Linear-Stapled Gastrointestinal Anastomosis
Daniel J. Lopez, DVM, University of Guelph
Ameet Singh, DVM, DVSc, DACVS (Small Animal), University of Guelph
Daniel D. Smeak, DVM, DACVS, Colorado State University
Intestinal resection and anastomosis is commonly performed in small animal practice to remove segments of bowel that are devitalized or diseased, often due to foreign material or neoplasia.1
In human and veterinary medicine, stapling devices have been developed for GI surgery, and a variety of different stapling techniques for intestinal anastomosis have been described, including1-10:
Everting, triangulating end-to-end anastomosis (EEA) using a thoracoabdominal linear stapler
Inverting EEA using an EEA circular stapler
EEA using a skin stapler
Antiperistaltic side-to-side (ie, functional end-to-end) anastomosis using a GI anastomosis (GIA) linear and/or cutting stapler
Stapled GIA in dogs and cats and, more recently, a technique in dogs for a stapled functional end-to-end anastomosis (SFEEA) using only a GIA stapler have also been reported.10,11 Ideally, SFEEA is used following enterectomy of the jejunum and/or ascending duodenum based on the mobility of this portion of the small intestine. Other portions of the intestine (eg, duodenum, large intestine) are more fixed because of the short mesentery, precluding the use of this technique.
Studies have been conducted to evaluate the technique and outcome of SFEEA in veterinary medicine.1,12-14 Potential benefits of SFEEA as compared with hand-sewn anastomosis include reduced procedure time, decreased tissue trauma, decreased intraoperative contamination, consistency and repeatability of the anastomosis, and preservation of blood supply.13-15 In addition, severe luminal disparity between 2 cut bowel ends (eg, severe segmental dilation orad to an obstructive foreign body) can be readily resolved via SFEEA. A multi-institutional retrospective study in dogs demonstrated no significant difference in anastomosis dehiscence rates or decreased procedure time with SFEEA as compared with hand-sewn anastomosis.12
Disadvantages of SFEEA as compared with hand-sewn anastomosis include the learning curve required to perform the procedure and the inability to perform this procedure in areas of the GI tract other than the jejunum and ascending duodenum. An additional limiting factor of stapled anastomosis may be financial investment, with SFEEA instruments and staple cartridges costing 15 to 25 times more than suture costs.14 However, in some institutions, the total procedural time saved may result in equivalent overall costs between SFEEA and hand-sewn anastomosis.
Preoperative peritonitis, a serum albumin concentration less than 2.5 g/dL (25 g/L), and presence of an intestinal foreign body are classically reported risk factors for intestinal anastomosis dehiscence following hand-sewn anastomosis.16 In a retrospective study examining risk factors specifically related to SFEEA dehiscence, preoperative presence of inflammatory bowel disease, intraoperative hypotension, and resection and anastomosis involving the large intestine were identified as risk factors.14
Preoperative peritonitis was examined and was not an identified risk factor for SFEEA, contrary to previous reports.14 Furthermore, in another retrospective study, SFEEA was found to be less likely to undergo dehiscence as compared with hand-sewn intestinal anastomosis in dogs with preoperative septic peritonitis.1
With proper instruction, SFEEA has been demonstrated to be a reliable tool for surgeons and may be useful during emergency situations to decrease operative time in unstable patients when a rapid anastomosis is required and to potentially decrease dehiscence risk in patients with septic peritonitis.13,14
Surgical Stapler Functionality
Before performing a linear-stapled intestinal anastomosis, the surgeon should become familiar with the GIA stapling device used for SFEEA (Figure 1). The GIA stapler is a linear/cutting stapling device composed of 2 interlocking halves. When fired via a push-bar handle, the device applies 4 staggered rows of B-shaped titanium staples while a knife blade cuts between the 2 rows of double staple lines (Figure 2). The knife blade stops cutting approximately 8 mm before the last staple at the tip of the fork.
Staple cartridges for the directional stapling technology (DST) series GIA stapler come in different lengths and closed staple heights. The color of the cartridge corresponds to the closed staple height. Blue staple cartridges (1.5-mm closed staple height) are typically used in small animals for SFEEA. White (1-mm closed staple height) and green (2-mm closed staple height) staple cartridges are also available but are not routinely used for SFEEA.
