This response is incorrect. See below for the correct answer.
Left-Sided Congestive Heart Failure
Jessica McGinnis, DVM, University of Florida College of Veterinary Medicine
Amara H. Estrada, DVM, DACVIM (Cardiology), University of Florida

Left-sided congestive heart failure (L-CHF) is a life-threatening condition caused by venous congestion secondary to increased left atrial pressure. This pressure occurs when the left ventricle is unable to adequately fill with or eject blood because of a primary structural or functional cardiac condition.1
L-CHF patients may initially show no clinical signs; however, those that present with acute dyspnea must receive appropriate treatment before undergoing testing to establish the diagnosis. (See Table 1for a list of common conditions that cause L-CHF in dogs and cats.)
Common Primary Cardiac Conditions Causing Left-Sided Congestive Heart Failure in Dogs & Cats
Clinical Signs
Cats and dogs may appear clinically normal in the early compensatory phase of L-CHF. Monitoring sleeping respiratory rates (SRR) at home can help detect early L-CHF in patients with known cardiac disease. A sustained SRR of more than 30 breaths per minute may be indicative of potential decompensated CHF.2 As the disease progresses and the patient reaches the decompensated phase of L-CHF, pulmonary edema can cause tachypnea and increased inspiratory effort.3 In cats, pleural effusion can also be present, resulting in short, shallow breathing with increased inspiratory effort.1 Dogs with L-CHF can develop tachycardia as the heart compensates to increase cardiac output.3
Thoracic auscultation may disclose crackles or harsh bronchovesicular sounds in dogs and cats with pulmonary edema and decreased bronchovesicular sounds ventrally in cats with pleural effusion.1,3 The absence of these findings, however, does not rule out the presence of L-CHF. Cats, for example, do not breathe deeply enough to manifest obvious pulmonary crackles even with severe dyspnea. Decreased rectal temperature, pale mucous membranes, and prolonged capillary refill time because of vasoconstriction and decreased peripheral perfusion may also be observed, and cardiac arrhythmias may be present, depending on the underlying condition.1,3 Coughing does not always indicate that a dog with cardiac disease has L-CHF, as small dogs frequently have a paroxysmal-to-sustained cough related to compression of the mainstem bronchus secondary to cardiac enlargement.4 In these patients, thoracic radiography is needed to establish the diagnosis and guide treatment.
Patients with acute dyspnea should undergo aggressive stabilizing treatment before any ancillary diagnostic testing is performed.
Diagnosis
If clinical signs are not immediately life-threatening, at a minimum, a lateral thoracic radiograph should be obtained. Thoracic radiography is the gold standard for diagnosing pulmonary edema and venous congestion secondary to L-CHF.3,5 If the patient is not in distress, a 3-view study with a ventrodorsal or dorsoventral (VD/DV) view and opposite lateral thoracic views is ideal. Characteristic findings of cardiogenic pulmonary edema include increased interstitial-to-alveolar infiltrates of the perihilar and/or caudodorsal lung field in dogs.3,5 (See Figures 1A and 1B.)
