Lower Urinary Tract Infections: From Diagnosis to Treatment
Patricia Dowling, DVM, MSc, DACVIM (Large Animal), DACVCP, Western College of Veterinary Medicine, Saskatoon, Saskatchewan, Canada
Bacterial UTIs are commonly diagnosed in dogs and cats. Although bacterial cystitis occurs in male and female dogs of all ages, in cats, it is more common in spayed females and cats >10 years of age. Antimicrobial agents used to treat UTIs have not changed, but there are increasing concerns over rising rates of antimicrobial resistance. Good antimicrobial stewardship is needed; thus, there are new recommendations regarding which types of bacteriuria require antimicrobial treatment, which antimicrobials should be considered first-line, and duration of antimicrobial treatment.1
Diagnosis
Accurately diagnosing infection that requires treatment should be considered first. A complete urinalysis is warranted for dogs and cats presented with clinical signs of UTI. Indications to perform urine culture and susceptibility testing include history (eg, sporadic or recurrent infection), clinical signs (eg, dysuria, hematuria, pollakiuria, stranguria), visualization of bacteria during urine sediment examination, and evidence of pyuria.1
Because UTIs predominantly occur in senior cats, typically those with comorbidities, urine culture and susceptibility testing is recommended, even with initial diagnosis; however, reports from several veterinary hospitals show poor concordance of appropriate diagnosis and antimicrobial use for canine and feline UTIs.2,3 In a recent unpublished study by the author, ≈40% of in-clinic diagnoses of bacterial UTIs in dogs were not confirmed by urinalysis, and culture and susceptibility testing was not performed by an accredited veterinary diagnostic laboratory. Although underuse of diagnostic laboratory services can be a result of many factors (eg, cost and time delay between sampling and results), administering antimicrobials to patients without an infection that requires antimicrobial therapy is a serious misuse of these drugs.
Types of UTIs
Once an accurate diagnosis of UTI has been made, the type of UTI should be considered before an antimicrobial treatment regimen is selected.
Sporadic Bacterial Cystitis
Sporadic bacterial cystitis (SBC; also known as simple UTI) is caused by a temporary break in host defenses. Patients are typically presented with compatible lower urinary tract signs and respond quickly to appropriate therapy; clinical signs do not readily recur. Because most antimicrobials achieve high concentrations in urine, most cases of SBC are one-time infections that respond well to appropriate first-line therapy (Table). If the diagnosis of infection is accurate, treatment for SBC in dogs may be empiric and based on knowledge of the commonly isolated pathogens and their typical susceptibility to antimicrobials.1 This is not true for young to middle-aged cats, as those with clinical signs of lower urinary tract disease are unlikely to have SBC and more likely to have feline lower urinary tract disease/feline urological syndrome.
When choosing an antimicrobial, the pharmacokinetics and pharmacodynamics of the drug, potential adverse effects (for both patient and pet owner), ease of administration, and cost should be considered.
Urine concentrations of antimicrobials are more important than serum concentrations during treatment of sporadic UTIs. Urine concentrations generally exceed serum concentrations, as most antimicrobials are excreted in an active form in the urine. If the urine concentration is ≥4 times than the minimum inhibitory concentration for the duration of the dosage interval, it will most likely be effective (90%) for treatment of UTIs caused by that pathogen4; therefore, despite a susceptibility test result of resistant for amoxicillin for first-time SBC caused by Escherichia coli or Staphylococcus pseudintermedius in dogs or cats, extremely high urine concentrations make amoxicillin the first choice for therapy, and initial or empiric treatment with amoxicillin/clavulanic acid is not recommended.1-3
Because the clinical signs of SBC are related to inflammation, treatment with NSAIDs can be considered (caution is advised in cats), and antimicrobials can be started only if clinical signs persist or increase in severity. New recommendations are to administer antimicrobial therapy for only 3 to 5 days, despite label directions for longer treatment durations. If clinical signs resolve after short-term treatment, there is no need for additional urinalysis or urine culture.1
Antimicrobial Treatment Options for UTI*
*Treatment options are listed in order of preference according to antimicrobial stewardship principles.1
Recurrent Bacterial Cystitis
Recurrent bacterial cystitis is due to a persistent underlying abnormality in the urinary tract or host defenses that results in ≥3 episodes of UTIs in the preceding 12 months or ≥2 episodes in the preceding 6 months.1 The underlying cause may or may not be effectively managed depending on its pathophysiology, but long-term repeated antimicrobial therapy is unlikely to be effective. Reinfection occurs when the patient is infected with a new bacterial species or strain after successful therapy documented by negative urine culture posttreatment. Advanced diagnostics should be considered to identify treatable predispositions, and UTI should be treated according to the recommendations for SBC; long-term therapy is no longer recommended.
