Interpreting ECGs with Confidence: Part 2
Barret Bulmer, DVM, MS, DACVIM (Cardiology), Cummings School of Veterinary Medicine at Tufts University
This is the second installment of a two-part series outlining ECG interpretation. Part 1 discusses the general steps for ECG assessment and common rhythms associated with normal heart rates.
What are the most common tachyarrhythmias?
The most common sustained tachyarrhythmias include atrial fibrillation (AF), ventricular tachycardia (VT), sinus tachycardia, and supraventricular tachycardia (SVT).
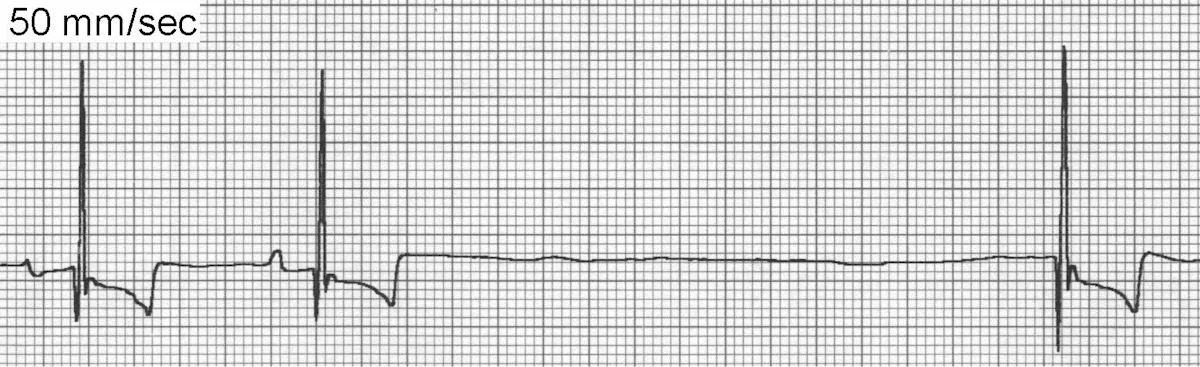
Atrial Fibrillation
AF (Figure 1) is the classic irregularly irregular, fast cardiac rhythm produced by disorganized and chaotic depolarization of atrial myocardial tissue, resulting in the inability to produce effective atrial contractions. AF is one of the most important arrhythmias in dogs but is uncommon in cats. Most cases are secondary to severe atrial enlargement and underlying heart disease.
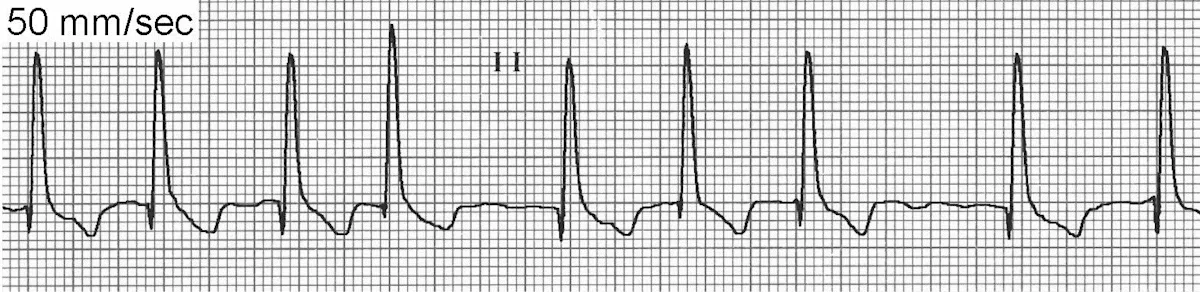
ECG of Atrial Fibrillation
Propagation of AF requires a critical amount of atrial mass and, in general, the larger the animal the easier it is to induce and maintain AF. Because of their size, giant-breed dogs can develop AF without other objective evidence of cardiac disease. Hallmark findings include an irregularly irregular rhythm with variation in heart sound intensity and arterial pulse quality.
The 3 ECG hallmarks of AF include absence of identifiable P waves in all leads, supraventricular QRS complexes, and an irregularly irregular rhythm. The baseline may frequently display oscillations but the organization is ill defined.
