How to Approach Ischemic Dermatopathy in Dogs
Paul Bloom, DVM, DABVP, DACVD, Allergy, Skin, & Ear Clinic for Pets, Livonia, Michigan

Dog with generalized ischemic dermatopathy. Image courtesy of Charlie Walker, The SkinVet/The PhotoVet
Ischemic dermatopathy (Figure 1) is a syndromic reaction pattern caused by diseases involving cutaneous blood vessels. Some dermatologists have subtyped ischemic dermatopathy into 5 groups1,2: familial dermatomyositis, juvenile-onset dermatomyositis-like disease in atypical breeds, post-rabies-vaccine–associated panniculitis, generalized vaccine-associated ischemic dermatopathy, and generalized idiopathic ischemic dermatopathy.
Familial Dermatomyositis
Familial dermatomyositis occurs in collies, Shetland sheepdogs, and their crossbreeds. The onset of ischemic dermatopathy in these breeds occurs between 6 weeks and one year of age, most commonly before 6 months of age. Recent studies demonstrate that dermatomyositis may be triggered by vaccinations, infections, toxins, drugs, stress, or estrus in genetically predisposed dogs; however, no causal relationship has been definitively proven.2
Juvenile-Onset Dermatomyositis-Like Disease
Juvenile-onset dermatomyositis-like disease in atypical breeds occurs in juvenile dogs that are not collies, Shetland sheepdogs, or their crossbreeds. This is not a familial disease, and the pathogenesis is currently unknown.
Post-Rabies-Vaccine–Associated Panniculitis
Post-rabies-vaccine–associated panniculitis may occur 2 to 12 months after SC or IM rabies vaccine administration. Small-breed dogs (eg, miniature poodles, toy poodles, Yorkshire terriers, silky terriers, bichons frises) appear to be predisposed to ischemic dermatopathy.3 Skin lesions are consistent with ischemic dermatopathy and develop only at the vaccination site. Polyvalent vaccines have also been implicated in the literature and anecdotally.4
Generalized Vaccine-Associated Ischemic Dermatopathy
In cases of generalized vaccine-associated ischemic dermatopathy, lesions develop at and distant from the vaccination site. In some cases, the vaccination site lesion may not be obvious if the surrounding hair has grown over the initial alopecic lesion.
This form of ischemic dermatopathy can be misdiagnosed as idiopathic unless there is an apparent temporal association with vaccination or a concurrent lesion is observed at the vaccination site. The proposed pathogenesis involves formation of an immune complex that triggers a type III hypersensitivity reaction, which leads to complement-induced microangiopathy. Immune complex deposition occurs locally at the site of vaccination (causing a localized lesion) and in other cutaneous small vessels at distant sites (creating lesions distant from the vaccination site).
Generalized Idiopathic Ischemic Dermatopathy
The idiopathic form of ischemic dermatopathy occurs in both juvenile and adult dogs5 and may be localized (eg, to the pinnae) or generalized. Lesions are clinically consistent with ischemic dermatopathy.
History
Examination should begin with signalment, ascertaining age at disease onset, and determing whether any relatives of the patient have similar clinical signs.
The following details should be confirmed:
When clinical signs appeared, and how long the lesions have been present
When (and whether) vaccines or drugs were administered, their route of administration, and when the lesions appeared in relation to the time of administration
Whether the lesions are progressing and/or have changed in appearance
Whether the lesions seem painful
Whether the dog is pruritic
Presence of systemic clinical signs (eg, lethargy, anorexia, polyuria/polydypsia, lameness) should be noted, as systemic disease (eg, tick-borne disease, neoplasia, hemolytic anemia) can trigger ischemic dermatopathy.6

Ischemic dermatopathy on a dog’s face. Images courtesy of David Sanmiguel Poveda
Clinical Signs
Early lesions associated with ischemic dermatopathy include scaling, alopecia, plaques, nodules, erosions, and crusts, whereas chronic lesions may have pigmentary changes (hyperpigmentation or depigmentation), cutaneous atrophy, and/or scarring. Pain and pruritus are not common unless ulceration or secondary pyoderma is present. Other than post-rabies-vaccine–associated ischemic dermatopathy, lesion distribution may include the face (particularly periorbital and on the bridge of the nose [Figure 2]), distal extremities, distal pinnae, bony prominences, and tip of the tail.1 Some dogs only have pinnal lesions. In some cases, onychodystrophy may be present (Figure 3).