Relapse occurs when the original infection is not cleared despite therapy. Relapses can occur secondary to pathology (eg, biofilms, urolithiasis, pyelonephritis) that prevents appropriate antimicrobial therapy from reaching the infection site in an effective concentration. E coli is the most frequently isolated bacteria that causes UTIs in dogs and cats.5-8
Relapses from E coli infection may occur due to unique virulence factors that allow E coli of enteric origin to invade the uroepithelium via a pathogenic cycle and evade adequate urine concentrations of antimicrobials (Figure).9,10 A uropathogenic E coli (UPEC) infection should be suspected when E coli is repeatedly cultured, especially if the susceptibility pattern remains consistent. For patients with relapsing UTIs, it is important to ensure that adequate antimicrobial concentrations are achieved in the urine and bladder to clear the infection. Antimicrobial choice, dosage regimen, susceptibility pattern, and owner compliance should be reviewed, as few drugs effectively treat intracellular or biofilm infections,11 and a high rate of antimicrobial resistance has been documented in dogs with UPEC.10,12
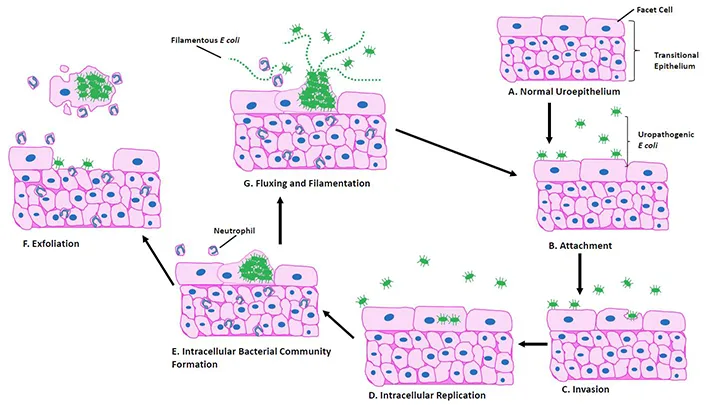
Pathogenesis of UPEC infections. The bladder uroepithelium is a pseudostratified transitional epithelium lined by large facet cells (A). UPEC that reach the bladder adhere to the surface of the facet cell via pili (B). Once attached, UPEC are able to invade (C) and replicate (D) in the cytoplasm of the facet cells. They then form intracellular bacterial communities (E) protected from antimicrobials that do not achieve adequate intracellular concentrations. The host’s immune response recruits neutrophils, and infected cells may be sloughed and excreted in the urine to contaminate the environment, resulting in spread to new hosts (F). Alternatively, bacteria from the intracellular bacterial community may develop a filamentous morphology and emerge in the bladder lumen to adhere to other facet cells (G) and restart the infection cycle.
Subclinical Bacteriuria
Subclinical bacteriuria is not uncommon in otherwise healthy patients, patients with comorbidities (eg, diabetes mellitus, chronic kidney disease), or those being treated with immunosuppressive drugs. Despite concerns over possible secondary complications (eg, sepsis, pyelonephritis) there is little evidence that subclinical bacteriuria increases the risk for clinical UTIs or other infectious complications in dogs or cats.13,14 Subclinical bacteriuria is not typically treated in human medicine, even in immunocompromised patients.1 Treatment may result in short-term elimination of the bacteriuria, but recolonization is common and associated with increasing antimicrobial resistance; therefore, if bacteria are seen on urinalysis but the dog or cat shows no clinical signs of UTI, it is now recommended that culture and susceptibility testing should not be performed and the patient should not be treated with antimicrobials.1 Even isolation of a multidrug-resistant pathogen does not necessarily indicate the need for treatment. Clinical judgment should be used on whether to treat patients without clinical signs of UTI (eg, due to a spinal cord injury, being immunosuppressed).
Treatment
Amoxicillin administered for 3 to 5 days is the first-choice treatment (Table) for patients with SBC.1 If clinical signs resolve, no further diagnostics or treatments are necessary. Reinfections should be treated as for SBC, with emphasis on identifying underlying abnormalities. Relapses may be due to complicated pathology, with UPEC and biofilms requiring special considerations for therapy. Patients with subclinical bacteriuria should not be routinely treated with antimicrobial agents, even if comorbidities are present.
Conclusion
Antimicrobial stewardship for UTIs in dogs and cats requires accurate diagnosis followed by determination of the type of infection and an appropriate antimicrobial regimen.
Editor’s note: This article was originally published in February 2022 as “Lower Urinary Tract Infections.”