Evaluation of thoracic limb lameness can be a challenge, in part because thorough assessment requires knowledge of common orthopedic abnormalities, understanding of relevant anatomy, and appropriate tools. Orthopedic examination should include gait, standing, and recumbent evaluations if the patient is compliant.
Gait Evaluation for Thoracic Limb Lameness
A long, nonslip, distraction-free area for gait evaluation, as well as assistance from a trained handler, can improve the likelihood of pain localization. Thoracic limb lameness is easiest to identify when watching a dog walk from the front or side.
Abnormal gait characteristics supportive of thoracic limb lameness include a head bob when weight is transferred to the lame leg, a head drop when weight is transferred to the sound leg, shorter stride length, and abnormal placement of the foot relative to the body (eg, placing the sound leg directly under the body and the lame leg more eccentrically [ie, away from midline]). Bilaterally affected dogs may shift weight onto the pelvic limbs without an obvious head bob or drop.
Lameness can be difficult to identify when intermittent, only apparent under certain circumstances, or absent at the clinic due to patient anxiety. Alternative methods for gait assessment include having the dog walk or trot in a circle or figure of 8 pattern, ascend and descend stairs, and navigate over obstacles. Pet owner recordings of lameness in the home can also help provide a more complete clinical picture.
Standing Evaluation for Thoracic Limb Lameness
Muscle atrophy, joint effusion, and standing joint angle should be evaluated. Both limbs can be palpated concurrently to evaluate symmetry. Because a cervical lesion can result in thoracic limb lameness, standing examination should also include a brief neurologic examination to evaluate the neck that may include assessment of proprioception, cervical range of motion, and cervical pain. A full description of canine neurologic examination is available in the literature (see Suggested Reading).
Recumbent Evaluation for Thoracic Limb Lameness
