Interpreting ECGs with Confidence: Part 1
Barret Bulmer, DVM, MS, DACVIM (Cardiology), Cummings School of Veterinary Medicine at Tufts University
How do I interpret ECGs with confidence?
Arrhythmias are clinically important because of their ability to compromise cardiac output and oxygen delivery to the body. The level of cardiac performance during an arrhythmia depends on rate, site of origin, and duration of the arrhythmia, as well as the presence of underlying cardiac or systemic diseases that may adversely affect the patient. Consequences of an arrhythmia may be clinically undetectable, produce signs of inadequate cardiac output (eg, weakness, fainting, shock), or lead to complete collapse of the circulatory system and sudden death.
The 4 general steps for ECG assessment include evaluation of heart rate, cardiac rhythm, mean electrical axis, and assessment for patterns of chamber enlargement. The following review assesses and interprets common canine and feline arrhythmias.
A systematic approach to interpreting ECGs will ensure an accurate diagnosis. The initial steps should include evaluating paper speed and sensitivity followed by labeling the individual waveforms recorded on the ECG. Afterward, the following questions should be addressed:
This is the first installment of a two-part series outlining ECG interpretation. Part 2 addresses bradyarrhythmias and tachyarrhythmias.
Is there a P wave for every QRS complex?
Atrial depolarization normally propagates through the AV node and subsequently produces depolarization of the ventricles, resulting in a fixed relationship of one P wave preceding every QRS complex.
Meanwhile, ectopic QRS complexes often originate without a preceding atrial event. Premature ectopic complexes occur <1 R-R interval from the preceding sinus beat, while escape complexes generally occur 1.5 to 2 R-R intervals from the preceding sinus beat.
Is there a QRS complex for every P wave?
After a brief delay (PR interval) ventricular depolarization normally follows every atrial depolarization, resulting in a QRS complex for every P wave. However, in some instances the electrical impulse may be blocked at the level of the AV node or His-Purkinje system, preventing propagation and subsequent depolarization of the ventricles.
Are P waves associated with QRS complexes?
Normally there is a fixed or nearly fixed physiologic PR interval between the P waves and QRS complexes, but in some instances there appear to be P waves that contribute to generating ventricular depolarization while they are instead merely fortuitous and QRS complexes are unrelated to the preceding atrial activity.
Are the QRS complexes supraventricular or ventricular?
If the electrical impulse originates from the sinus node, atrial myocardium, or atrioventricular (AV) node, the QRS complex will generally be tall, upright, and narrow (ie, supraventricular [SV]) because it utilizes the normal His-Purkinje system. Circumstances in which the QRS complex is SV but appears abnormal include ventricular enlargement patterns or bundle branch blocks.
If the electrical impulse originates from the ventricular myocardium, the QRS complex will be wide and bizarre (ie, ventricular) because it does not utilize the normal His-Purkinje system.
What is the underlying rhythm of P waves & QRS complexes?
A regular rhythm generally has <10% variation in the R-R intervals, while a regularly irregular rhythm has QRS complexes that vary by >10% but there is a repeating pattern to rate variation. An irregularly irregular rhythm is chaotic, usually fast, and without pattern to the irregular nature.
A paroxysmal rhythm disturbance is usually characterized by a sudden outburst of arrhythmia that may last for as short as 3 to 4 beats or as long as minutes to hours.
What are the most common rhythms with normal heart rates?
The most common cardiac rhythms that occur while the heart rate is normal include sinus rhythm, sinus arrhythmia, SV premature complexes, ventricular premature complexes (VPCs), or accelerated idioventricular rhythm. Sinus rhythm, sinus arrhythmia, and SV premature complexes tend to have tall, upright, narrow QRS complexes. Sinus rhythm with VPCs or accelerated idioventricular rhythm may have a normal heart rate with intermittent or sustained ventricular morphology QRS complexes; because these impulses originate from the ventricular myocardium, they are conducted aberrantly and have abnormal morphology.
Requirements for Success
Obtaining accurate ECG diagnosis
Considering possible underlying mechanism or cause of arrhythmia
Determining presence of underlying heart disease
Understanding the goals of arrhythmia treatment:
In patients with clinical signs: Reducing hemodynamic compromise caused by arrhythmia and preventing death
In asymptomatic patients: Preventing arrhythmia from progressing to cause clinical signs or death
Sinus Rhythm & Cardiac Arrhythmia
Sinus rhythm represents the normal sequence of cardiac electrical activity. Pacemaker cells within the sinoatrial node display automaticity and serve as the origin for the normal cardiac impulse. The P wave is recorded on the ECG as the wave of electrical activity depolarizes the atrial myocardium. The electrical impulse then traverses the AV node and His-Purkinje system, recorded as the PR interval, followed by depolarization of the ventricular myocardium producing the QRS complex. The T wave is recorded during ventricular repolarization (Figure 1). The average heart rate (ie, ventricular heart rate) can be determined on an ECG strip recorded at 50 mm/sec by counting the number of QRS complexes in 15 large boxes (75 mm) and multiplying by 40.