Onychodystrophic toenails
Diagnosis
Diagnosis of any skin disease is based on detailed patient history, clinical findings (eg, primary lesions, distribution of lesions), laboratory results, and/or therapeutic trials.
Differential diagnoses for ischemic dermatopathy depend on the distribution of the lesion(s). Demodicosis, dermatophytosis, pyoderma, vasculitis, and discoid lupus erythematosus should be ruled out if the skin lesions affect the face, trunk, or limbs. Vasculitis is the primary differential in cases that involve the tip of the tail or the tip/edges of the pinnae.
Initial diagnostics depend on the distribution of the lesions and can be divided into immediate and delayed tests. If the lesions affect the face, trunk, or limbs, initial diagnostics should include deep skin scrapings for Demodex spp and cytology to identify bacterial pyoderma. In patients with suspected dermatophytes, a Wood’s lamp examination, dermatophyte fungal culture, and PCR can be performed; if results are negative, a skin biopsy should be performed. If the skin lesions only involve the tip of the ears or the tip of the tail, these diagnostics (ie, skin scrapings, cytology, dermatophyte tests) are not indicated, and a biopsy should be performed.
In patients with ischemic dermatopathy, histopathologic evaluation of a skin biopsy is key to diagnosis. To get the best yield from the biopsy collections, a history and differential list should be submitted along with the sample, which should be obtained from areas without secondary infections or ulcerations. To capture the full development of ischemic dermatopathy in patients presented with alopecia, it is best to collect nonlesional, healthy-appearing skin and lesional skin at the center and margin/transition to healthy skin (eg, one part in lesional and the other part in healthy skin). This allows the pathologist to see the spectrum of lesional development.
Skin samples can be collected using elliptical and 8-mm punch biopsy instruments. When the dorsal aspect of the trunk is biopsied using a punch, a double punch (ie, a second punch collected in the same site as the first punch) can be performed to obtain subcutaneous tissue. If the ear tips or leading edges of the pinnae are the only area(s) affected with disease, amputation of the tip of the ear or a wedge biopsy of the edge of the pinnae may be necessary. The marginal cutaneous pouch is occasionally involved and can be easily biopsied without risk for ear deformation.
Except for vaccine-associated triggers (ie, panniculitis with focal lymphoid nodule), changes observed on histopathology only identify ischemic dermatopathy patterns of disease, not the trigger. Histopathologic findings are time-dependent and include fading hair follicles, smudging of the dermal collagen, and cell-poor interface change at the dermal–epidermal junction. Apoptotic keratinocytes in the basal cell layer, pigmentary incontinence, and separation of the dermal–epidermal junction may also be present.7
Because idiopathic ischemic dermatopathy is a diagnosis of exclusion, a search for an antigenic trigger should be performed, including investigating the possibility of infection (eg, bacterial, rickettsial), recent drug administration, occult or overt neoplasia, or cutaneous adverse food reaction.<sup2 sup>
Once ischemic dermatopathy is diagnosed, CBC, serum chemistry profile, urinalysis, heartworm test, and vector-borne disease titers should be performed unless a specific trigger (eg, breed, drug or vaccine administration) has been identified. If proteinuria is identified on urinalysis, a urine protein:creatinine ratio should be evaluated. Other diagnostics (eg, Coombs test, antinuclear antibody test, thoracic or abdominal radiography, ultrasonography) may be performed depending on patient signalment and presentation and the results of the initial minimum database.
MEDICATIONS USED TO TREAT ISCHEMIC DERMATOPATHY IN DOGS
Treatment
The underlying cause of ischemic dermatopathy should be identified and treated if possible. In drug-induced cases, future administration of the drug should be avoided. If rabies vaccination is the trigger, the risks and benefits of vaccination versus avoiding vaccination should be assessed. If medically appropriate, local jurisdictions may accept a letter stating it is medically unwise to vaccinate a patient for rabies—this is a serious decision because of the zoonotic risk for rabies.
