Nonresponsive Skin Lesions in a Siberian Husky
Andrew Rosenberg, DVM, DACVD, Animal Dermatology & Allergy Specialists, White Plains, New York, and Riverdale, New Jersey

Trooper, a 3-year-old 67-lb (30.5-kg) intact male Siberian husky, was presented to the dermatology clinic for skin lesions around the eyes. Lesions were first appreciated ≈4 months prior to presentation and showed no response to amoxicillin/clavulanic acid or cefpodoxime, which were prescribed by the primary veterinarian. Treatment with combined trimeprazine/prednisolone twice daily and tapered over 1 month resulted in partial improvement. The affected areas were only mildly pruritic. According to the owner, the lesions around the eyes had worsened, and the scrotum had become inflamed in the previous 4 months.
Physical Examination
On examination, Trooper was bright, alert, and responsive. All peripheral lymph nodes were normal. Periocular regions were alopecic with mild to moderate crusting (Figure). The pinnae were moderately erythematous on the concave surface with mild adherent scaling. The scrotum was severely erythematous. All paw pads were crusted. The remainder of the examination was unremarkable.
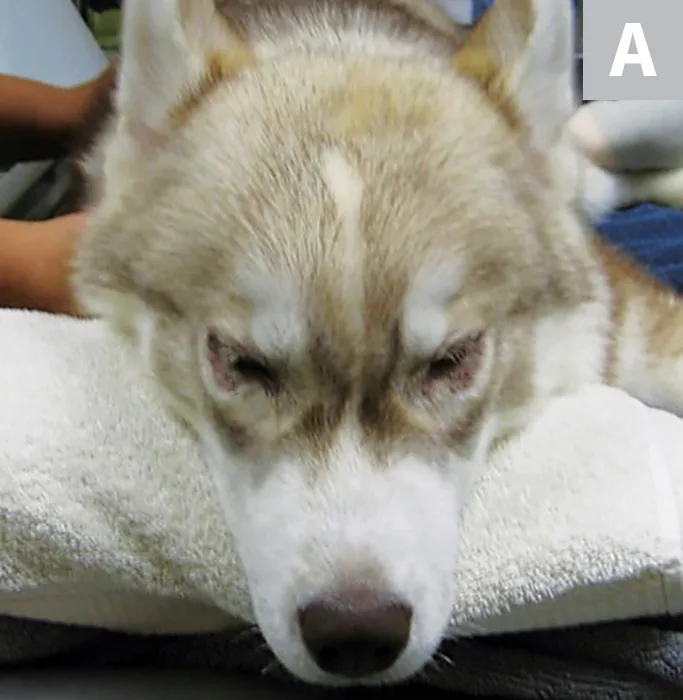


Affected areas showing alopecia (A), crusting (B), and scaling (C)
Diagnosis
Evaluation of an impression smear of the periocular region revealed numerous cocci with streaming neutrophils. A deep skin scrape was negative for ectoparasites. Skin biopsies were discussed with Trooper’s owner; however, superficial pyoderma was initially treated prior to biopsy to ensure accurate results. Bacterial culture and susceptibility testing was performed on the lesions to guide therapy.
Four days after initial presentation, culture results revealed methicillin-resistant Staphylococcus schleiferi (Table). Treatment with chloramphenicol (40 mg/kg every 8 hours) was initiated. In addition, the owner was instructed to bathe Trooper weekly using a 3% chlorhexidine/phytosphingosine shampoo. Due to the location of the periocular lesions, topical therapy did not seem appropriate as the sole means of eliminating pyoderma.
Infection had improved significantly 2 weeks after initial presentation, and Trooper was returned to the clinic for punch biopsies (6 mm) of the affected areas, performed while he was under sedation. The specimens were submitted for histopathology, which confirmed zinc-responsive dermatosis (see Histopathology Results of Punch Biopsies Indicating Marked Parakeratotic Hyperkeratosis).
HISTOPATHOLOGY RESULTS OF PUNCH BIOPSIES INDICATING MARKED PARAKERATOTIC HYPERKERATOSIS
Three specimens of haired skin obtained via punch biopsy were evaluated histologically. In all biopsy samples, marked parakeratotic hyperkeratosis that expanded to the follicular infundibula and into the intrafollicular stratum corneum was apparent. The epidermis was moderately spongiotic, and mild acanthosis and leukocyte exocytosis were observed. The superficial dermis was markedly expanded by edema and a mild interstitial chronic inflammatory infiltrate of small lymphocytes, plasma cells, and fewer granulocytes. Many superficial dermal fibroblasts were plump and reactive; this type of superficial dermal expansion can give the skin surface a papillated appearance. Multifocal small inflammatory aggregates associated with adnexa were observed in 2 sections throughout the dermis; these inflammatory cells included epithelioid macrophages, lymphocytes, plasma cells, and neutrophils. Free keratin (ie, furunculosis) was observed in one of these foci.