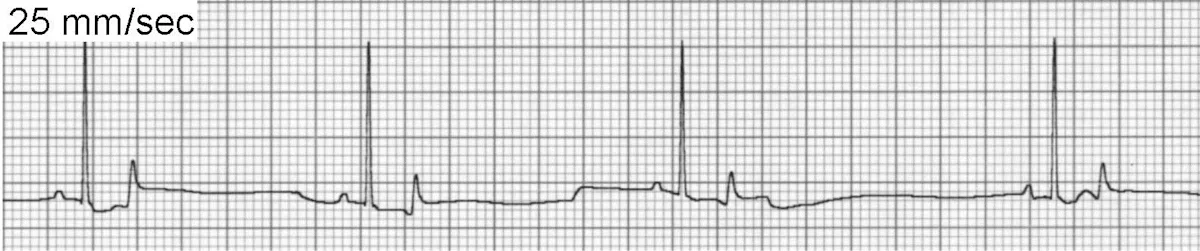
Ventricular Tachycardia
VT is defined as 3 or more ventricular premature complexes (VPCs) occurring in succession. VT produces wide and bizarre QRS complexes and displays a range of rate, morphology, and regularity; it is generally considered a serious and potentially life-threatening arrhythmia, especially in patients with underlying heart disease or clinical signs (weakness, collapse, shock). A variety of mechanisms can produce VT, including reentry, abnormal automaticity, and triggered activity. P waves may still be visible (Figure 2A) but there is no consistent temporal relationship with QRS complexes. SVT with abnormal ventricular conduction (eg, bundle branch block) can be confused with VT.
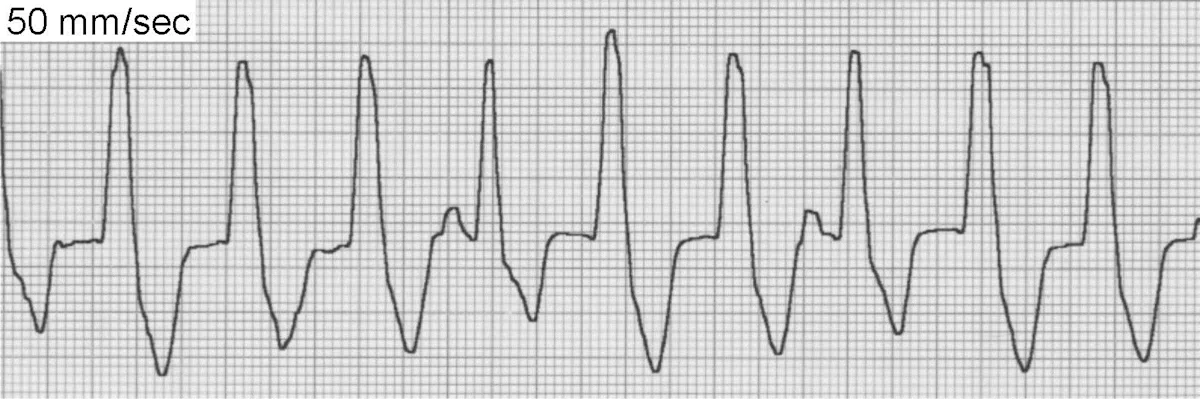
ECG of unifocal ventricular tachycardia
Unifocal VT is the most common type and (when sustained) produces a fast, regular cardiac rhythm.
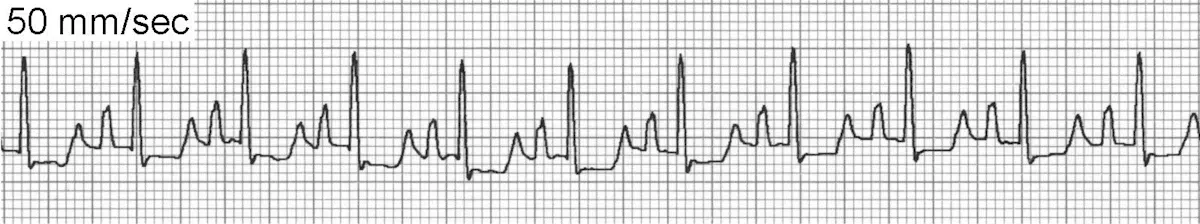
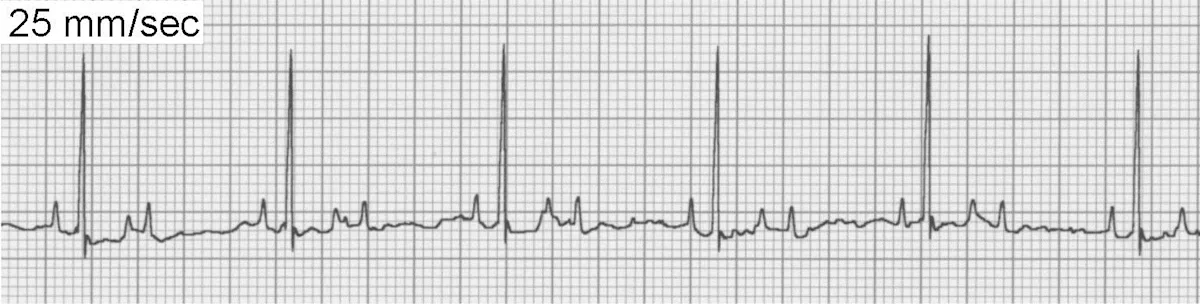
Paroxysmal VT (Figure 2B) may produce irregular bursts of tachycardia that interrupt an otherwise normal rhythm.