When planning treatment, severity of disease versus adverse effects of treatment should be considered. Therapeutic options include pentoxifylline, glucocorticoids, oclacitinib, and/or other immunosuppressive agents (eg, mycophenolate, modified cyclosporine, sulfones, sulfasalazine).
Pentoxifylline (15-25 mg/kg PO every 8-12 hours) should be included as first-line therapy because of its safety, positive effects on microcirculatory blood flow, and rheologic and immunomodulatory effects.1,8-11 There may be a 30- to 90-day lag before the patient demonstrates full clinical response.
Pentoxifylline and its metabolites improve the flow properties of blood by decreasing viscosity, although the mechanism of action and sequence of events leading to clinical improvement are still undefined. In patients with chronic peripheral arterial disease, blood flow is increased to the affected microcirculation and enhances tissue oxygenation. Pentoxifylline administration has been shown to produce dose-related hemorrheologic effects, lower blood viscosity, and improve erythrocyte flexibility.1,8-11 Leukocyte properties of hemorrheologic importance have been modeled in veterinary and in vitro human studies. Pentoxifylline has been shown to increase leukocyte deformability and inhibit neutrophil adhesion and activation.8 Tissue oxygen levels have been shown to be significantly increased by therapeutic doses of pentoxifylline in patients with peripheral arterial disease.12
Vitamin E (dogs <55 lb [25 kg], 400 IU PO every 12 hours; dogs >55 lb [25 kg], 800 IU PO every 12 hours)2 and essential fatty acids are used for their anti-inflammatory properties and antioxidant activity; however, there have been no studies evaluating the efficacy of this therapeutic modality in canine ischemic dermatopathy.2,13 When prescribing vitamin E, the author recommends alpha-tocopherol,* as it is preferentially absorbed and accumulated in humans. Vitamin E should be given with a small amount of fatty food to increase absorption.
Topical therapy (ie, glucocorticoids) may initially be used to treat focal lesions to minimize adverse effects associated with systemic glucocorticoid administration. A potent topical glucocorticoid (eg, desoximetasone 0.25%) can be applied every 12 hours until clinical remission (not to exceed 21 days), and then tapered slowly over the next few months.
Although topical steroids are used to avoid systemic adverse effects, systemic signs consistent with steroid administration are possible but rare. If adverse effects occur, or if the lesions fail to respond to topical steroids, topical tacrolimus (0.1%) can be given every 12 hours for 30 days, and then tapered.2 Of note, topical tacrolimus may initially cause transient focal erythema that will resolve as the lesions resolve. Pet owners should wear gloves when handling topical steroids or tacrolimus.
Systemic steroids have historically been the mainstay of therapy for ischemic dermatopathy and are the author's drug of choice for more severe forms of disease; however, oclacitinib has been reported as rapidly effective for resolution of active lesions (eg, erosions, ulceration, crusting).3,14 For mild to moderate cases of ischemic dermatopathy, the author administers oclacitinib (0.4-0.6 mg/kg PO every 12 hours for 30 days [extra-label]) rather than using glucocorticoids.
If the patient is in remission (ie, crusts are in the hair coat or are easily removed from the skin and all ulcers are healed) after 30 days, the author decreases the frequency to once every 24 hours for 30 days, and then to once every 48 hours for 30 days; treatment is then stopped. If treatment every 12 hours for 30 days is ineffective, oclacitinib should be discontinued and oral glucocorticoids should be dispensed.
If clinical relapse occurs during a medication taper, the drug should be increased to the last effective dose and frequency.
In cases of severe, generalized disease, systemic steroids are used as follows:
Prednisone (1 mg/kg PO every 12 hours for 4 days, then 0.5 mg/kg PO every 12 hours for another 10 days), with recheck every 14 days.
If the disease is in remission, the dose should be decreased by 25% every 14 days and not tapered too quickly.
If lesions recur during tapering, a steroid-sparing agent should be added to the treatment regimen.
At 14-day recheck:
If systemic steroids are administered but the disease has not improved, a steroid-sparing agent should be added and the prednisone dose should be increased back to 1 mg/kg PO every 12 hours for 14 days.
