Intestinal Incision Dehiscence
Sabrina L. Barry, DVM, DACVS (Small Animal), Virginia-Maryland College of Veterinary Medicine
You Have Asked...
How can I prevent intestinal dehiscence from occurring after my GI surgeries?
The Expert Says...
The overall rate of dehiscence of full-thickness intestinal incisions in dogs is reported to be between 12% and 16%.1-4 This risk is substantially higher in patients that have a pre-existing septic abdomen (eg, from a perforating foreign body, an earlier intestinal surgery failure).1-4 More than one-third of patients experience dehiscence after repairs of an intestinal incision breakdown.1-4 Other pre- or intraoperative factors that should alert a practitioner to an increased dehiscence risk include intraoperative hypotension, hypoalbuminemia, intestinal foreign body, and a trauma patient. 1-2,4 Surprisingly, GI neoplasia has not yet been shown to increase the risk of GI incision dehiscence in veterinary studies.1,5
The healing process of any incision involves a period when tissues break down and lose strength before they become stronger. Briefly stated, this happens because the inflammatory processes of healing characterized by edema, neutrophil recruitment, and increased local collagenase activity begin before the repair processes of healing characterized by fibroblast recruitment and new collagen production. In the first few days of healing when the inflammatory phase predominates, the up-regulation of collagenase activity causes a tremendous loss of structural integrity as collagen is broken down at the incisional edges.
The healing process of any incision involves a period when tissues break down and lose strength before they become stronger.
During this period, the incision relies on the sutures and their ability to engage the remaining tissue. In healing rat intestinal anastomoses, the breaking strength of the sutured anastomotic sites (ie, the suture pull-out strength) decreased by 70% 24 hours after surgery.6 This initial decrease in tissue strength reverses as the repair phase initiates and new collagen is produced by fibroblasts and smooth muscle cells, leading to the characteristic quick healing of healthy small intestine, which typically reaches 75% of its initial tissue strength by 2 weeks after surgery. However, the vulnerable, initial period of relative collagenolysis, sometimes referred to as the lag phase of intestinal healing, can be intensified or prolonged by anything that causes persistent inflammation (eg, necrosis from lack of blood supply) or inhibits the production of collagen (eg, low oxygen tension). The ability of a clinician to influence the outcome of a healing GI incision has been succinctly described as “… our ability to manipulate the early struggle between collagen synthesis and collagen breakdown.”7 What follows are specific suggestions that surgeons can keep in mind to tip the balance toward collagen synthesis and to promote an early watertight seal that maintains its integrity through the lag phase of healing.
Related Article: Hypovolemic Shock
Support Tissue Oxygen Delivery to the Gut
The importance of perioperative supportive care to optimize intestinal perfusion and blood oxygen carrying capacity cannot be overemphasized: “Under normal conditions the rate limiting factor in collagen biosynthesis is the local availability of molecular oxygen.”8 The body compensates for early hypovolemia by routing blood away from the GI tract in favor of perfusion to more vital organs (eg, kidney, heart, brain). Most patients undergoing GI surgery have hydration and electrolyte disturbances, and a severely dehydrated patient with impending hypovolemia may have compromised GI blood flow even before signs of decreased perfusion are detectable elsewhere in the body. Replacing a substantial part of the patient’s fluid deficit before surgery and continuing to replace fluid deficit and losses after surgery is of utmost importance. In a study of rats undergoing resection and anastomosis, supplementing with more inspired oxygen during surgery lessened the risk of GI dehiscence by increasing oxygen delivery to the tissues.9 Interestingly, anemia does not seem to increase GI dehiscence rates unless it is severe (<15%).8
When possible, the segment of bowel to be incised can be moved out of the abdomen and away from the abdominal incision.
Minimize Contamination
Any full-thickness intestinal incision inevitably contaminates the surgery site with intraluminal microorganisms. Taking steps to keep this contamination to a minimum is an important principle of intestinal surgery. It is good practice to set aside instruments to be used for the contaminated portion of the procedure and keep them separate from clean instruments. When possible, the segment of bowel to be incised can be moved out of the abdomen and away from the abdominal incision. Carefully packing off the segment of intestines with laparotomy sponges before creating the enterotomy helps to isolate any spillage that may occur. Before the enterotomy, intestinal contents should be milked orad and aborad from the planned incision site and held out of the way with atraumatic (noncrushing) intestinal clamps or the fingers of a scrubbed-in assistant. Once the enterotomy is closed, the segment of intestine can be lavaged, and the contaminated laparotomy sponges removed before the intestine is replaced into the abdomen. Gloves and instruments should be changed before moving back to the clean portions of the surgery (eg, abdominal wall closure).