P wave (P), QRS complex (QRS), and T wave (T). In this ECG, the average heart rate would be 120 bpm. If the ECG strip is recorded at 25 mm/sec, the number of QRS complexes can still be counted in 15 large boxes (75 mm) but must be multiplied by 20 to determine the bpm.
Sinus Rhythm
Sinus rhythm (Figure 2) maintains a regular underlying rhythm with P waves present for every QRS complex, QRS complexes present for every P wave, a relatively fixed PR interval, and SV QRS complexes. Sinus rhythm is normal for dogs and cats.
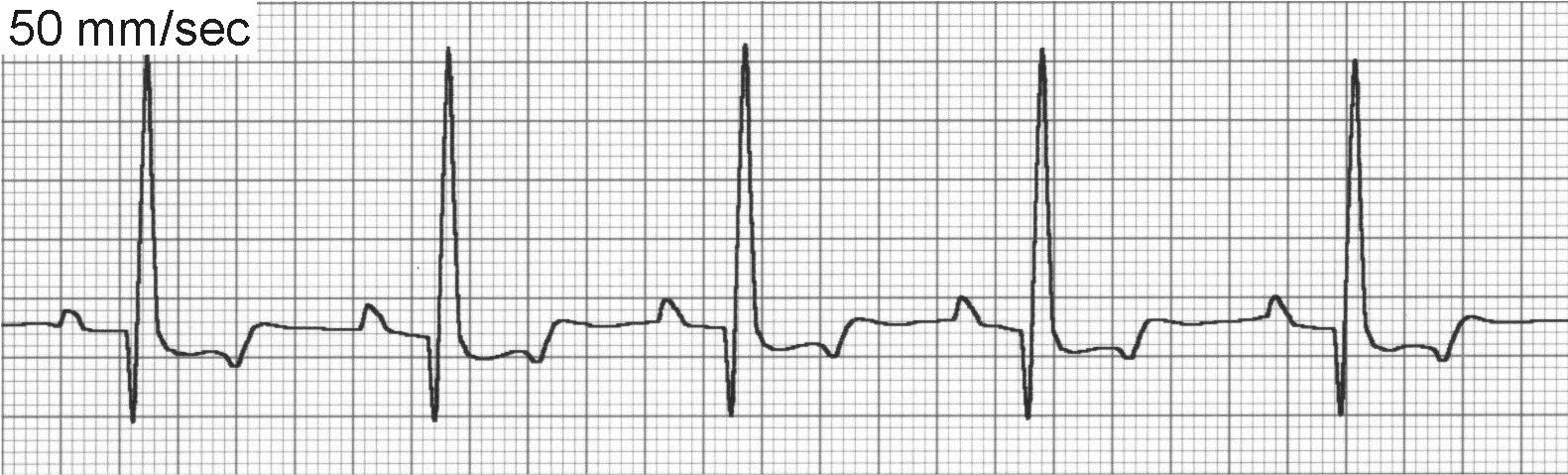
ECG of sinus rhythm
Sinus Arrhythmia
Sinus arrhythmia (Figure 3) is a phasic variation in heart rate in which R-R intervals often vary by >10%. There continues to be a P wave for every QRS complex and a QRS complex for every P wave, although on occasion the P wave morphology will vary or be difficult to visualize because of a phenomenon called wandering pacemaker (Figure 3B).

