Negative Pressure Wound Therapy for Complicated Elbow Hygroma
Shaylan Meyer, University of Minnesota
Stan Veytsman, DVM, VCA Palm Beach Veterinary Specialists, West Palm Beach, Florida
Shiori Arai, DVM, MS, DACVS (Small Animal), University of Minnesota

A hygroma is a nonepithelial-lined cavity or sac filled with serous fluid surrounded by a dense wall of fibrous tissue that develops over a bony prominence.1 Serous fluid is not absorbed during hygroma development, and previously formed skin callus fails to protect the underlying tissue as inflammation increases; a fibrous capsule can form in an attempt to wall off the area.2,3
This condition is commonly seen in large- and giant-breed dogs (eg, German shepherd dogs, Great Danes, mastiffs, Saint Bernards, Newfoundlands, Irish wolfhounds) that are 6 to 18 months of age.4-7 Hygromas can occur over any bony prominence (eg, greater trochanter, ischiatic tuberosity) but most commonly occur over the olecranon of the elbow.2,3,8
Elbow hygromas can be classified as uncomplicated or complicated based on clinical appearance.9 Uncomplicated elbow hygromas are small, painless, and nonulcerated and can progress in severity as trauma occurs and continues, resulting in cellular death, ischemia, and edema. Complicated elbow hygromas are typically recurrent, large, painful, ulcerated, and/or infected.6 Calcinosis cutis circumscripta-type lesions appearing secondary to chronic hygromas have also been described.10 Other classification schemes for elbow hygromas based on the mechanisms of development have been reported.5
Treatment & Management
Conservative Management
Conservative management of uncomplicated elbow hygromas aims for resolution in 2 to 3 weeks; fibrous connective tissue can develop during this healing process.3,4 Aspiration of the hygroma fluid may be attempted using an aseptic technique, but recurrence and infection are common sequelae.3,4 Intralesional corticosteroid administration is not recommended because of the risk for acute infection following injection.8 Conservative management includes educating pet owners about at-risk breeds and emphasizing the importance of maintaining the patient’s ideal body weight, protecting elbows from hard surfaces using soft bedding, and maintaining loose padding of the elbows, especially in early stage of elbow hygroma development.1,4 Although neoprene/polyester-padded elbow sleeves are commercially available, their clinical efficacy has not been evaluated.
Surgical Correction
Surgical correction should be reserved for complicated elbow hygromas and can include:
Passive or active drainage of cavitated lesions with external coaptation6
Releasing incisions or using tension-relieving closing techniques2,3,11
Ostectomy of the olecranon to decrease pressure on the overlying skin3
Reconstruction after excision of the hygroma using single pedicle advancement flaps, single pedicle direct flaps, and axial pattern flaps (eg, superficial brachial artery, thoracodorsal artery, or rectus abdominis free muscle flaps)3,12
The microvascular free muscle transfer technique7
Surgical repair with commercially available foam pipe insulation for the protection of elbows13
Surgical debridement and vacuum-assisted closure with application of negative pressure wound therapy (NPWT)14
Postoperative external coaptation with soft padded bandaging or splinting is commonly used to immobilize the elbow joint, regardless of surgical technique. NPWT has been used in wound management in small animal patients and can be useful for large unhealthy wound beds.15 NPWT aids in closing wounds through development of healthy granulation tissue, which enables later primary wound closure. NPWT has been shown to improve the wound healing process, decrease the frequency of bandage changes, and decrease the risk for contamination. Limitations include equipment, labor costs, and the need to train staff members, including clinicians.
Complications reported with surgical correction of elbow hygromas include skin dehiscence associated with tension, surgical site infection, splint- and bandage-related lesions, seroma formation, pain, delayed healing, and, with NPWT, loss of the periwound seal.4,8,14
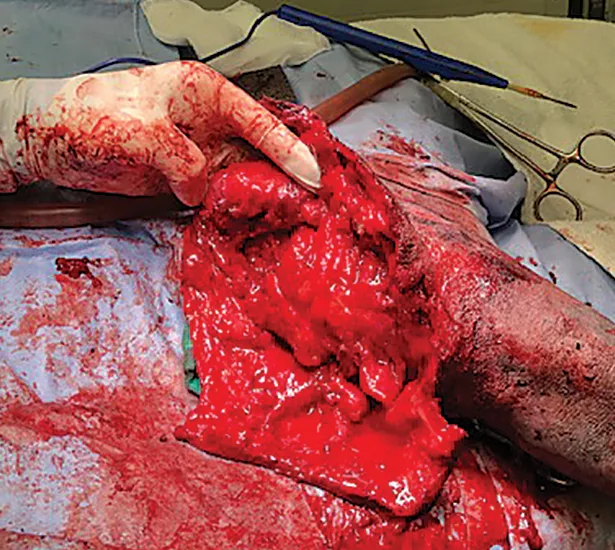
Orthogonal elbow radiography is recommended prior to surgery to rule out osteomyelitis, periostitis, and neoplasia as possible causes of hygroma formation.3 Sedation may be required for tissue biopsy and deep cultures prior to surgery if the hygroma is complicated and ulcerated (Figure 1).

