Isoflurane & Sevoflurane: Application & Protocols
Patrick M. Burns, BVSc, MANZCVS, DACVAA, University of Montreal
Part 2 of this 2-part series reviews the use and follow-up protocols associated with common inhalant anesthetic agents. Part 1 (December 2014 issue) discussed the pharmacologic effects and mechanisms of these agents.
Related Article: Isoflurane & Sevoflurane: Mechanics & Effects
Respiratory Circuit & Anesthetic Agent Concentration
Anesthetic Circuits
Non-rebreathing circuits
If using a non-rebreathing circuit (eg, modified Jackson-Rees circuit), the percentage of anesthetic agent inhaled by the patient is considered known (fraction inspired agent = FI); it is the same as the vaporizer percentage.
The increase in the FI anesthetic agent occurs within seconds.
Simply changing the percentage on the vaporizer alters the anesthetic depth.
Rebreathing circuits (circle circuits, F-circuits, filter circuits)
A rebreathing circuit can take 5–10 minutes to obtain a FI agent concentration equal to the vaporizer.
This is a function of the time-constant of the rebreathing circuit.
Time constant [min] = volume of the circuit [liters] ÷ fresh gas flow [liters/min]
The duration of 3 time constants needs to pass before the concentration of anesthetic in the circuit is approximately of the same value of the vaporizer.
The FI anesthetic agent in a rebreathing circuit is lower than the percentage of vaporizer because of the dilution of the anesthetic agent by exhaled gas, which is already present in the circuit.
Increasing fresh gas flow accelerates the rate of change of anesthetic concentration.
This flushes out the nitrogen already in the circuit and patient and replaces it with oxygen and anesthetic agent.
The percentage on the anesthetic vaporizer, fresh gas flow, volume of the circuit, and uptake of the anesthetic agent by the patient all influences the rate of change in the FI anesthetic agent.
Other sources of anesthetic loss from the circuit are the adsorption of anesthetic agent onto the circuit itself and degradation by the CO2 absorber.
Rubber and plastic tubing can adsorb a significant amount of isoflurane.
Sevoflurane binds less to rubber and plastic (Figure 1).<sup1 sup>
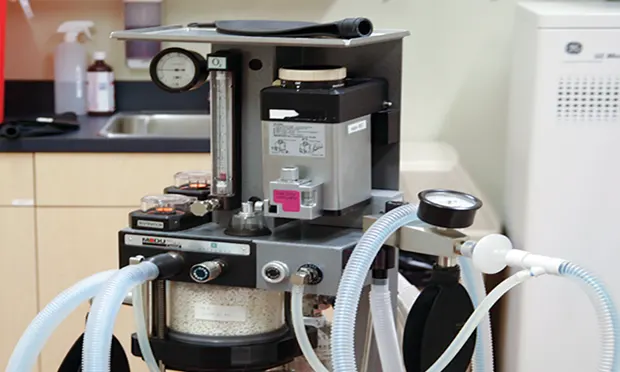
Figure 1. Adsorption of anesthetic onto the rubber and plastic tubing of an anesthetic machine or degradation by the CO2 absorbent can significantly slow the rate of increase of the FI anesthetic concentration and the fraction alveolar anesthetic concentration. An example of a coaxial circle circuit can be seen on the left and a modified Jackson-Rees circuit (non-rebreathing) on the right.
Time constant = Volume of the circuit ÷ Fresh gas flow
This calculation describes the time it takes to fill the respiratory circuit one time and can estimate the concentration of a volatile anesthetic in a respiratory circuit assuming a constant fresh gas flow. This equation does not take into consideration the anesthetic uptake by the patient or the adsorption of the anesthetic onto the anesthetic circuit. The percentage of change (final concentration – original concentration) of the inhalant anesthetic is a function of the number of time-constants (ie, following 1, 2, 3, 4, or 5 multiples of the time constant, the percentage of change will be 63.2%, 86%, 95%, 97.5%, and 99.9%, respectively). For example, if 2% of isoflurane is chosen on the vaporizer, the percentage of change after filling the circuit once will be 63% of the difference between the starting isoflurane concentration (0% in this example), and the final isoflurane concentration chosen on the vaporizer (ie, 63 ÷ 100 × [2% – 0%] = 1.26%); therefore, the approximate concentration of isoflurane in the circuit will be 1.26%. Note: The graph of the isoflurane percentage (black line) overlies the percentage of change line (gray line) and cannot be seen.
CO2 Absorbents
Sevoflurane can be degraded by moist CO2 absorbents to a potentially nephrotoxic compound (compound A).