ECG of sinus arrhythmia
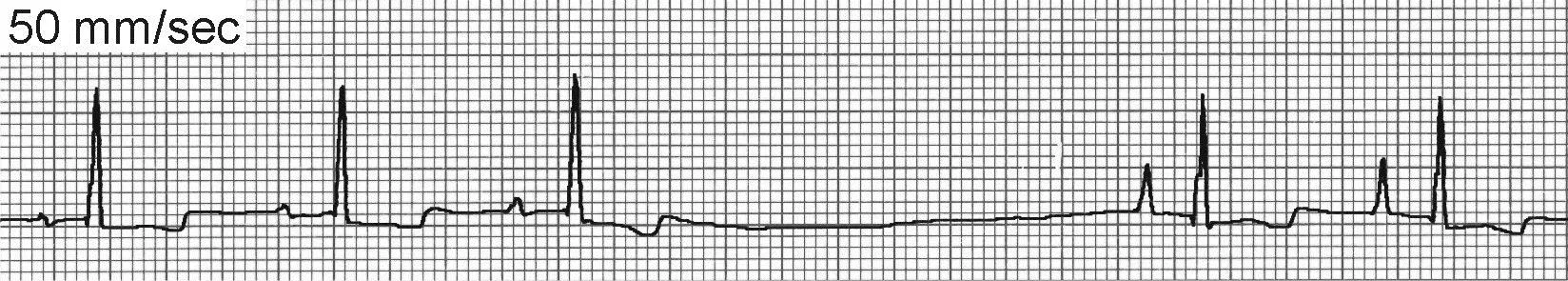
ECG of the wandering pacemaker phenomenon
Sinus arrhythmia is usually respiratory with the heart rate increasing in late inspiration and early expiration and decreasing in mid to late expiration. However, any other cause of increased vagal tone may also contribute to sinus arrhythmia even in the absence of respiratory variation. The underlying mechanism of sinus arrhythmia is depressed normal automaticity of the SA node.
Sinus arrhythmia is most common in normal resting dogs but uncommon in cats. Treatment is not required.
Accelerated Idioventricular Rhythm
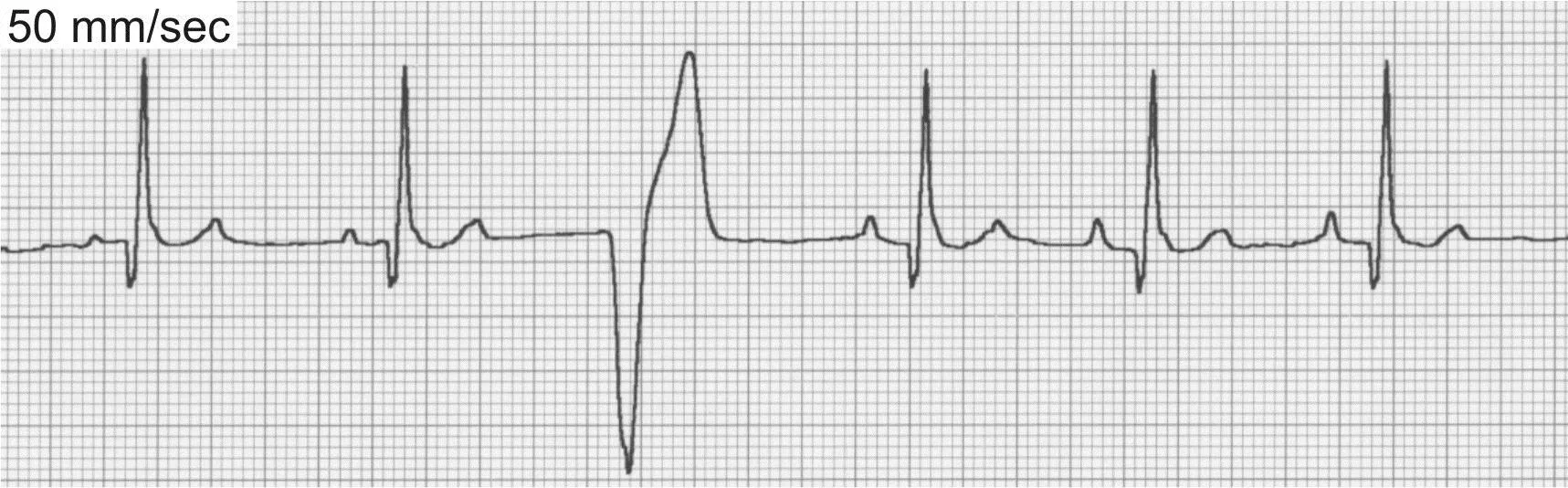
Also known as slow ventricular tachycardia (Figure 4), this is a unique form of ventricular tachycardia typified by slow heart rates (dogs, 70–150 bpm). The rate of the accelerated idioventricular rhythm is usually within 10 to 15 beats of the normal sinus rate, and control of the heart rhythm alternates between the two sites. Because the rate of the idioventricular focus is slow, there is little hemodynamic consequence and patients generally remain asymptomatic. These rhythms are commonly seen with noncardiac disease and also in dogs with traumatic myocarditis and neurologic disease. Specific treatment of an accelerated idioventricular rhythm is rarely indicated and should be directed toward underlying causes.