Complicated right elbow hygroma in a 2-year-old neutered male Great Dane
Clinical Monitoring & Follow-Up
Postoperatively, the patient should be hospitalized for 3 to 4 days and monitored at least every 2 hours for fluid production and to ensure consistent negative pressure. Alternatively, the patient can be discharged with the unit for at-home monitoring (Figure 2). Owners should be educated about the unit so they can troubleshoot if necessary and be provided with multiple canisters so they can change the canister as it fills.
NPWT can be discontinued 3 to 4 days postoperatively with the patient under general anesthesia (Figure 3). The resultant wound bed may have evidence of stimulated and evenly distributed granulation tissues, allowing for delayed primary closure with interrupted and tension-relieving (near-far-far-near pattern) skin sutures (3-0 nylon).
External coaptation should be performed for an additional 10 to 14 days until the incision heals (Figure 4). Bandages should be changed every 3 to 5 days to assess the wound for complications. As an alternative to external coaptation, foam insulation can be applied to protect the elbow.13 Once the surgical site heals, the owner should be advised of the necessary lifelong changes to care, including providing soft bedding, padding the elbows if erythema is observed (usually the first sign of pressure sores), and maintaining an ideal body condition.

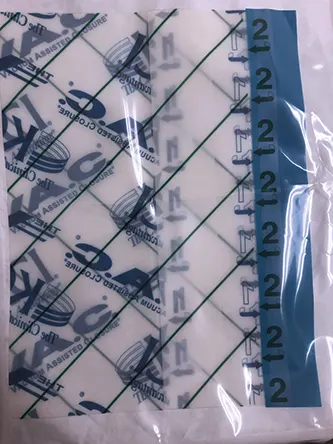
FIGURE 2
An NPWT unit for at-home monitoring of a patient following elbow hygroma removal
STEP-BY-STEP
Negative Pressure Wound Therapy for Complicated Elbow Hygroma
WHAT YOU WILL NEED
Standard surgical pack with #10 or #15 scalpel blades
Sterile isotonic saline
Monopolar electrocautery or Mayo or Metzenbaum scissors
Polyurethane ether foam dressing and vacuum pad
Vacuum-assisted closure system, including canisters with attached tubing
Semipermeable adhesive drapes
Antimicrobial incise drapes or transparent film dressing
Medical adhesive spray or stoma paste
Nylon suture (3-0)
Bandaging material and tape
STEP 1
Clip the affected thoracic limb from mid-dorsum of the cervical region distally to the digits. Position the patient in lateral recumbency with the affected limb isolated and the lateral side exposed. Aseptically prepare the limb while it is hung from the ceiling or other device. Perform standard draping.

STEP 2
Administer perioperative IV antimicrobials (eg, cefazolin) 30 minutes prior to making an incision; re-administer every 90 minutes. Make a proximal-to-distal incision using a #10 or #15 scalpel blade over the wound, incorporating the open ulcerated wounds. Carefully dissect the SC and/or necrotic tissue directly and sharply with monopolar electrocautery or Mayo or Metzenbaum scissors. Simultaneously perform surgical debridement of any necrotic tissue.
Author Insight
Avoid incising over the olecranon region, as a pressure point will form when the incision is closed, increasing the risk for dehiscence. When trimming, preserve as much skin and cutaneous callus as possible for closure.
STEP 3
Copiously lavage the wound site with warm sterile isotonic saline prior to closure. Obtain a tissue sample for bacterial culture and susceptibility testing if needed.

STEP 4
Apply foam dressing to the wound bed; avoid overlapping skin to prevent skin maceration and damage. Apply adhesive spray or stoma paste 3 to 5 cm around the periwound skin as needed. Next, apply a semipermeable adhesive drape to the entire wound bed, covering the skin and foam. Using a #10 scalpel blade, make a 2-cm slit through the drape over the foam, remove the protective covering from the vacuum pad, and attach the vacuum pad to the slit area. Direct the tubing toward the dorsum, not distally. Cover the pad with another layer of semipermeable adhesive draping.
Author Insight
Antimicrobial incision drapes or transparent film dressing can be used if there is limited availability of semipermeable adhesive drapes.
STEP 5
Attach the suction tubing to the collection canister and initiate the pump unit. Maintain pressure at -125 mm Hg.13 After the pump is activated, confirm successful dressing placement through visualization of shriveling, hardening, and wrinkling of the foam and drapes.14