 FIGURE 2B
FIGURE 2BECG of paroxysmal ventricular tachycardia
Sinus Tachycardia
Sinus tachycardia (Figure 3) maintains all criteria for sinus rhythm except the heart rate is above normal. The most common cause of sinus tachycardia is high sympathetic tone, usually associated with excitement or stress during examination. Other causes include fever, pain, hyperthyroidism, anemia, shock, heart failure, and treatment with sympathomimetic agents such as bronchodilators or catecholamines.
ECG of sinus tachycardia
The underlying mechanism of sinus tachycardia is enhanced normal automaticity of the sinoatrial (SA) node. In general, there are P waves for every QRS complex and the PR interval is consistent. However, at faster rates the P waves may become superimposed on the preceding T wave and the rate may be fast enough to cause intermittent atrioventricular (AV) block. The heart rate may gradually slow during a vagal maneuver, ultimately allowing identification of P waves.
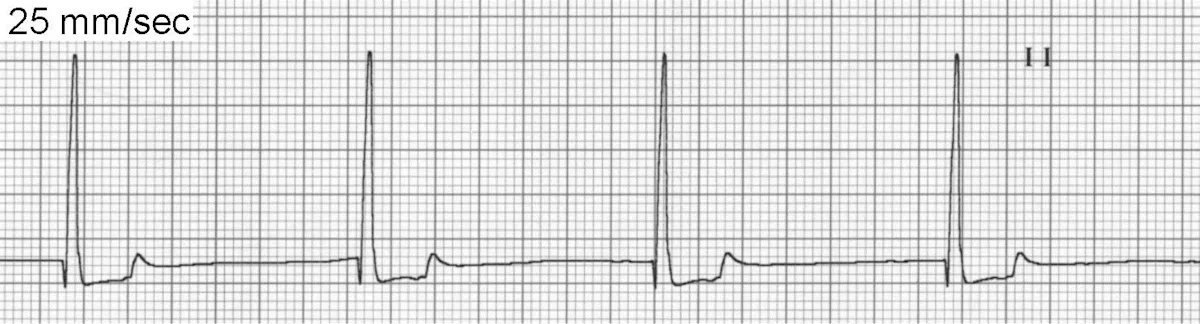
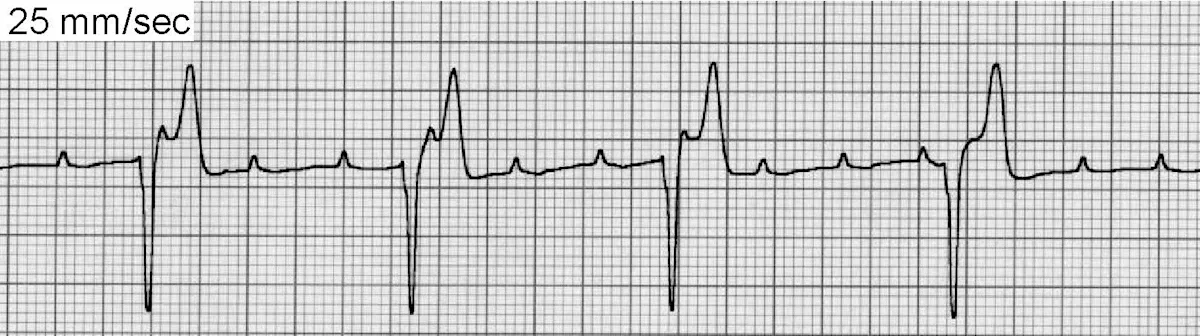
Supraventricular Tachycardia
SVT (atrial or junctional) may lack easily identifiable P waves or have P waves with slightly different morphology than normal sinus beats. Paroxysmal SVT often displays abrupt onset and termination. AF is a specific form of SVT, as previously discussed.