If lesions have improved but are not in remission, the dose can be continued and rechecked after 14 days.
At 28-day recheck:
If the disease is still not in remission, a steroid-sparing agent should be added and prednisone should be maintained at the current dose (0.5 mg/kg PO every 12 hours).
If the disease is in remission, the prednisone dose should be decreased by 25%.
Rechecks should be performed every 14 days to determine the effectiveness of the medications, and adjustments should be made based on clinical assessment of lesions (Figure 4).
For patients receiving a steroid-sparing agent in addition to prednisone, prednisone should be tapered first, as it is typically associated with overt adverse effects. Once prednisone has been discontinued or is at its lowest dosage, the steroid-sparing agent can be tapered by 25% every 30 days (other than oclacitinib, as previously described).
In cases in which ischemic dermatopathy does not respond to prednisone, other immunosuppressive agents (eg, mycophenolate, modified cyclosporine, sulfones, sulfasalazine) can be added to therapy. A food trial should also be initiated, as food can trigger ischemic dermatopathy.2 The author only begins a food trial if the disease is unresponsive to additional drugs (eg, steroid-sparing agents). Diet should be maintained until the dose and frequency of all drugs are stable; diet can then be changed to determine if disease is exacerbated.
CBC, serum chemistry profile, and urinalysis should be performed every 6 months in dogs receiving glucocorticoids for a prolonged period.


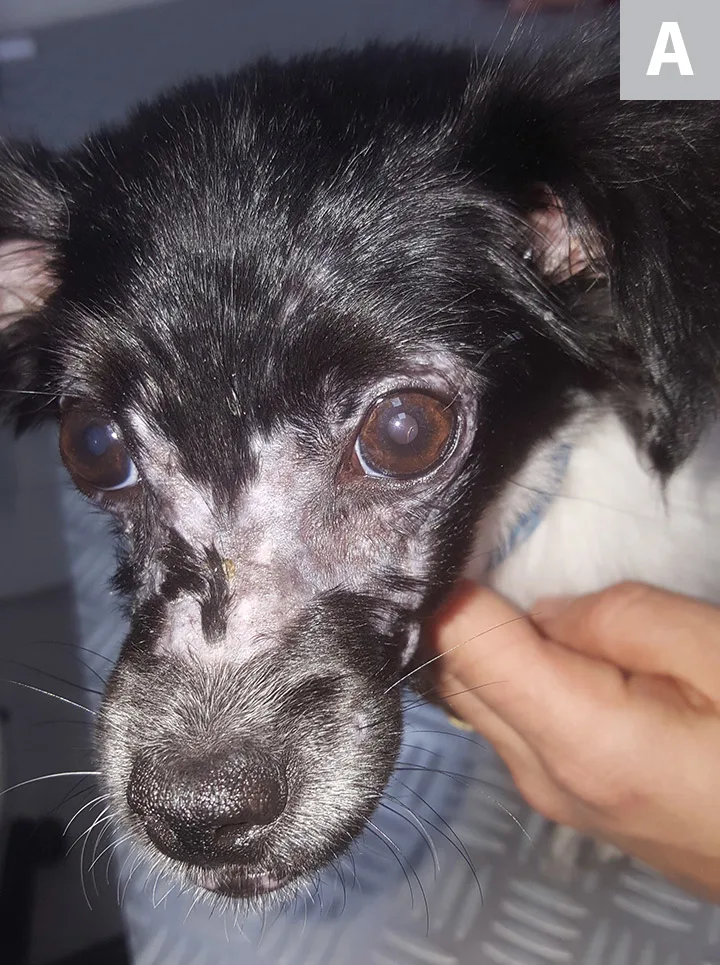
Dog with ischemic dermatopathy before (A) and 2 months after (B) treatment with oclacitinib. Images courtesy of Pablo Del Mestre
*Alpha-tocopherol may be referred to as D-alpha-tocopherol. This is not the same as DL-alpha-tocopherol, which is less effectively absorbed in humans.
Editor's note: This article was originally published in November 2021 as "Ischemic Dermatopathy in Dogs"