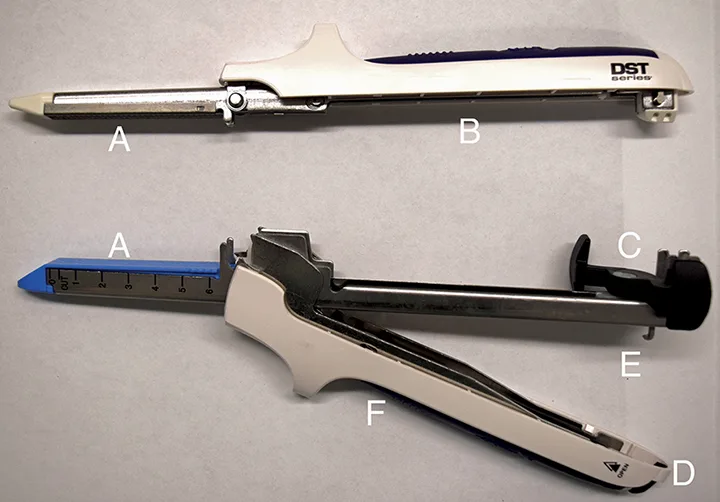
Figure 1 A DST series GIA 60 stapler. Stapler forks (A), stapler handle (B), push trigger (C), release mechanism (D), locking mechanism (E), cartridge lock lever (F; a blue cartridge is loaded in the opposite side of the handle)
STEP-BY-STEP
STAPLED FUNCTIONAL END-TO-END ANASTOMOSIS
WHAT YOU WILL NEED
Standard surgical instrument kit
Balfour retractor
GIA stapler (60-mm and/or 80-mm or 100-mm for medium-to-large–breed dogs) and blue staple cartridges that correspond in length to the stapler
Doyen intestinal forceps (atraumatic; 2 pairs)
DeBakey thumb forceps (2 pairs)
Traumatic forceps (eg, Rocheter-Carmalt; 1 pair)
Suture material (3-0 monofilament, absorbable)
STEP 1
Anesthetize the patient and place in dorsal recumbency. Administer antimicrobial therapy (eg, cefoxitin [30 mg/kg IV for clean-contaminated surgery]) 30 minutes before incision and every 90 minutes thereafter until skin closure; of note, recent data suggest that q4h administration of cefoxitin is also acceptable.17 Clip, prepare, and drape the ventral abdomen for aseptic surgery.
Perform a ventral midline exploratory laparotomy and remove the falciform ligament to improve abdomen exposure, then place a Balfour retractor. Explore the abdomen thoroughly in a systematic fashion, and isolate the affected intestinal segments with multiple layers of saline-soaked laparotomy sponges. Perform an enterectomy and, if indicated, submit for histopathologic evaluation.
Author Insight
An initial pair of Doyen forceps (gripping the portion of bowel to remain intact) can help with intestinal manipulation and resection and anastomosis, and traumatic forceps (gripping the portion of bowel to be removed) can help limit surgical-site contamination. When placing Doyen forceps, only one ratchet should be used to prevent devitalization of tissue. Although the initial Doyen forceps are placed at the traditional site of hand-sewn anastomosis, this portion of tissue will be removed after SFEEA completion.
STEP 2
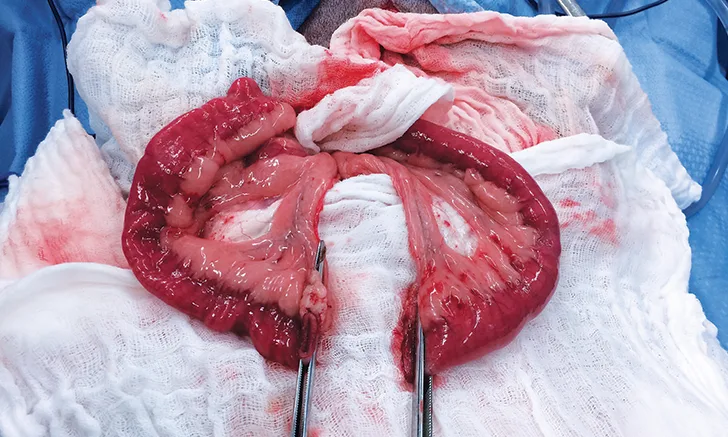
After resecting the affected intestine, milk the intestinal contents orally and aborally to the Doyen forceps (A). Place a second pair of Doyen forceps approximately 10 cm orally and aborally to the first set of Doyen forceps (B). This technique is employed to minimize contamination when using the stapling devices for anastomosis, as the initially placed pair of forceps will be removed on staple application.
