Locoregional Anesthesia Complications
Katherine Bennett, DVM, DACVAA, Veterinary Specialty Center, Buffalo Grove, Illinois
Locoregional anesthesia is a critical part of balanced anesthesia. Local blocks, which are a type of locoregional anesthesia, can provide perioperative pain management that exceeds the duration of the procedure and reduces the minimum alveolar concentration of inhalant anesthetics by ≤50%.1,2 Locoregional anesthesia can be as simple as a splash block on a surgical site or as advanced as ultrasound-guided deposition of local anesthetic into a fascial plane. Knowledge of pharmacology, safe and standardized techniques, and careful patient monitoring can help mitigate risks for complications.1,3
Local anesthetics are ion channel blockers that act mainly on sodium channel receptors to block the generation and propagation of electrical impulses in nerves, inducing sensory and, potentially, motor blockade.1 Local anesthetic agents administered systemically or in the central neuroaxis (eg, epidural or intrathecal routes) also inhibit potassium and calcium channels in the dorsal horn of the spinal cord.1,4,5
Consideration of patient comorbidities (eg, clotting disorders, allergic reactions to local anesthetics) is basic standard of care when performing locoregional anesthesia.1,6,7 Attention should also be given to individual drug properties (eg, lipophilicity)1,3 and route of administration, which can affect both desirable and undesirable actions of local anesthetic drugs.
Infected tissue should not be punctured, despite the rare incidence of infections related to locoregional anesthesia. Careful attention to aseptic technique and evaluation of the area are recommended; block administration in areas with obvious skin infection (eg, crusts, pustules) or damage (eg, open wounds over the site of administration) is contraindicated.1,3,8,9 Risk for infection increases with repeated nerve blocks.3
Several risks and complications can be associated with locoregional anesthesia; systemic toxicosis, administration complications, and subsequent self-inflicted trauma are most common.
Systemic Toxicosis
Careful training and administration can help avoid toxicosis, which can be a dangerous risk associated with locoregional anesthesia. Different drugs have different dosages for toxicity. Cats are significantly more sensitive than dogs to the effects of local anesthetics (Table). Up to 7.5 of 10,000 humans receiving locoregional anesthesia experienced systemic toxicosis.6
High plasma concentrations of local anesthetics can cause both CNS and cardiac complications. CNS toxicosis usually occurs prior to cardiovascular toxicosis; initial clinical signs include agitation, sedation, and ataxia, which can progress to increased excitatory activity (eg, involuntary twitching), seizures, coma, respiratory arrest, cardiovascular depression, collapse, and possible death. Bupivacaine, a commonly used local anesthetic, blocks conduction between cardiac myocytes, preventing normal cardiac conduction and making bupivacaine the most cardiotoxic local anesthetic.1,10 Thus, if bupivacaine is inadvertently administered IV, cardiovascular collapse is expected prior to development of neurologic signs.
Development of CNS or cardiac toxicosis is highly reliant on the rate of drug absorption. For example, accidental IV administration of bupivacaine has a significantly faster onset of cardiovascular toxicity than an overdose via wound soaker catheter over 12 to 24 hours, yet both routes can induce systemic toxicosis.
Some local anesthetics (eg, lidocaine) are used as antiarrhythmics at low dosages, but higher dosages inhibit cardiac conduction via prolongation of phase 0 of the cardiac myocyte action potential and induce a prolonged refractory period. Arrhythmias, including ventricular tachycardias that evolve into ventricular fibrillation and cardiac arrest, are a common clinical sign of systemic toxicosis from local anesthetic agents. Extra caution is needed with bupivacaine because of cardiotoxicity; even rapid treatment is often unsuccessful if a large dose is administered IV.1,10 Accidental IV delivery can be prevented by aspirating the syringe to ensure the needle is not in a vessel prior to local anesthetic drug administration.
Treatment for local anesthetic toxicosis includes stopping administration of the drug, treating associated clinical signs, and administering IV lipid emulsion therapy (see Lipid Emulsion 20%).1,11 Patients that receive more than the recommended dose of a local anesthetic (Table) in a 24-hour period and/or are exhibiting clinical signs associated with toxicosis should be treated.
Lipid Emulsion 20%1
1.5 to 4 mL/kg IV over 1 minute, followed by 0.25 mL/kg/minute IV CRI for 30 to 60 minutes (CRI can be continued at 0.5 mL/kg/hour for up to 24 hours or until clinical signs improve.)
