Metastatic Carcinoma in a Mandibular Lymph Node of a Dog
Maria Bell, DVM, Kansas State University
Lisa M. Pohlman, DVM, MS, DACVP, Kansas State University

Fine-needle aspiration of a mandibular lymph node from a dog. Photo courtesy of Dr. Dudley McCaw
Lymph node fine-needle aspiration with cytology is a noninvasive, low-cost method for staging cancer in canine and feline patients. Carcinomas are commonly diagnosed in dogs and cats, and these neoplasms frequently metastasize to lymph nodes.
Epithelial cells are not present in the lymph nodes of healthy patients. Therefore, identification of epithelial cells within a lymph node is significant and typically indicative of metastatic disease (assuming the cells have been correctly identified and the sample was obtained appropriately).1
In the author’s experience, it is relatively common for the initial diagnosis of malignant neoplasia to be generated from the identification of abnormal cells in the lymph node aspirate. This finding initiates the search for a primary mass if one has not already been identified. Additionally, identification of malignant neoplasia in a lymph node is extremely valuable when a primary lesion has been identified via imaging but a sample is not easily obtainable without anesthesia or more invasive sampling techniques. The following case illustrates the value of lymph node cytology for the diagnosis of malignancy when the primary tumor is not easily accessible.
History
An 11-year-old intact female pug was presented for evaluation of epistaxis, sneezing, dyspnea, and swelling above both eyes. Brief improvement was noted after administration of clindamycin and corticosteroids, but clinical signs worsened and the dog was referred to Kansas State University Veterinary Health Center. On presentation, the owners reported that they had noticed significant exercise intolerance and an increase in respiratory effort. They also said that the dog was unable to sleep for more than a few seconds at a time.
Examination
Physical examination revealed increased body temperature (103.5°F [39.7°C]; normal range, 100.5-102.5°F), stenotic nares, and referred upper airway noise on auscultation. Firm swelling was noted above the left orbit, and anisocoria was evident, with a slightly larger left pupil. Mucous membranes were pink; capillary refill time was <2 seconds. BCS was 4/5. Gingivitis and gingival hyperplasia were also noted.
Moderate left mandibular lymphadenopathy was identified on palpation, so a fine-needle aspirate of the node was obtained and submitted for cytologic evaluation.
Computed tomography of the skull showed a mass lesion that was causing severe bony lysis of the maxilla, frontal sinuses, nasal turbinates, and cribriform plate, consistent with neoplasia (Figure 1).
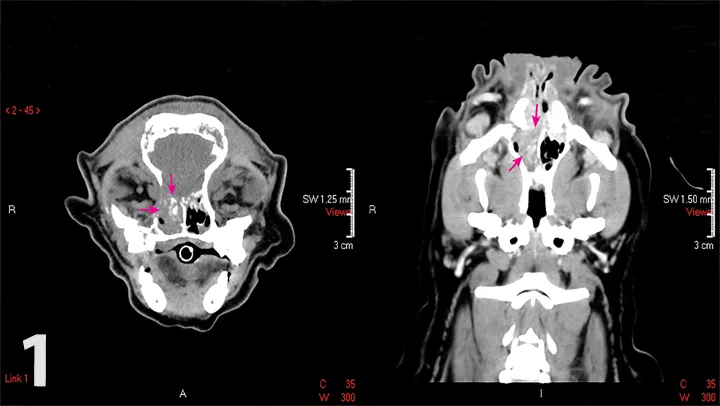
Computed tomography scans of the patient’s skull. Note the mass (arrows) in the right nasal passage. Image courtesy of Dr. Paxton Harness
Cytologic Findings
Cytology revealed predominantly small lymphocytes containing mature chromatin and fewer but mildly increased medium and large lymphocytes and plasma cells. Scattered among the lymphoid population were a few large, round-to-polygonal cells arranged in cohesive sheets and occasionally seen individually. These cells exhibited moderate anisocytosis, anisokaryosis, and anisonucleoliosis. Each had a round-to-oval nucleus with a finely stippled chromatin pattern and as many as 8 prominent nucleoli. Neutrophils were mildly increased in number. The background contained scattered mast cells, macrophages, red blood cells, and lymphoglandular bodies (cytoplasmic fragments; Figure 2).