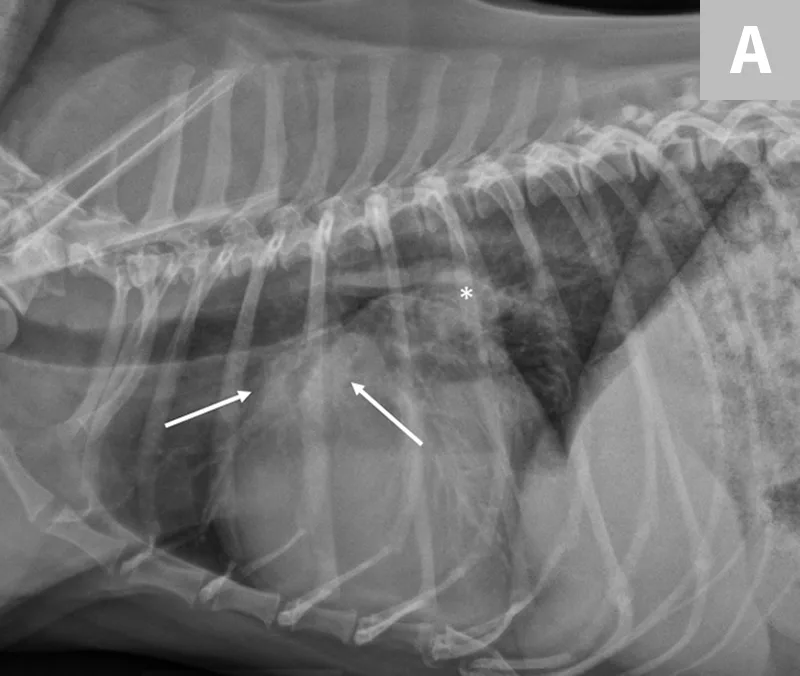

(A) L-CHF in a Cavalier King Charles spaniel with mitral valve disease. Enlarged cranial lobar vessels are marked by the arrows. Enlarged left atrium is marked with an asterisk. (B) DV projection shows a caudal interstitial-to-alveolar pattern with air bronchograms (arrow). Images courtesy of University of Florida Small Animal Hospital
In cats, a ventral or diffuse interstitial-to-alveolar pattern may be present3,5; pleural effusion is indicated by pleural fissure lines, retraction of the lung lobes, and effacement of the cardiac silhouette.6 (See Figure 2.) Dyspneic cats with evidence of pulmonary infiltrates should receive a presumptive diagnosis of cardiogenic pulmonary edema until proven otherwise (often by a clinical diuretic trial).

L-CHF in a cat with cardiomegaly and pleural effusion with visible pleural fissure line (arrow).
Left atrial enlargement is typically present in both cats and dogs with L-CHF. In dogs, left atrial enlargement typically appears in radiographs as a rounded increased opacity caudal to the carina in the perihilar region on the lateral projection. (See Figure 1A.) Generalized cardiomegaly is identified by measuring vertebral heart score (VHS).3,5 (See Figure 3.) In cats, both generalized cardiomegaly and left atrial enlargement are more difficult to assess because of their more subtle radiographic changes; they are characterized by a VHS score greater than 8 and the presence of a valentine-shaped heart on the VD/DV projection, respectively. However, normal left atrial size on thoracic radiography does not rule out the presence of L-CHF in dyspneic cats.1 Once acute L-CHF has been identified and treated, evaluation by a cardiologist is recommended, but stabilization of the patient is the first priority.
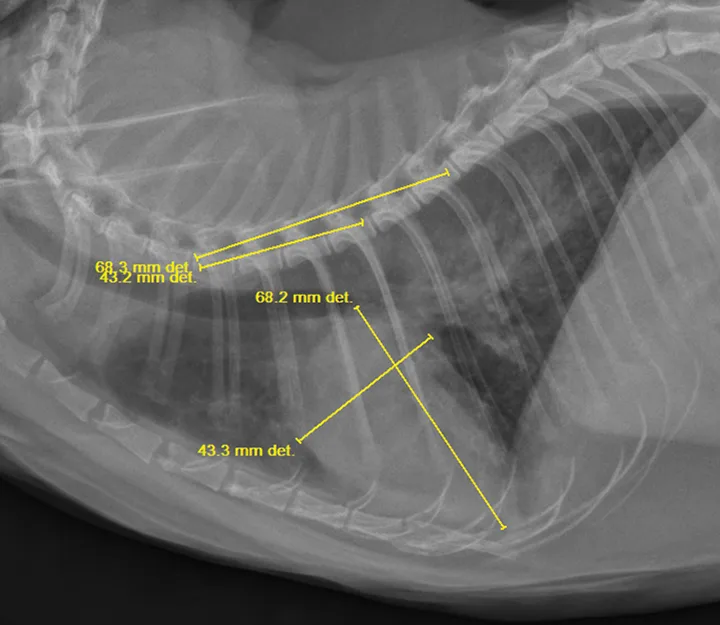
VHS of 10.5 in a cat. Normal VHS for cats and dogs is less than 8.0 and less than 10.5, respectively. Note the diffuse interstitial-to-alveolar lung pattern, which most likely represents cardiogenic pulmonary edema.