Hyperkeratosis, especially of the superficial follicular infundibula, was striking and suggestive of zinc-responsive dermatosis. The superficial dermal edema and foci of furunculosis were suggestive of resolving pyoderma.
Aerobic Culture & Susceptibility Results for Staphylococcus schleiferi 4+ Bacterial Growth*
*S schleiferi is resistant to oxacillin and therefore is methicillin-resistant. All staphylococci are screened for methicillin resistance.
†Oxacillin can be used to predict methicillin sensitivity. Oxacillin-resistant staphylococci are resistant to all cephalosporins, including cefpodoxime and cefovecin.
DIAGNOSIS:
ZINC-RESPONSIVE DERMATOSIS SYNDROME I
Treatment & Long-Term Management
Chloramphenicol therapy was continued for 4 weeks, including 1 week after resolution of clinical signs of infection and cytologic cure. Supplementation with zinc methionine (elemental zinc, 3 mg/kg once daily [dose can be split and given every 12 hours]) was initiated (see Treatment at a Glance).1-3
Trooper was rechecked 1 month after zinc therapy was initiated; lesions showed some improvement, and evaluation of an impression smear confirmed the absence of bacteria. Low-dose methylprednisolone (initial dose, 0.7 mg/kg once daily) was initiated and tapered over 1 month. In many cases, low-dose corticosteroids can be beneficial for treatment of dogs that do not respond to zinc alone,4 as corticosteroids are known to increase zinc absorption from the GI tract.
TREATMENT AT A GLANCE
Cytologic impression smears should be performed and any secondary infections (eg, Malassezia pachydermatis, bacteria) treated.
Zinc-responsive dermatosis syndrome I should be treated through long-term supplementation with zinc sulfate, zinc gluconate, or zinc methionine, and doses should be based on elemental zinc (initial dose, 2-3 mg/kg once daily or split and given every 12 hours). Zinc sulfate may have lower bioavailability and can cause gastric irritation.
Supplemental therapies (eg, omega fatty acids, corticosteroids, antibacterial topical medications) may be helpful and can be used as warranted.6
Prognosis & Outcome
Trooper was presented 6 weeks later for a recheck examination. He had not received methylprednisolone for 2 weeks, and all lesions were resolved. Zinc methionine supplementation was continued, and Trooper was free of lesions. Lifelong zinc supplementation is typically needed. Long-term prognosis is favorable as long as zinc supplementation is maintained.
Discussion
Zinc-responsive dermatosis syndrome I is a condition that occurs primarily in Alaskan malamutes, Siberian huskies, and other arctic breeds and may be associated with defective intestinal absorption of zinc.1,2,5
Syndrome II occurs in dogs fed a zinc-deficient diet.1,2,6 The author has anecdotally seen an increase in the number of syndrome II cases that may be a result of an increase in dogs being fed home-prepared and alternative diets. Lesions are typically located at mucocutaneous junctions and paw pads and appear as areas of erythema with scaling, crusts, and hyperkeratosis.
The discussion continues on Clinician's Brief: The Podcast
Hear the author lay out the specialist’s perspective on initial work-up and eventual diagnosis in this episode of Clinician's Brief: The Podcast. Plus, Dr. Rosenberg covers the bread-and-butter clinical tools of veterinary dermatologists and shares his insights on how telehealth translates to dermatology.
Zinc-responsive dermatosis should be on the differential diagnosis list for crusted skin disease in any northern- or arctic-breed dog (see Take-Home Messages). Diagnosis is made through history and biopsy. Serum or hair levels of zinc may be low in affected patients; however, proper analysis can be difficult due to a variety of factors, so biopsy is the recommended diagnostic test if zinc-responsive dermatosis is suspected.7
TAKE-HOME MESSAGES
There are 2 types of zinc-responsive dermatosis: syndrome I, which affects arctic breeds (most frequently Siberian huskies and Alaskan malamutes) and appears to be associated with abnormal intestinal absorption of zinc, and syndrome II, which may affect dogs fed a zinc-deficient diet.
Diagnosis is made via history and biopsy.
Syndrome I should be treated with zinc supplementation. Doses should be based on elemental zinc (initial dose, 2-3 mg/kg once daily or split and given every 12 hours).
Corticosteroids can be helpful for dogs with syndrome I that do not respond to zinc supplementation alone.4 Omega fatty acids may also be helpful.
Once identified and treated, the prognosis for both syndromes is typically favorable.