ECG of accelerated idioventricular rhythm, or slow ventricular tachycardia
Ventricular Premature Complexes
VPCs (Figure 5) can be associated with significant inflammatory, structural, toxic, infiltrative, traumatic, or ischemic heart disease. VPCs are also common in patients with noncardiac disease (eg, gastric dilatation-volvulus [GDV], splenic disease/surgery, hyperthyroidism, sepsis, anemia, hypoxia, myocarditis/infectious disease, coagulopathies). Patients with elevated sympathetic tone from extreme excitement or pain may also display VPCs, as well as drug therapy with digoxin, anesthetics (especially short-acting thiobarbiturates), and catecholamines.
ECG of ventricular premature complexes
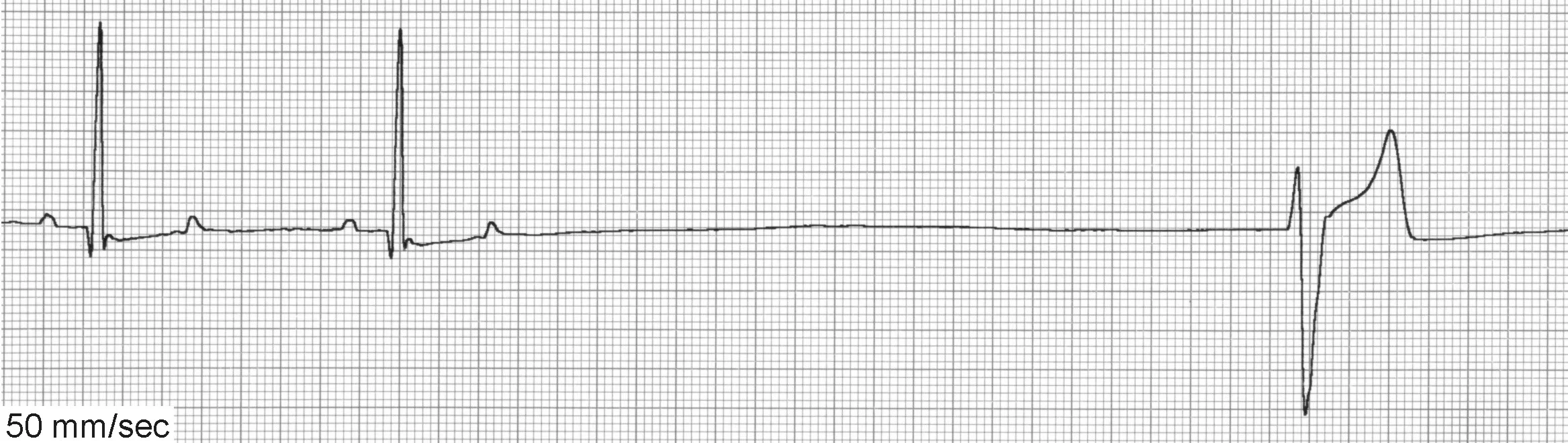
ECG of ventricular escape beats
VPCs generally occur <1 R-R interval from the preceding sinus beat (vs ventricular escape beats [Figure 5B] that generally occur >2 R-R intervals from the preceding sinus beat) and are not associated with preceding P waves. Care must be taken to exclude these arrhythmias from sinus rhythm with chamber enlargement patterns or sinus rhythm with conduction disturbances.
The decision to treat VPCs can be difficult. Frequent and multiform VPCs in the presence of underlying heart disease, especially with clinical signs, will necessitate treatment. Infrequent, uniform VPCs without clinical signs or heart disease uncommonly require treatment. Treatment for VPCs secondary to underlying metabolic disease is usually not indicated and therapy should instead be aimed at correcting the underlying condition.
Supraventricular Premature Complexes
Underlying sinus rhythm with SV premature complexes will have QRS complexes that occur early (<1 R-R interval from the preceding sinus beat), maintain an SV morphology, and either lack P waves (junctional) or have P waves with aberrant morphology (atrial). SV premature complexes can be difficult to distinguish from sinus arrhythmia with a wandering pacemaker, although the former usually occurs at an instantaneous rate suggestive of tachycardia. The instantaneous rate is determined by counting the number of millimeters between 2 successive QRS complexes, and if recorded at 50 mm/sec, dividing that number into 3000.
SV premature complexes (Figure 6) are often produced subsequent to atrial enlargement associated with underlying myocardial, valvular, or congenital heart disease. SV premature complexes are occasionally seen in patients without clinical evidence of cardiac disease. The presence of these beats may precede development of further atrial arrhythmias, including SV tachycardia (SVT), atrial flutter, or atrial fibrillation.
 FIGURE 6
FIGURE 6ECG of supraventricular premature complexes
In most cases, SV premature complexes are infrequent, do not cause clinical signs, and do not require treatment. In patients with paroxysms of SVT, treatment with digitalis, calcium-channel blockers, or β-blockers may be instituted. Treatment for underlying heart disease may also be necessary.