Additional initial diagnostics include blood pressure measurement and renal and electrolyte studies to assess the patients perfusion and kidney function before initiating diuretic therapy.1,3,7 Additionally, an NT-proBNP ELISA SNAP test can be performed when the diagnosis of L-CHF is in question.
NT-proBNP is a biomarker that, when present, can indicate the presence of cardiac remodeling. In recent studies, the point-of-care SNAP test has been shown to have a 65% sensitivity and 100% specificity.8 However, these studies did not include normal cats and specificity results may have been skewed. Nevertheless, a positive NT-proBNP SNAP test can raise clinical suspicion of L-CHF and prompt the practitioner to treat accordingly.
Treatment
Acute L-CHF is treated with oxygen supplementation and diuretic therapy.1,3,7,9 (See Figure 4.) Oxygen can be administered via flow-by, oxygen cage, or nasal oxygen cannulas and should be provided until the patient is eupneic in room air (ie, 21% oxygen).1,3 In cats, empiric treatment with an albuterol inhaler can also be considered; however, this should be avoided if proven that it adds extra stress to the patient.
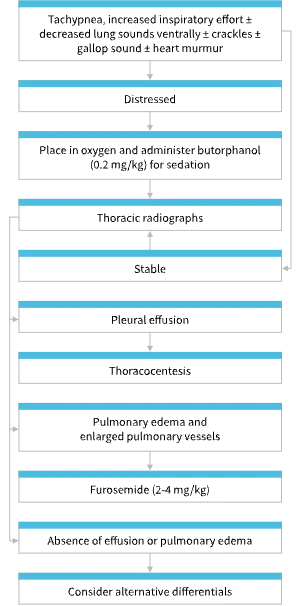
Algorithm for recognizing, diagnosing, and treating feline CHF.
Furosemide is the initial diuretic of choice and should be administered at 2 to 4 mg/kg IV.1,3,7 If IV access is not possible because of patient distress, furosemide can be administered IM.9 Maximal effect is expected within 30 minutes of IV administration and within 1 to 2 hours of IM administration.7,9 Diuretic therapy should aim to relieve respiratory distress. Repeat bolus doses can be administered every 30 minutes until the desired effect is achieved. Ideally, the total daily dose of furosemide should not exceed 12 mg/kg.1
If repeat bolus doses are required, a furosemide CRI at a rate of 0.66 to 1.0 mg/kg/h may be considered.1,3 Thoracocentesis is recommended in cats with clinically significant pleural effusion.1 Because azotemia and hypokalemia may develop with the use of a loop diuretic (eg, furosemide), renal and electrolyte values should be monitored daily in hospitalized patients receiving treatment for acute L-CHF. These values should be rechecked within 1 week of initiating oral furosemide dosing at home.1,3,7 Note that IV fluid therapy is contraindicated in the treatment of L-CHF.
Patients are considered to be in compensated L-CHF once they are eupneic in room air. Long-term treatment of compensated L-CHF includes oral administration of furosemide and an ACE inhibitor and treatment of the underlying condition.1,3,7 Use of pimobendan, a positive inotrope, is recommended in dogs with stage B2 and C myxomatous mitral valve disease and dogs with dilated cardiomyopathy. Pimobendan has been shown to prolong the time to onset and recurrence of L-CHF.10-13 No prospective literature supports the use of pimobendan in cats, but retrospective studies have suggested a potential benefit of this drug in cats with hypertrophic cardiomyopathy and L-CHF, especially those with systolic dysfunction and without systolic anterior motion of the mitral valve.14,15
Conclusion
L-CHF is often a life-limiting disease. However, patients who receive an initial diagnosis of L-CHF have an approximate survival-to-discharge rate of 80%, and patients typically have a good quality of life during treatment of compensated L-CHF.1 (See Resource.)
In a well-managed patient nave to previous cardiac medications, the average survival time with L-CHF is 6 to 12 months.1,11 SRR is a valuable parameter for owners to measure at home and, when increased, indicates the need for prompt treatment.2 Continued follow-up care, including repeat measurement of renal and electrolyte values, thoracic radiography (if indicated), and echocardiography is an important aspect of L-CHF management.
This article originally appeared in the January/February 2018 issue of Veterinary Team Brief.