SVT (Figure 4) is an infrequent arrhythmia defined as 3 or more SV beats in succession. SVT is usually associated with significant heart disease and atrial enlargement. A unique form of SVT is associated with an accessory pathway connecting the atria and ventricles. When occurring as a paroxysm, the rhythm is fast and regular, often with abrupt onset and termination. The first heart sound is often accentuated while audible murmurs diminish in intensity during the paroxysm as a result of decreased stroke volume. SVT usually results from a reentry circuit, although it may also occur subsequent to enhanced normal or abnormal automaticity.
 FIGURE 4
FIGURE 4ECG of supraventricular tachycardia
Sustained SVT can provoke loss of normal myocardial contractility and eventual heart failure, while paroxysmal SVT can cause episodic weakness and syncope. Therapeutic interventions can be administered to acutely terminate SVT and prevent recurrence.
What are the most common bradyarrhythmias?
The most common bradyarrhythmias include atrial standstill, sinus arrest, sinus bradycardia, and various forms of AV block (second- or third-degree).
Atrial Standstill
Atrial standstill (Figure 5) is an uncommon arrhythmia caused by idiopathic destruction of atrial myocardium or severe hyperkalemia. The atrial myocardium becomes unresponsive to sinus impulses and does not depolarize. A junctional or ventricular escape rhythm takes over control of the ventricles. The prognosis in dogs with idiopathic disease is guarded, as many experience progressive myocardial disease and eventual heart failure. However, some dogs will live several years with pacemaker implantation and prevention of congestive heart failure.
ECG of atrial standstill
Sinus Arrest
If a P wave is not present for every QRS complex, sinus arrest (Figure 6) may be present. Some patients with sinus arrest may have sick sinus syndrome, which may be complicated with periods of AV block and/or SVT. Sinus arrest occurs when the SA node fails to depolarize because of deceased normal automaticity, resulting in a pause in the heart rhythm that can last from <1 second to many seconds. Longer periods of sinus arrest may be accompanied by signs of weakness or syncope.
ECG of sinus arrest
Historically, the criteria for sinus arrest involved a pause that lasted >2 R-R intervals; however, dogs with pronounced sinus arrhythmia can also display pauses of this duration, resulting in some overlap between the diagnoses. Possible causes of sinus arrest include excessive vagal tone, sick sinus syndrome, and hyperkalemia. In general, treatment is not required in asymptomatic patients.
Sinus Bradycardia
Sinus bradycardia (Figure 7) occurs when criteria for sinus rhythm are met but the heart rate is slower than normal. The exact rate at which sinus bradycardia is considered pathologic is subjective: 40 bpm in a sleeping dog is considered normal, but the same would be considered abnormal during examination. A common cause of sinus bradycardia is elevated vagal tone caused by athletic conditioning, increased intracranial pressure, severe GI or respiratory disease, or administration of parasympathomimetic or sympatholytic drugs. Other causes include sedative or anesthetic agents, hypothermia, hyperkalemia, sick sinus syndrome, and severe hypothyroidism.
ECG of sinus bradycardia
Second- & Third-Degree AV Block
Second-degree (Figure 8) and third-degree (Figure 9) AV block have some (second-degree) or all (third-degree) P waves blocked at the level of the AV node or His-Purkinje system. This alteration will produce P waves without an associated QRS complex.
ECG of second-degree AV block
ECG of third-degree AV block
Second-degree AV block occurs when a proportion of atrial impulses are prevented from reaching the ventricles. High-grade second-degree AV block is often secondary to idiopathic conduction system disease and may cause transient weakness, syncope, or sudden death. Other causes include high vagal tone, treatment with digoxin, calcium-channel blockers, β-blockers, or underlying heart disease or electrolyte abnormalities (uncommon).
Third-degree or complete AV block is present when none of the atrial impulses reach the ventricles, indicating complete AV dissociation. Instead, ventricular depolarization relies on subsidiary pacemaker cells that depolarize more slowly than the sinus node or AV node. Canine patients with third-degree AV block usually present with weakness, exercise intolerance, syncope, congestive heart failure, and/or dyspnea; some have experienced sudden death. Dogs reportedly may also be asymptomatic and the arrhythmia will be detected during routine or preoperative examination. AV block is often idiopathic, although other causes include degenerative, infiltrative, inflammatory, infectious, and/or immune-mediated heart disease; hyperkalemia or severe digoxin toxicity can also be a cause.
Cats with third-degree AV block rarely display clinical signs as a result of an adequate ectopic pacemaker rate to maintain cardiac output. Some cats with transient AV block will present with syncope. Atropine or oral sympathomimetics can be administered but are often ineffective.