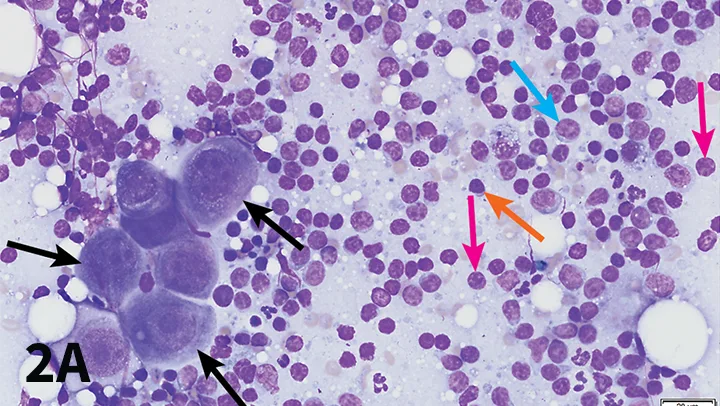
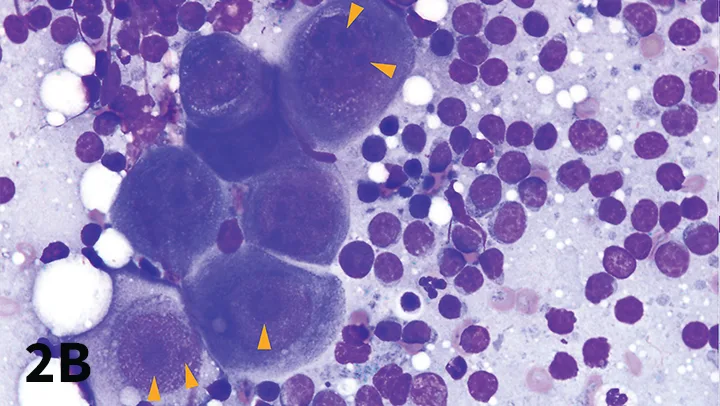
(A) Fine-needle aspiration cytology of the left mandibular lymph node. Note the cluster of large, cohesive cells (black arrows). These cells exhibit anisocytosis, anisokaryosis, and anisonucleoliosis and should not normally be present in lymph nodes. Also visible are numerous intact lymphocytes, including small lymphocytes (orange arrow), medium lymphocytes (blue arrow), rare large lymphocytes (arrowhead); scattered neutrophils; and macrophages. Naked nuclei (pink arrows) of ruptured cells are also seen and should not be confused with intact cells. (Modified Wright’s stain, magnification 600×) (B) Higher-magnification image of a cluster of metastatic epithelial cells. Note the anisonucleoliosis (variably sized nucleoli both within single cells and among different cells; arrowheads). (Modified Wright’s stain, original magnification 1000×)
When examining cytology images, it is important to recognize that metastatic epithelial cells have a very different appearance than lymphoid cells. The epithelial cells are much larger than the lymphoid cells, have significantly more cytoplasm, and are grouped cohesively.
Diagnosis
Cytologic findings were consistent with metastatic carcinoma with concurrent mild reactive lymphoid hyperplasia and mild neutrophilic lymphadenitis. Given the imaging findings, a primary nasal carcinoma was presumed.
Clinical Outcome
Treatment options for metastatic carcinoma include radiation, chemotherapy, or palliative treatment with piroxicam.2 Studies indicate that patients that undergo radiation therapy have an average survival time of ≈6 months.2 Radiation therapy was declined in this case because of the degree of tumor invasion and the high likelihood of side effects and/or complications. Chemotherapy was not advised, as it was unlikely to stop or slow progression of a tumor of this magnitude. The owners elected a treatment plan of piroxicam, mirtazapine, codeine, and Yunnan Baiyao. The patient died at home several weeks after diagnosis.
Summary
Lymph node fine-needle aspiration with cytology is commonly used for evaluating patients for metastatic disease after a diagnosis of malignant neoplasia. In some cases, however, the primary lesion is not easily accessible or a sample cannot be obtained without anesthesia (which may be contraindicated in a critical patient or cost-prohibitive for the owners). Lymph node cytology may provide a diagnosis. In this case, the primary tumor had metastasized to an accessible peripheral lymph node and a diagnosis of carcinoma was reached without more invasive sampling.