Recumbent examination allows for thorough palpation of the long bones and joints to further localize pain. The limbs are typically evaluated from distal to proximal because joints located more distally are easier to isolate. Long bones should be carefully palpated, and firm palpation of soft tissue should be avoided. The foot should also be carefully evaluated because abnormalities of the manus (eg, broken toenails, foreign bodies in the interdigital spaces or carpal pads) can be significant sources of pain.
Each joint should be evaluated for crepitus, range of motion, effusion, pain, and instability (CREPI). Joint effusion is often easier to feel during standing examination because weight-bearing pressurizes joint fluid toward the periphery of the joint but should also be evaluated during recumbency.
Evaluating the lame leg last can aid in patient compliance. Performing the examination in the exact same manner each time can help ensure no clinical abnormalities are missed.
Step-by-Step: Orthopedic Examination to Localize Thoracic Limb Lameness in a Dog
What You Will Need
Long, nonslip, well-lit walkway free of obstacles and distractions
Trained handler
Smartphone or other video recording device (optional)
Lift table (optional)
Step 1: Evaluate the Gait
Observe the dog for evidence of lameness and confirm the affected limb(s) as a trained handler walks and trots the dog back and forth and from side to side on a long, nonslip, distraction-free walkway. Ensure the handler leads the dog in a straight line at a constant speed and does not allow the dog to pull on the neck lead.
Author Insight
Recording the dog walking and/or trotting and watching the video in slow motion may help detect subtle signs of lameness.
Step 2: Evaluate the Natural Stance
Observe how the dog stands naturally. Subjectively assess weight-bearing by lifting each thoracic limb off the ground; the lame leg is often easier to lift compared with the contralateral limb.
Author Insight
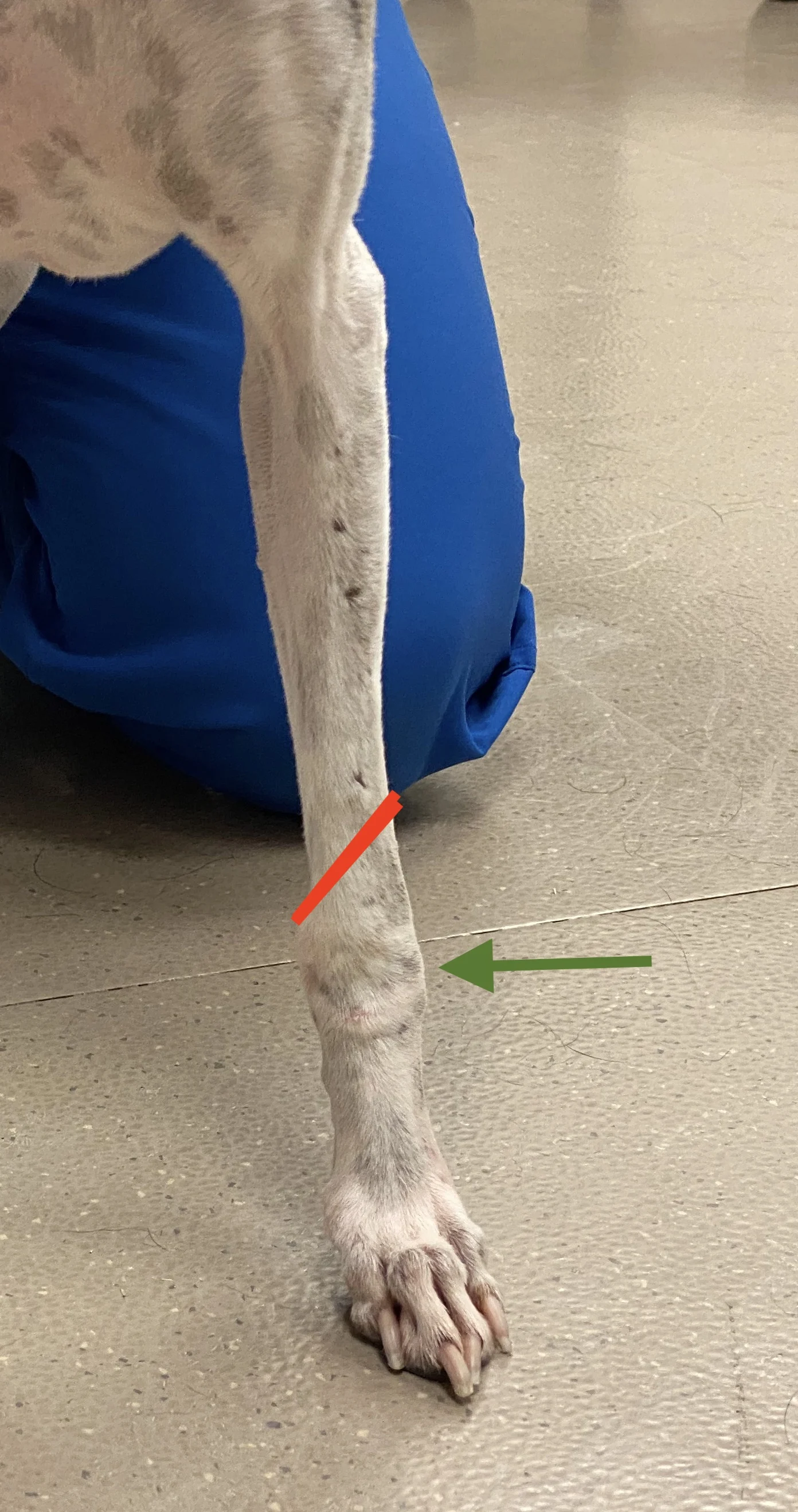
Dogs with thoracic limb lameness may place the lame limb eccentrically (ie, further from midline), have visible muscle atrophy (particularly over the lateral scapula), and have more of the metacarpal pad visible compared with the contralateral limb (Figure).