The author recommends IV lipid emulsion therapy and inotropes or antiarrhythmics (eg, phenylephrine: dogs, 0.5-3 µg/kg/minute; cats, 0.5-2 µg/kg/minute; dobutamine: cats and dogs, 5-15 µg/kg/minute; and/or amiodarone: dogs only, 0.5-0.8 mg/kg/hour, or esmolol: cats and dogs, 0.02-0.1 mg/kg/minute) for cardiac complications in cats and dogs, depending on the severity of the arrhythmia and concurrent blood pressure. Lipids help bind the local anesthetic agents, which are highly lipophilic.
Treatment for cardiovascular toxicosis depends on the drug administered. Lidocaine and mepivacaine toxicoses can be treated with positive inotropes (eg, dobutamine) and fluid support. Bupivacaine toxicosis is typically treated with amiodarone.1,8
Amiodarone is a class III antiarrhythmic that acts by blocking potassium, sodium, and calcium channels as well as beta-adrenergic receptors. Complications are possible, especially anaphylaxis, depending on the drug formulation. Amiodarone (dogs, 2 mg/kg IV bolus, then 0.8 mg/kg/hour for 6 hours, then 0.4 mg/kg/hour for 18 hours) should be administered slowly and carefully; blood pressure and heart rhythm (via ECG) should be monitored.12
IV lipid therapy can help resolve neurologic and cardiovascular toxicoses and is recommended along with monitoring and treatment for arrhythmias.2,10 Continued care, including continuous telemetry and neurologic status monitoring for at least 24 hours, is recommended.1,8
Maximum Recommended Dosages of Commonly Used Local Anesthetics1
Administration Complications
Complications of locoregional anesthesia include accidental IV administration of local blocks, hematoma formation or other tissue injury at the administration site, and nerve blockade failure.1,3,8,9
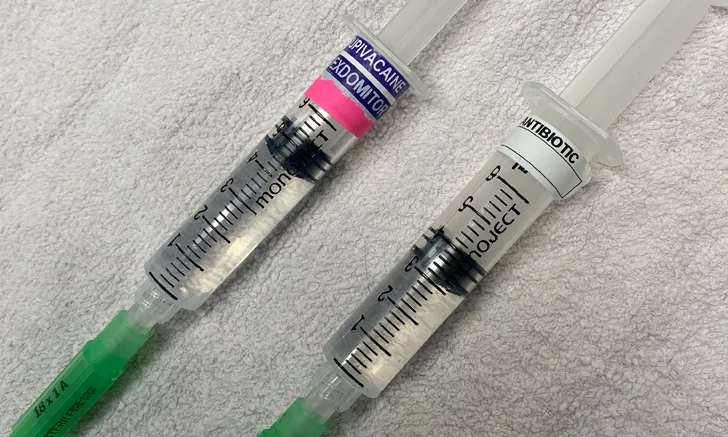
IV administration of bupivacaine can induce significant systemic toxicosis that can be fatal. Accidental administration is more likely when syringes are poorly labeled or not labeled in the perioperative period. Brightly colored labels or special syringe caps instead of a needle can be used (Figure). Waiting until right before administration to draw the solution can also help avoid accidental IV delivery. Blocks may be drawn for multiple patients in a clinic, so a conspicuous patient label on the syringe is recommended.
The incidence of complications associated with dental blocks in horses was <3% in a retrospective study.13 Complications included hematoma formation at the site of administration and failure to desensitize the desired nerve. Another retrospective study on equine dental blocks noted hematoma formation as the most common complication (3 of 270 cases); all cases resolved in 24 to 48 hours.5 A case report noted formation of retrobulbar hematoma following maxillary block in a dog that required immediate drainage to avoid damage to the eye.14
Hematoma formation following locoregional anesthesia does not always result in significant complications, but it can induce bruising that may be upsetting to the pet owner, significant swelling, and temporary disfigurement of the area that makes anatomic landmarks difficult to find. Hematoma formation also increases blood flow to the area, which can increase absorption of the local anesthetic and thus decrease the duration and efficacy of a nerve blockade.
Peripheral nerve injuries can occur when the nerve involved in a block is lacerated, stretched, or otherwise compromised due to poor technique. Most needles used in ultrasonography or nerve-stimulator–assisted techniques are designed with a rounded bevel and no bladed edges, making them less likely to cut or slice through nerve tissue. Although these needles are more expensive, they can help mitigate nerve or tissue damage.