Be Mindful of Vascular Anatomy
The surgeon can help to ensure adequate blood supply to a healing intestinal incision by keeping in mind the jejunum’s vascular pattern (Figures 1-3). Twelve to 15 jejunal arteries arise from the cranial mesenteric artery and anastomose in arcades near the intestine. From these terminal arcades the short vasa recti bring blood directly to the intestinal wall on the mesenteric side. When planning a resection and anastomosis, the jejunal transection sites should be planned so that each remaining free edge is near a supplying jejunal artery, and the arcuate artery within the mesentery should be preserved up to the planned transection site (Figure 2). It is also important to avoid inadvertently ligating the supplying jejunal artery when suturing the mesenteric defect after the anastomosis is complete. If the surgeon chooses to transect the jejunum at an angle to correct for size disparity, recall that blood enters the jejunum on the mesenteric side and transect at an angle that leaves more mesenteric side with the body (Figure 3).

When performing an enterotomy to remove a foreign body, the enterotomy incision should be made on the aborad side of the foreign body whenever possible. This ensures that uncompromised tissue is sutured rather than the compromised tissue on the orad side. If needed, the aborad incision can be extended over the foreign body as much as necessary to remove the material.

For a resection and anastomosis, the jejunal transection sites should be planned so that each remaining free edge is near a supplying jejunal artery. This sometimes means taking more jejunum than one otherwise would.

When transecting jejunum at an angle to correct for luminal size disparity, transect at the angle that takes into account the blood supply.
Minimize Inflammation & Ensure Vascular Wound Edges
Some inflammation is a normal part of healing, but anything that prolongs or intensifies the inflammatory phase of wound healing causes a corresponding increase in collagenase activity. In general, abiding by Halsted’s principles of gentle tissue handling (see Halsted’s Principles), good apposition, and aseptic technique are of paramount importance in GI surgery. When handling intestines, the surgeon should avoid gripping the wall with thumb forceps and use atraumatic manipulation methods (eg, stay sutures) whenever possible. Crushing sutures are no longer recommended when closing GI incisions because they cause foci of necrosis in the postoperative period.11 Sutures should be pulled just tight enough to create a seal. Catgut suture has also fallen out of favor because its primary mechanism of dissolution is inflammation. Many other suture types are appropriate for intestinal incisions. The author prefers absorbable monofilament suture (eg, 4-0 polydioxanone) for most small animal intestinal surgeries.
Related Article: The Case: Pug With a GI Foreign Body
Halsted’s Principles10
Strict aseptic technique
Gentle tissue handling
Preservation of blood supply
Meticulous hemostasis
Elimination of dead space
Accurate tissue apposition
Engage the Submucosa During Suturing
During the lag phase, an incision’s mechanical strength comes primarily from the sutures, so it is imperative that sutures continue to engage the strength-holding part of the wall, the submucosa, throughout this phase. Although the thicker muscular layer of the intestine gives the surgeon strong tactile feedback during surgery, it is the submucosal layer that retains its integrity when the rest of the tissues at the wound edge lose their strength. As the mucosa naturally everts after it is incised, it hides the incision edge, so it is possible to accidentally incorporate a large amount of mucosa without including a substantial bite of submucosa. The result of this mistake is early loss of integrity of the repair.
