severely affected patients can have radial pigmentation on the lens capsule, fibrinous material in the anterior chamber, and vision- and globe-threatening complications (eg, glaucoma). Affected dogs are most often diagnosed between 4 and 8 years of age.
GRPU diagnosis should be made in golden retrievers when radial pigment is present on the anterior lens capsule, even in the absence of other findings (eg, iridal hyperpigmentation, aqueous flare).3 GRPU is not the only potential cause of uveitis, hyphema, or glaucoma in this breed. Thorough physical and ocular examinations should be supported with appropriate diagnostic testing when the diagnosis is not clear.
Although not seen in this case, uveal cysts are commonly found in patients with GRPU and are a significant risk factor for development of GRPU in golden retrievers.3 Visualization of uveal cysts is not necessary to diagnose GRPU, as only 13.3% to 42% of eyes with GRPU have this finding on examination.3 When ultrasound biomicroscopy is used, however, 100% of eyes affected with GRPU contain multiple uveal cysts.3,4 This discrepancy is because eyes with GRPU are often affected by miosis, which may prevent complete examination of the posterior chamber.
GRPU occurs almost exclusively in golden retrievers and is therefore strongly suspected to be inherited. Because of the potential for severe visual impairment and ocular pain, breeding dogs affected with GRPU is not recommended5; however, late onset (ie, 4-8 years) has led to difficulties in preventing breeding of affected dogs.
Treatment for GRPU
Treatment is challenging because underlying pathophysiology is not completely understood. Although it is assumed that GRPU has an inflammatory component, histologic confirmation is not always possible.2 Regardless, topical or systemic anti-inflammatory medications are the standard of care.3
Topical NSAIDs (eg, diclofenac, ketorolac, flurbiprofen) can be used in eyes with mild to moderate intraocular inflammation and should be initially applied every 12 to 24 hours. Frequency can then be tapered to effect. Adverse effects are infrequent, but ocular hypertension may occur.
Systemic NSAIDs (eg, carprofen, meloxicam) can be used in patients with mild to moderate intraocular inflammation. Topical NSAIDs are more often preferred because adverse effects and contraindications are more frequently associated with systemic use.
Topical corticosteroids (eg, dexamethasone, prednisolone) are usually reserved for patients with moderate to severe intraocular inflammation and should be initially applied every 4 to 8 hours. Frequency can then be tapered to effect. Adverse effects include corneal opacification. These drugs are contraindicated in eyes with corneal ulceration.
Systemic corticosteroids (eg, prednisone) are typically reserved for patients with severe intraocular inflammation. Dose recommendations vary, but anti-inflammatory doses (eg, prednisone, 0.5 mg/kg PO every 12 hours, then tapered to effect) are typically used for severe GRPU and tapered to effect. These drugs have numerous adverse effects and contraindications.
Treatment for Glaucoma
Secondary glaucoma and vision loss occur in ≈20% to 45% of eyes with GRPU.1,3,6 Treatment options are limited. There is no difference in disease progression in eyes treated with topical steroids compared with eyes treated with topical NSAIDs, but time between examinations is a significant factor in disease progression.7 Posterior synechiae and fibrinous material in the anterior chamber are significant risk factors for glaucoma development.3,7
Topical ocular antihypertensive medications can be used to treat glaucoma in dogs. Topical dorzolamide 2% ophthalmic solution (typically applied every 8 hours) is preferred for cases of secondary glaucoma. Topical latanoprost 0.005% ophthalmic solution (typically applied every 12 hours) is usually avoided in patients with secondary glaucoma because it can exacerbate underlying uveitis. Topical timolol 0.5% ophthalmic solution (typically applied every 12 hours) is usually inadequate for reduction of severely elevated intraocular pressure.
Specialty glaucoma surgical procedures are another treatment option. Transscleral diode cyclophotocoagulation can be used to control intraocular pressure in some cases.1 A surgical salvage procedure (eg, enucleation) is typically warranted in painful, permanently blind eyes. Elevated intraocular pressure is considered painful.
TAKE-HOME MESSAGES
GRPU is a common, inherited ocular disease in golden retrievers.
Radial pigment deposition on the anterior lens capsule is the hallmark clinical finding.
Many cases of GRPU progress to secondary glaucoma and vision loss.
GRPU is most often a bilateral disease.
There are numerous causes of uveitis in golden retrievers, and a thorough systemic and ocular diagnostic investigation should be pursued in all cases.
Referral to a veterinary ophthalmologist for further assessment is recommended in most cases.
Early diagnosis and treatment may help prolong vision.