In the clinical human setting, the quantity of compound A produced does not commonly cause adverse effects, even with the use of low-flow anesthesia.<sup1 sup>
When using oxygen flows of less than 500 mL/min, the concentration of compound A was lower than the renal toxic dose reported in rats.2
Higher concentrations of compound A are associated with prolonged sevoflurane administration at high concentrations, low-flow anesthesia, the use of barium hydroxide and soda lime, and higher absorbent temperatures.
The use of soda lime produces less of compound A when compared with barium hydroxide.
When monovalent bases are absent from the CO2 absorbent, the production of compound A from sevoflurane does not occur.
Desiccated CO2 absorbents degrade volatile anesthetics, resulting in production of carbon monoxide.
It is important to avoid desiccation of CO2 absorbents.
Desiccation has been seen with desflurane and, to a lesser extent, with isoflurane.
Neither volatile agents have degradation with the newer CO2 absorbents (eg, calcium hydroxide lime), so there will be no formation of compound A or carbon monoxide.
Low-Flow Anesthesia
Reducing fresh gas flow reduces the amount of anesthetic agent used, decreasing anesthesia cost and environmental impact.
All volatile anesthetic agents degrade the ozone layer.
Low-flow anesthesia is used only with a rebreathing system.
A high fresh gas flow must be maintained to eliminate the CO2 when using a non-rebreathing system.
The lower the fresh gas flow, the more difficult it can be to predict the FI and alveolar anesthetic concentrations.
The anesthetic alveolar concentration is proportional to the anesthetic concentration of the blood and brain.
This is the true measure of anesthetic depth, not vaporizer setting.
When using a rebreathing system, the lowest flow rate possible for any patient is the oxygen consumption rate as defined as VO2 = 10 × (body weight [kg])<sup0.75sup>.
This is based on Kleiber’s Law.
This can be estimated by assuming a metabolic rate of 3–5 mL/kg/min for most mammalian species.
Low-flow anesthesia cannot be used at the beginning of an anesthesia event.
A fresh gas flow that is sufficiently fast enough to obtain a steady-state of FI anesthetic agent must be used.
After a plateau has been obtained, fresh gas flow may be reduced closer to the oxygen consumption rate.
An analyzer of anesthetic agents is best used to help the operator identify the true concentration of inspired anesthetic agents.
Table. Low-Flow Anesthesia: Advantages & Disadvantages
Use of Inhalant Anesthetic Agents
From Induction to Maintenance
The pharmacodynamic profile of the inhalant anesthetic agent predicts the time available to intubate the patient; desflurane has the shortest available time of these agents.<sup1,3,4 sup>
Often, this time is quite short and is one reason why inhalant anesthetic agents are not frequently used for induction of anesthesia.
Pollution and elevated patient stress are other reasons not to use inhalant anesthetic agents for induction.
Injectable anesthetic agents often provide a more secure environment for induction.
The anesthetic concentration of the breathing circuit must be approaching the minimum alveolar concentration (MAC) before the effects of the injectable agent wear off.
During and immediately after intubation, the patient’s depth of anesthesia dictates the initial percentage of anesthetic used and the fresh gas flow.
Coughing during intubation, tachycardia, hypertension, breath-hold or tachypnea, lack of muscle relaxation, and brisk reflexes all suggest a light depth of anesthesia.
In this instance, an injectable agent has the shortest onset time when compared with an inhalant anesthetic.
An additional bolus of an injectable agent would be warranted in this situation.
Related Article: Anesthesia Monitoring: Raising the Standards of Care
Choosing the Appropriate Settings
Non-rebreathing circuit
The fresh gas flow is normally fixed at 2–3 times the respiratory minute ventilation.
The FI anesthetic concentration is the same as the percentage on the vaporizer.
Rebreathing Circuit
More complicated because of the dilution of the fresh gas by the exhaled gas.
This effect lowers the concentration of the anesthetic agent.
Concentration estimation of the anesthetic agent in the circuit can be performed as follows:
Assuming the rebreathing circuit is a closed system, the time constant of the circuit can be estimated by calculating the ratio of the volume of the circuit (Vol, L)/fresh gas flow (FGF, L/min).
The concentration in the circuit will likely be lower because of anesthetic uptake by the patient and adsorption of anesthetic by the CO2 absorber and respiratory tubing.
After a period equal to 3 time constants has passed, concentration of anesthetic in the circuit is approximately 95% of the value of the vaporizer percentage.
When a steady state has been attained, the fresh gas flow can be reduced.
This reduces the cost of anesthesia because of the reduction in output of the vaporizer and oxygen used.
The depth of anesthesia should always guide the practitioner because of individual variability in response to anesthetic agents.
Each patient has a specific MAC.