Approximate the Submucosal Edges
Most of the early watertight seal of a GI repair is attributable to fibrin deposition between the edges of the incision, and early division and migration of enterocytes to meet one another across the mucosal defect. These processes work best when the edges are apposed, and approximating patterns (rather than inverting or everting patterns) are recommended for primary intestinal wound healing.12 Although hand-sutured anastomoses often have some degree of microscopic eversion despite attempted apposition13 and yet go on to heal uneventfully, purposefully interposing mucosa between the wound edges results in foci of mucosal necrosis and a prolonged inflammatory response.7 Biomechanically, everted closures have lower bursting strength during the lag phase of healing, suggesting an increased tendency to leak during this phase.7
Minimize the Number of Enterotomies
Each additional intestinal incision adds another potential source of intestinal leakage and prolongs surgery time. In the case of a single nonlinear foreign body, assess whether the foreign body can be milked into the stomach for removal via gastrotomy. Although often not possible because of the foreign body’s shape or because of poor wall viability, when the foreign body can be milked into the stomach, the enterotomy is avoided. For linear foreign bodies anchored in the pylorus, a gastrotomy is usually required. Once the gastric anchor is released, this author’s experience is that it is rarely necessary to perform more than one enterotomy to remove the rest of the foreign body.
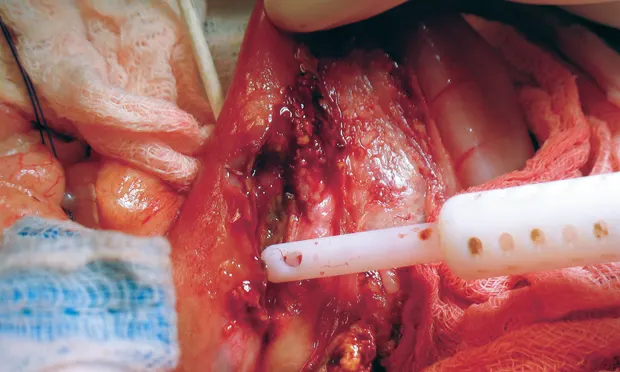
Particularly challenging cases are those with very thin, thread-like linear foreign material.In these cases, a technique using a red rubber catheter can be particularly helpful to remove the entire length of foreign material through one enterotomy. In this technique, a red rubber catheter is tied to the foreign body in the stomach and then passed through the pylorus and milked aborad through the intestine. As the catheter is advanced, the foreign material releases from the wall of the intestine and folds onto itself until it is safe to remove through a single incision. A similar technique has been described in which the red rubber catheter, along with the foreign material, is milked all the way out of the anus to avoid enterotomy completely.14
Related Article: Feline Intestinal Foreign Bodies
Preserve the Omentum
The omentum has an impressive ability to support viscera with fast adhesion formation and neovascularization. The omentum protects and supports the early fibrin seal and the overall healing environment. Although the healthy omentum can be expected to cover the GI repair site on its own, surgeons often tack the omentum to the seromuscular layer with interrupted sutures around the repair before closing the abdomen, which is meant to take full advantage of the healing properties of this unique tissue. In experimental dogs in which a segment of ischemic intestine was transected and reanastomosed, wrapping the anastomosis site with omentum prevented the dehiscence and peritonitis that developed in the unomentalized dogs.15
There is overwhelming evidence that withholding food is more detrimental to intestinal healing than early feeding.
Offer Early Enteral Nutrition
Withholding food after GI surgery makes intuitive sense, and food withholding was the standard of care in human and veterinary surgery for many years. There is overwhelming evidence that withholding food is more detrimental to intestinal healing than early feeding.16 Small molecules (eg, short-chain fatty acids, glutamine) are the key nutrients for enterocytes, and their presence in the intestinal lumen stimulates enterocyte proliferation. Early enteral feeding leads to higher intestinal bursting pressure after anastomosis in experimental dogs17 and less clinical dehiscence, lower mortality, shorter hospital stays, and fewer postoperative infections in human clinical trials.16 This author’s practice is to offer a small meal of highly digestible food when the patient is fully recovered from anesthesia. Consider placing a feeding tube at the time of surgery if the patient has experienced extensive weight loss or if the patient is expected to not eat within the first few days of surgery.
Related Article: Nutritional Support for Critically Ill Dogs & Cats
Conclusion
Unlike skin incisions, GI incisions cannot be seen during the vulnerable postoperative healing period. This makes it hard for a surgeon to know what factors, if any, could have been changed to prevent cases of septic abdomen when they occur. The GI healing process is important for the clinician to keep in mind before, during, and after surgery to best guide therapy to minimize the risk of intestinal incision dehiscence.