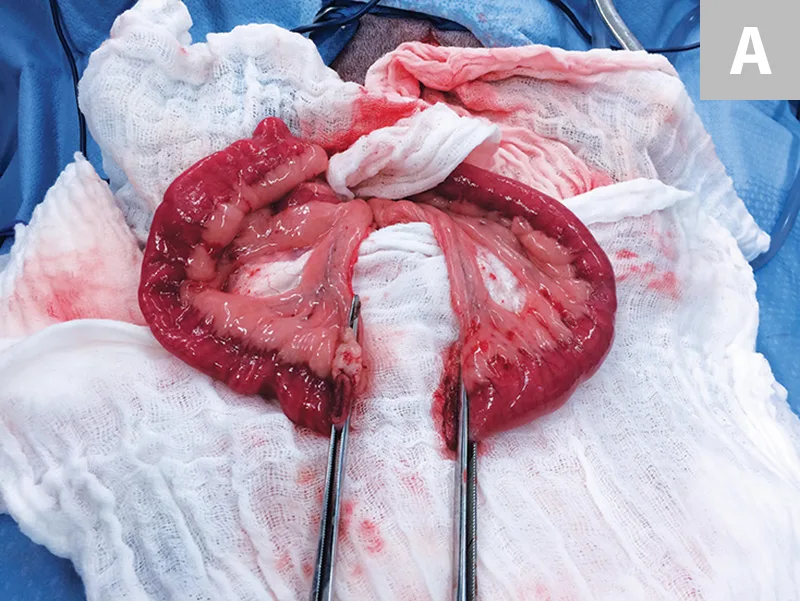
Proximal and distal segments of the jejunum occluded by Doyen forceps at the site of resection (A). The resected portion of the intestine was removed from the surgical site with Rochester-Carmalt (ie, traumatic) forceps attached (not pictured). Proximal and distal jejunal segments of the intestine with second Doyen forceps placed approximately 10 cm away from the initial Doyen forceps (B; black arrows)
STEP 3
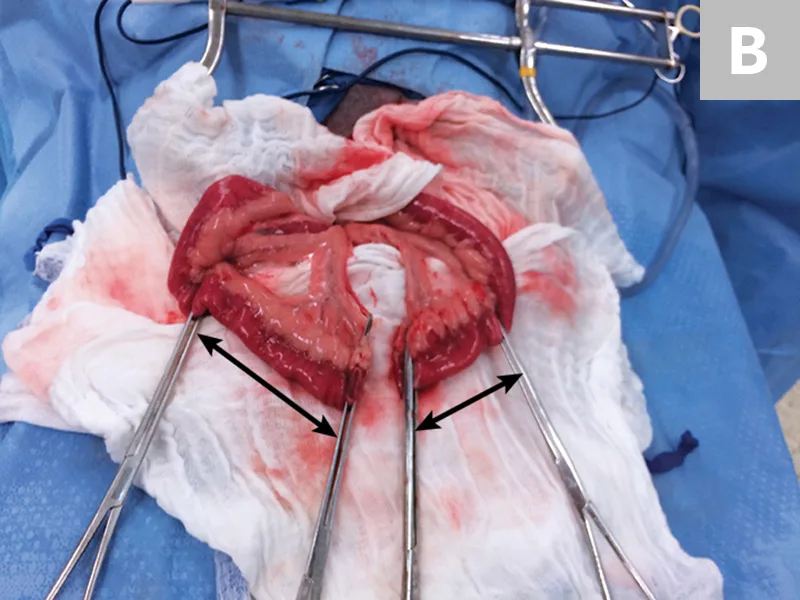
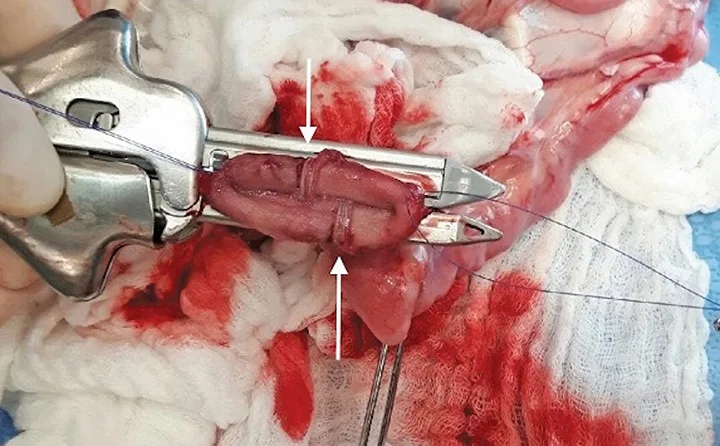
Place 2 stay sutures (eg, 3-0 polydioxanone) into the cut ends of each intestinal segment on the mesenteric border. Once the stay sutures have been applied, remove the first pair of Doyen forceps directly at the cut bowel ends; leave the second pair in place until the stapled anastomosis is complete. Use the stay sutures to elevate the bowel ends and to facilitate insertion of each fork of the GIA stapler (A). It is important to ensure symmetrical apposition of the antimesenteric border of the intestine before locking the stapler. The authors recommend apposition of the antimesenteric borders of the bowel because this can help minimize incidence of trauma to the vascular supply on the mesenteric border.