Other drugs used for anesthetic protocol (ie, sedatives, analgesics, local anesthetic agents), specific diseases, and physiologic conditions can affect MAC.
Time constant plot
This graph demonstrates the effect of changing the duration of the time constant of the respiratory circuit. A time constant = Volume of the circuit (L) ÷ fresh gas flow (L/min). For example: A respiratory circuit has a volume of 5 L and the operator has chosen 2% on the isoflurane vaporizer. Decreasing the fresh gas flow from 5 L/min to 1 L/min to 0.5 L/min can prolong the time constant of the circuit. The resulting three saturation curves are shown based on this equation (ie, 1 minute, 5 minutes, 10 minutes, respectively). After one time constant, the concentration of isoflurane in the respiratory circuit is the same; however, the time required is progressively longer. Assuming an approximation for the elimination of propofol following an IV bolus, it can be seen that the level of anesthesia may be insufficient to maintain the patient anesthetized as indicated by the MAC-Awake line. By definition, this is the MAC of an inhalant anesthetic with which an animal will spontaneous awaken. The isoflurane MAC is indicated by the solid line.
Manipulation of Anesthetic Depth with a Rebreathing Circuit
When the patient has reached surgical anesthetic plane, the fresh gas flow can be reduced to one closer to the patient’s oxygen consumption rate.
A greater percentage of the exhaled gas will be recycled, making the circle circuit more efficient.
Decreasing the fresh gas flow also prolongs the time constant of the circuit (ie, the time required to change the anesthetic concentration of the circuit).
Many anesthesiologists use a fresh gas flow of 0.5 L/min as a compromise between efficiency and responsiveness to changes in anesthetic concentration.
In patients with inadequate depth of anesthesia, the course of action depends on the clinical signs.
If changes are subtle, the anesthesiologist may increase the percentage on the vaporizer only.
The magnitude of the anesthetic concentration change is a function of the fresh gas flow.
The lower the fresh gas flow, the greater the required magnitude of change on the vaporizer.
The patient absorbs a certain volume of anesthetic per minute.
Another option is to increase the fresh gas flow.
This increases the volume of anesthetic agent that leaves the vaporizer and reduces the time constant required to attain the new steady state.
After this, the fresh gas flow may be decreased once again.
It is possible to increase the rate of absorption of the inhalant anesthetic agent by increasing the respiratory minute ventilation, which will increase the uptake of anesthetic.
This effect is more evident with isoflurane because of the higher blood-gas solubility as compared with sevoflurane or desflurane.
When the depth of anesthesia is insufficient and the patient is moving, an injectable anesthetic agent is the option of choice.
The onset time is shorter when compared with inhalant anesthetic agents.
Recovery from Volatile Anesthetics
All factors that influence the uptake of anesthetic agents also influence their wash-out.
The principal route of elimination of inhalant anesthetics is via the respiratory tract.
If ventilation is not supported during the initial phases of the recovery, the elimination time of the anesthetic agent is prolonged.
Because of the higher solubility of isoflurane, muscle and fat compartments are more saturated and act as a reservoir that slows the rate of recovery following long duration anesthesia.
The duration of anesthesia has little effect on the rate of recovery following sevoflurane.
The MAC-awake (ie, the MAC with which an animal spontaneously awakens) for both anesthetic agents is approximately 0.3–0.5 times their respective MAC values.
After a short duration of anesthesia, the recovery rate is similar between isoflurane and sevoflurane.
In this situation, the sedatives and analgesics administered during the preoperative period have a larger impact on the recovery rate than do the inhalant anesthetic agents.
Ventilation, the Anesthetic Machine, & Recovery
Elimination of anesthesia from the body is slowed because of anesthetic saturation of other body compartments.
Off-gassing from circuit tubing, CO2 absorbent, and the exhaled gas of the patient can slow the decrease in anesthetic concentration in the circuit.
Elimination of anesthesia depends on the respiratory minute ventilation; maintenance of the respiratory minute ventilation accelerates rate of recovery.
If the vaporizer is off and the animal detached from the circuit, recovery rate will be slower.
Immediately after disconnection from the circuit, the respiratory minute ventilation of the patient will be depressed, especially if an opioid has been administered.
Use of a mechanical ventilator or manual ventilation during the recovery period shortens the recovery period.
Increasing fresh gas flow to the maximum on the flow meter decreases the time constant and accelerates the rate of decline of anesthetic concentration in the circuit.
Another option is to empty the reservoir bag repeatedly into the scavenging system with the APL (adjustable pressure limiting) valve open.
Related Article: Waste Anesthetic Gas
MAC = minimum alveolar concentration