Loss of Balance in a Geriatric Dog: A Diagnostic Dilemma
C. Elizabeth Boudreau, DVM, PhD, DACVIM (Neurology), Texas A&M University College of Veterinary Medicine and Biomedical Sciences

Marty, a 13-year-old castrated Yorkshire terrier, developed a persistent right head tilt and was unable to stand during a routine veterinary visit.
History
After a week of lethargy and hyporexia, Marty was diagnosed with tapeworms and administered praziquantel during a primary care veterinary visit. Shortly after the medication was given, he became acutely unable to stand and developed a persistent right head tilt. There was no known history of trauma, and the owners had not noted any other abnormalities before the visit.
Physical Examination
Marty was referred to the local teaching hospital through its emergency receiving service. At presentation, the dog was anxious. Truncal alopecia and seborrhea were the only abnormalities on general examination. Neurologic examination showed that he was nonambulatory but had good voluntary movement in all limbs and decreased proprioceptive placing in both pelvic limbs. He continued to tilt his head to the right. Cranial nerve (CN) assessment identified spontaneous right rotatory nystagmus in all postures. Because of the extreme nature of the right head tilt, it was difficult to discern if there was also a right head turn present.
No other neurologic abnormalities were noted. Fundic and otoscopic examination showed no abnormalities.
Ask Yourself
What neurologic examination findings help differentiate central from peripheral vestibular disease?
What are the major differentials for acute-onset vestibular disease in geriatric dogs?
What prognostic and therapeutic features do the top 2 differentials have in common?
Why is definitive diagnosis of the cause of acute-onset vestibular disease in a geriatric dog important?
Diagnostic Results
Blood pressure by Doppler was within normal limits. A CBC showed a mild mature neutrophilia, and a serum chemistry panel showed moderate elevations in ALP and ALT. All other values were within reference ranges for the laboratory. Mild heptomegaly was noted on plain abdominal radiographs; thoracic radiographs were within normal limits.
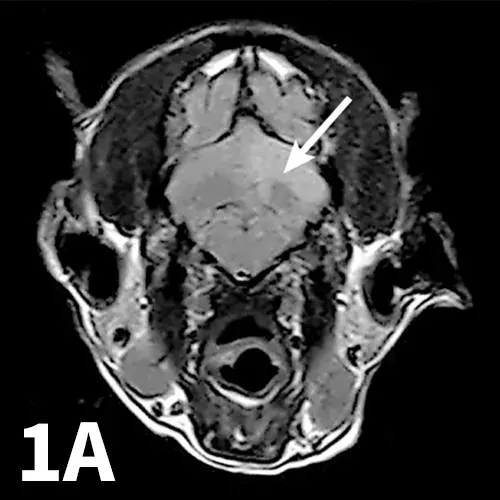
T2-weighted fluid-attenuated inversion recovery (FLAIR) transverse image showing well-demarcated hyperintensity (arrow) without apparent mass effect in the left cerebellar hemisphere (A). Apparent diffusion coefficient (ADC) map showing a coincident area of restricted diffusion (B; arrowhead).
Marty was hospitalized for monitoring and treatment for vestibular disease of unknown cause. Meclizine (4 mg/kg PO once a day) and maropitant (1 mg/kg SC once a day) were used to manage presumed vestibular dysfunction-associated nausea. After 48 hours, no improvement was seen, and further diagnostic testing was recommended.