Two stay sutures have been placed at the mesenteric border of the jejunum, and the initially placed Doyen forceps have been removed (A). The stay sutures are elevated to allow for insertion of the individual forks of the GIA stapler into the lumen of both jejunal ends. The GIA stapler is engaged and locked, ensuring symmetrical apposition of the antimesenteric border and terminal end of the jejunum (B). The GIA stapler is then fired. The stay sutures (black arrows) can be noted.
When placement is deemed adequate, lock and fire the forks, creating the side-to-side opening between the bowel lumens (B). After firing, disengage and remove the forks. Carefully inspect the anastomosis site to ensure proper staple placement, which is dependent on passage of the staple fully through both layers of the adjacent intestinal wall and on consistent closure of the B-shaped staple on the opposite tissue edge.
Author Insights
Caution should be exercised when using this stapling technique for anastomosis in cases in which the intestinal wall is severely thickened (eg, inflammatory bowel disease), as the closed blue cartridge staple leg length (1.5 mm) may not be long enough to completely capture both intestinal walls.14 In cases of severely thickened intestines, hand-sewn anastomosis is recommended.
Future obstruction at the site of anastomosis is a potential long-term risk, with one report documenting subsequent obstruction in 4.3% of SFEEAs.18 The authors routinely use a GIA 60 stapler for the first half of the SFEEA; in their clinical experience, a GIA stapler of longer working length, although not harmful, does not appear to be beneficial in preventing subsequent obstruction. Further investigation in this area is needed.
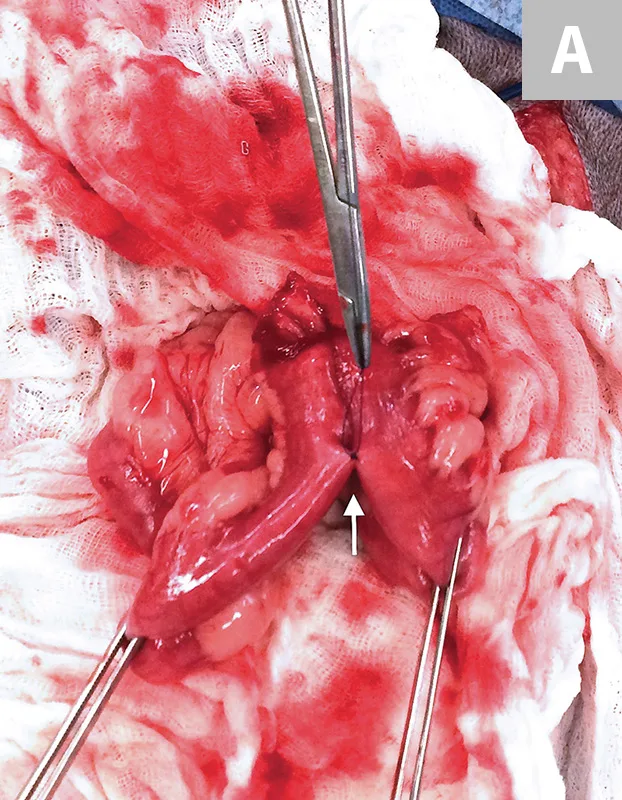
STEP 4
Using the previously placed stay sutures for handling the intestinal segments, place the GIA stapler (with a new loaded cartridge) perpendicular to the lumen of the intestine. Before locking, offset the staple rows from the lumens portion using 2 pairs of DeBakey thumb forceps. This prevents the initial staple lines from being stacked on top of each other, which could prevent complete engagement of the staples through both walls of the terminal end of the SFEEA. Lock and fire the stapler. The authors generally aim to leave 1 mm to 3 mm of tissue beyond the edge before firing the GIA stapler. The GIA stapler will automatically transect the bowel, resulting in a 2-row stapled edge creating the “waist.” The remaining tissue at the terminal end of the SFEEA does not need to be oversewn.