It is important to note the pressure required when administering a block, as high resistance during injection may indicate the needle is in the nerve sheath; if this occurs, the needle should be redirected slightly and reassessed for lower resistance during administration.3,8
Blockade failure can occur with certain conditions (eg, inflammation or neoplasia at the blockade site), increased blood flow to the area being blocked (faster metabolism of the local anesthetic), or removal of the blockade (eg, flushing the abdomen after an intraperitoneal splash block). Timing, location, and clinician comfort level (eg, willingness to perform the block, willingness to use multiple attempts to achieve appropriate landmarks) should be considered when determining the cause of blockade failure.
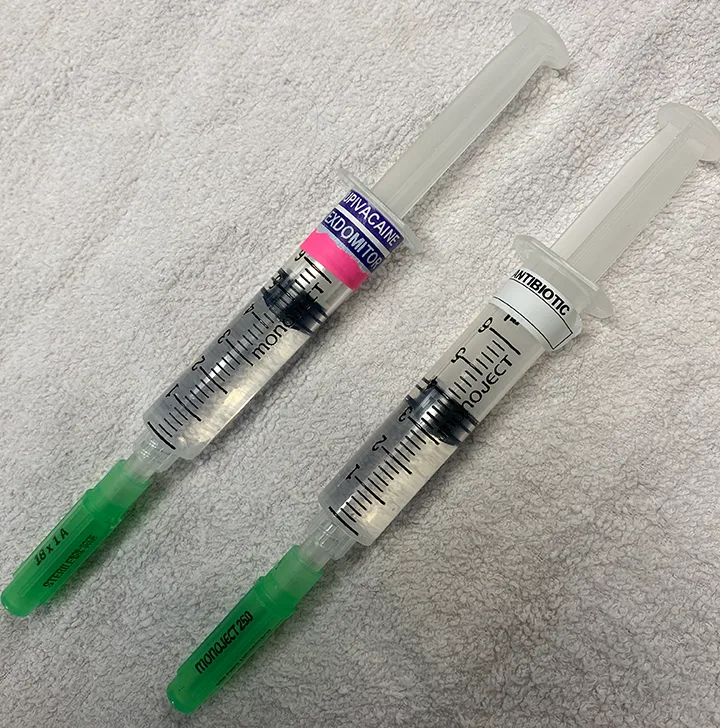
A common bupivacaine 0.5% dose for a 33-lb (15-kg) dog scheduled to receive a nerve block and perioperative antibiotics for stifle surgery would equal 4.5 mL (left), and a cefazolin 100 mg/mL dose would be 3.3 mL (right).8 These drug volumes are similar and could easily be mistaken. The local block syringe has a brightly colored label.
Subsequent Self-Inflicted Trauma
The most common sequela is patient trauma, which may be self-inflicted after block administration due to lack of sensation or lack of motor capabilities (eg, with epidural anesthesia). Complications are specific to the type of block; more information is available in the literature.
Self-trauma can occur if a patient is unable to feel a desensitized area of the body. For example, a bilateral mandibular blockade blocks the lingual nerve and, thus, sensory input to the tongue. Lingual mutilation has occurred in several species (eg, horses, dogs, cats) following dental block administration because of an inability to feel the tongue.1,2,8,9,13 Lingual trauma is more common when the tongue has both motor and sensory blockade, but a lack of pain sensation (ie, sensory blockade) alone can result in self-mutilation, especially if the patient is dysphoric in the immediate postoperative period. Other examples of self-trauma include tail mutilation after epidural administration, fractured pelvic limbs during recovery after epidural administration, and self-mutilation after onychectomy in cats. Careful observation and prevention (eg, no food or drink for 24 hours after oral surgery, Elizabethan collar or bandage placement, sling or harness support) of self-trauma behaviors are critical.1
Conclusion
Complications of locoregional anesthesia can be reduced with careful planning and proper technique. Appropriate medication and supportive care are paramount for patient survival. Locoregional anesthesia provides perioperative pain management without systemic effects and significantly reduces minimum alveolar concentration (≤50%) of inhalant anesthetics.1,2 Potential complications should not eliminate locoregional anesthesia from balanced anesthetic protocols.