Step 3: Perform Gross Visual Evaluation of the Limb
Evaluate each joint for standing angle and position, as well as the overall limb for visible angular limb deformities (Figure) and obvious length discrepancies.

Step 4: Assess for Effusion, Thickening, & Pain
Visualize and palpate joints for effusion, thickening, and pain.
Author Insight
The shoulder is difficult to assess for effusion because of increased soft tissue coverage. Elbow effusion (A, arrow) is often easiest to see/palpate in the lateral joint compartment, which can be identified by palpating the space between the lateral epicondyle of the humerus and the olecranon (B).

A
Step 5: Palpate the Biceps Tendon
Palpate the biceps tendon medial to the greater tubercle in the intertubercular groove of the humerus.

Step 6: Position the Patient for Recumbent Examination
Place the patient in lateral recumbency.
Author Insight
A lift table should be used if possible because it can provide better ergonomics for the clinician and assistant compared with the floor.
Step 7: Examine the Manus
Examine the digits by moving the joints through full range of motion and palpating the phalanges. Examine the manus for broken toenails, wounds, draining tracts, dermatologic pathology, and other evidence of foreign bodies or trauma.
Step 8: Palpate the Metacarpal Bones
Palpate the metacarpal bones for swelling, pain, or instability.
Step 9: Palpate the Carpus
Palpate the carpus for abnormalities (ie, CREPI). Evaluate for normal range of motion in extension (A) and flexion (B). Apply varus (C) and valgus (D) stresses to evaluate for instability in the lateral and medial aspects of the joint, respectively.

A
Author Insight
Carpal effusion is typically easy to palpate because the carpus has minimal soft tissue coverage.
Step 10: Assess the Abductor Pollicis Longus Tendon
Palpate for swelling and pain associated with the abductor pollicis longus tendon, which crosses the cranial surface of the distal radius from lateral to medial.
Author Insight
Swelling associated with this tendon is located proximal to the carpus (line), helping differentiate it from joint effusion (arrow).
Step 11: Palpate the Radius & Ulna
Palpate the radius and ulna for instability, swelling, and pain. Palpate the mid to distal radius medially between muscle bellies (arrows) and the proximal radius on the lateral aspect of the limb below the elbow joint (dashed arrows).

Step 12: Palpate the Elbow
Evaluate the elbow for abnormalities (ie, CREPI). Assess for pain in the medial compartment (common in dogs with elbow dysplasia) by palpating the medial epicondyle of the humerus (circle), sliding one finger distally between muscle bellies until the level of the joint is reached (X), and applying pressure.

Step 13: Perform a Campbell's Test
Flex the elbow to 90 degrees, and pronate (A) and supinate (B) the distal limb to assess for collateral ligament laxity and/or injury (ie, Campbell’s test).

A
Author Insight
The anconeal process aids in stability when the joint is extended.
Step 14: Palpate the Humerus
Palpate the humerus for swelling, pain, and instability.
Author Insight
The distal humerus is most easily palpated between muscle bellies on the lateral and medial aspects. The proximal humerus is most easily palpated on the lateral aspect only. The radial nerve passes laterally over the distal third of the humerus. Direct palpation results in a pain response and should be avoided.
Step 15: Palpate the Shoulder
Assess the shoulder joint for abnormalities (ie, CREPI). When performing range of motion, isolate the shoulder joint as much as possible. Extend the shoulder by placing one hand behind the elbow with the other hand at the cranial aspect of the distal scapula and applying cranially directed pressure on the elbow (A). Flex the shoulder by placing one hand on the cranial aspect of the distal humerus and moving the elbow proximally toward the dorsal ribcage (B).

A
Step 16: Perform a Biceps Tendon Test
Perform a biceps tendon test by extending the elbow while the shoulder is flexed to place maximum tension on the tendon. Concurrently palpate the tendon in the intertubercular groove to assess for pain.
Author Insight
Careful localization of pain to the shoulder or biceps tendon (rather than the proximal humerus) is important, as certain bone tumors are commonly located in the proximal humerus.

Step 17: Palpate the Scapula
Palpate the scapula for swelling, pain, and instability.
Step 18: Palpate the Axilla
Palpate the axilla for pain, swelling, and obvious soft tissue masses.
Listen to the Podcast
Dr. Barnes shares her tips for conducting an effective examination and gait assessment in lame patients, including how clients can play a helpful role at home, in this podcast episode.