The patient was anesthetized and magnetic resonance imaging (MRI) of the brain was performed. MRI showed a well-demarcated T2-weighted hyperintensity without mass effect in the left cerebellar hemisphere. This area was noncontrast enhancing and showed evidence of restricted diffusion on diffusion-weighted imaging (Figure 1). A cisternal cerebrospinal fluid tap was performed; results were within normal limits. These findings are most consistent with an ischemic event associated with the left rostral cerebellar artery. 1,2
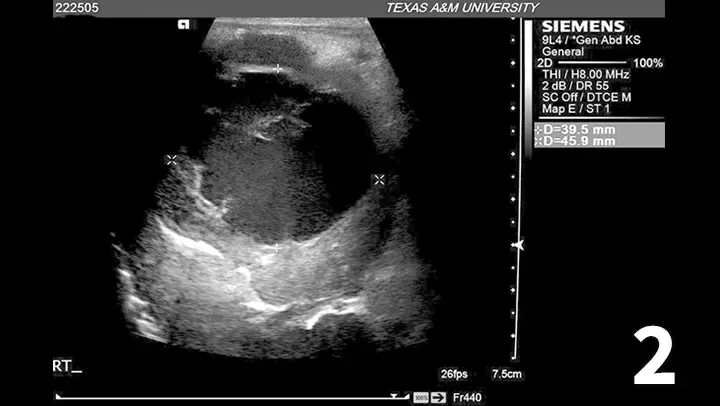
Cavitary region within mass in the right liver lobe, composed of mixed highly echogenic and hypoechoic fluid and a few small, hyperechoic septae. The cavitation measures ~4.0 x 4.5 cm between the ‘x’ symbols.
An abdominal ultrasound was also pursued to investigate possible sources of thromboembolic disease and to further evaluate the hepatomegaly identified on abdominal radiographs. A 4-5–cm diameter, ill-defined mass with poor intraparenchymal blood flow and a large cavitary region was identified in the right liver lobe (Figure 2).
Did You Answer?
Both central and peripheral vestibular disease are likely to have cardinal signs of vestibular dysfunction, including head tilt, loss of balance, asymmetrical ataxia and extensor tone, and abnormalities of eye position and movement (ie, induced ventrolateral strabismus, spontaneous nystagmus). Central vestibular disease may also be associated with changes in mentation, abnormal body posture (eg, head turn, proprioceptive deficits, paresis). Dogs with severe vestibular disease, either central or peripheral, may be difficult to assess for some of these more subtle findings. Also although finding these abnormalities strongly suggests a central vestibular problem, their absence does not rule one out (Table 1).
One of the most common causes of acute-onset peripheral vestibular disease in geriatric dogs is idiopathic, which is a diagnosis of exclusion. Other relatively common causes include extension of middle ear disease to the inner ear or toxic effects of topical medications applied to the ear canal. Hypothyroidism has been reported in association with acute-onset peripheral or central vestibular disease,3 but the pathophysiology is unknown. One of the most common causes of acute-onset central vestibular disease in geriatric dogs is a vascular accident, as the rostral medulla and cerebellum seem prone to infarction of the rostral cerebellar artery.4
Neoplasia and toxic effects of medication (most notably metronidazole) are also relatively likely. Primary inflammatory diseases such as granulomatous meningoencephalomyelitis (GME) typically affect younger adults, and nutritional deficiency (ie, thiamine deficiency) is rarely diagnosed in dogs (Table 2).
In cases where a peripheral vs central localization for vestibular signs is difficult to determine, the 2 most likely differentials may be idiopathic geriatric vestibular disease of dogs and a vascular accident. These would be expected to have peracute onset, be static to improving with no specific treatment, and be unlikely to recur (though recurrence is possible with both).
Definitive diagnosis through advanced imaging is helpful to rule out less likely causes of peracute-onset vestibular disease that would require specific treat-ment (eg, progression of middle ear disease, meningitis or encephalitis, neoplastic processes, metabolic or toxic causes). In cases of vascular injury, MRI diagnosis may alert clinicians that systemic diagnostics to identify possible predisposing causes for infarction are indicated. In dogs, it is thought that more than half of patients with an MRI diagnosis of intracranial infarct have a concurrent medical condition that could predispose to thromboembolic events.5
Although most patients with central nervous infarcts improve over time, identification of predisposing factors may help reduce the risk for recurrence and benefit overall health.
TABLE 1. Neurologic Examination Findings in Vestibular Disease
TABLE 2. Common Differentials for Acute-Onset Vestibular Disease*
*In older dogs, in the absence of a history of trauma
Diagnosis
Vestibular disease
Treatment
Following completion of diagnostics, Marty remained hospitalized on maintenance fluids. Meclizine and maropitant were continued, and omeprazole was added at 1 mg/kg PO once a day. Clopidogrel (3.75 mg/kg once a day) was initiated to reduce the risk for future thromboembolic events. Unfortunately, Marty showed no neurologic improvement over the next 5 days, and owners elected euthanasia.