The 2 previously placed stay sutures are gently distracted to maintain tension on the intestine. A GIA stapler (of appropriate length) is engaged and locked over the terminal end of the intestine. Approximately 3 mm of tissue extends beyond the proposed staple line, and no tissue extends past the 0 mark of the GIA stapler, ensuring a complete terminal seal. If tissue extends past the 0 mark of the GIA stapler, a stapler of longer working length should be used. The stapler is fired, resulting in a stapled terminal end of the intestine and transection of the remaining distal portion, including the stay sutures. The 2 staple lines of the GIA line should be offset (white arrows) to ensure staple engagement of all tissues.
Author Insight
The GIA 60 stapler is often too short to adequately engage all tissues when closing the terminal end of the SFEEA in medium-to-large–breed dogs; in such patients, a GIA 80, 90, or 100 stapler is recommended.
STEP 5
Two simple interrupted, prolonged absorbable monofilament sutures should be placed just below the base (ie, point of the “V” intersecting GIA staple line) of the anastomosis to minimize tension on the staple line (A). These sutures should aim to capture submucosa for holding power (B).
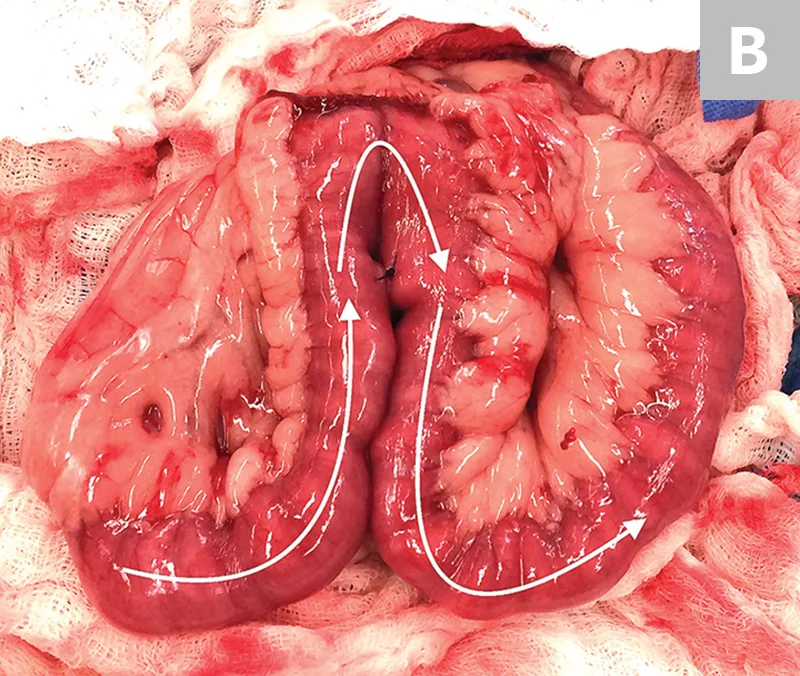
Two simple interrupted, prolonged absorbable monofilament sutures are placed at the SFEEA base (A; white arrow) to minimize tension on the staple line. Completed SFEEA, with a demonstration of the flow of ingesta through the SFEEA (B; white arrows)
STEP 6
Remove the laparotomy sponges from the surgical field. With a new pair of sterile surgery gloves, use a separate sterile closure pack to complete the laparotomy. Lavage the abdomen thoroughly with sterile saline. Using a monofilament absorbable suture, close the mesenteric defect in either an interrupted, cruciate, or continuous pattern. Avoid damaging adjacent vasculature supplying the anastomosed bowel in the mesentery. Drape the omentum over the anastomosis site before closing the abdominal incision in a routine fashion, and perform a routine closure of the abdomen.
DST = directional stapling technology, EEA = end-to-end anastomosis, GIA = gastrointestinal anastomosis, SFEEA = stapled functional end-to-end anastomosis<