Infectious Diseases of the Nasal Cavity

An 8-year-old, spayed female Siberian husky presented for epistaxis and mucopurulent nasal discharge.
History. The first episode of epistaxis had occurred 3 weeks before presentation and resolved after several hours. The second episode happened the following week and was more severe, prompting veterinary attention. Bleeding occurred from the right nostril only. Diagnostic investigation included complete blood count, measurement of prothrombin and partial thromboplastin times, measurement of Ehrlichia canis titers, and nasal radiographs. No significant abnormalities were identified. Mucopurulent nasal discharge was first observed after the second episode of epistaxis, which initially occurred from the right nostril only but became bilateral within days. The third episode of severe epistaxis prompted referral. Other than the nasal signs, the dog had been in good health.
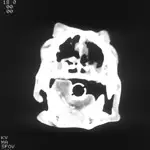
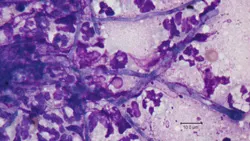
Physical Examination. Abnormalities were limited to the dog's head. Bilateral mucopurulent nasal discharge was observed, with intermittent epistaxis from the right nostril. After removal of crusty debris, airflow was apparent from both nares. Depigmentation of the nasal planum was observed. Although there was moderate dental tartar, obvious periodontal disease was absent. Diagnostic investigation included CT (Figure 1) and rhinoscopy (Figure 2) with cytologic evaluation (Figure 3), biopsy, and fungal culture.
_
Figure 3. Wright-Giemsa stain; original magnification, 100×; image courtesy of Dr. Linda Berent, University of Missouri.
_
Ask Yourself ...
What are the likely causes of mucopurulent nasal discharge with nasal hemorrhage in the dog?
What advantages over nasal radiographs are offered by CT of the nasal passages?
Diagnosis: Fungal rhinitis
The primary differential diagnoses included nasal neoplasia and aspergillosis. No contrast-enhancing mass was seen on nasal CT, but areas of osteolysis were observed in both nasal passages and increased soft tissue opacity was seen in both frontal sinuses. The cribriform plate was intact. Rhinoscopy revealed large, irregular white plaques in both nasal passages, nasal turbinate destruction, and hemorrhage. Cytologic evaluation of a plaque confirmed fungal infection. Aspergillus fumigatus was identified both histologically and through culture.
Aspergillus fumigatus is the most common cause of fungal rhinitis in dogs. The diagnosis can sometimes be suggested by noninvasive tests, including cytologic impression of nasal discharge or nasal swab to identify fungal elements or by serologic titers. However, sensitivity of either technique is inadequate to rule out fungal rhinitis and specificity is also low, as these tests do not confirm that fungal elements identified are actually the cause of the animal's signs.
The treatment of choice for A. fumigatus if the cribriform plate is intact is topical infusion of clotrimazole via nasal catheters. In this dog, clotrimazole infusion was followed by overnight observation. The dog had severe bilateral mucopurulent nasal discharge, slight epistaxis, and melena (probably resulting from swallowed blood), but the amount of discharge and epistaxis gradually lessened over the next several days. Although success rates of 80% to 90% are reported for topical clotrimazole treatment, second and even third treatments may be required for some dogs. For this dog, a single infusion was adequate to eliminate fungal disease. However, permanent destruction of nasal turbinates, as occurred in this dog, removes an important physical defense mechanism, therefore predisposing to secondary bacterial rhinitis. This dog required occasional courses of antibiotic therapy when mucoid or mucopurulent nasal discharge developed but had no further episodes of epistaxis.
Figure 1. Noncontrast-enhancing soft tissue densities compatible with mucus and/or blood accumulation are visible in the ventral nasal passages and frontal sinuses and were confirmed by evaluating Hounsfield values. The dog also had loss of nasal turbinates in the central nasal passages, confirmed by viewing the images with an expanded gray scale (lung window not shown). Such lung windows allow all soft tissues to be uniformly gray so that thin structures, such as turbinates, can be evaluated. (They are usually not visible in high-contrast soft tissue windows.)

Figure 2. The white area represents fungal plaque, a finding essentially pathognomonic for fungal rhinitis.
Figure 3. Fungal hyphae of Aspergillus fumigatus are microscopically visible among inflammatory cells.
Did You Answer ...
The most likely causes of mucopurulent nasal discharge with nasal hemorrhage in dogs are nasal neoplasia (often adenocarcinoma) and fungal rhinitis. Nasal foreign body and periodontal disease are also reasonable differential diagnoses but are unlikely to cause bilateral discharge.
Nasal radiographs and nasal CT can both identify bone lysis, nasal cavity distortion, nasal mass effect, and radiopaque foreign bodies. However, CT offers important advantages over plain nasal radiographs because it can assess the integrity of the cribriform plate and plain radiographs cannot. Intravenous iodinated contrast administration during CT may allow differentiation of vascularized tissue (mass) from mucus or hemorrhage. Brain contrast enhancement, if present, may indicate tumor invasion through the cribriform plate. Compared with radiographs, CT offers spatial information as well as the ability to reformat acquired axial images into sagittal and dorsal plane images, which facilitates biopsy sample collection and allows for radiation planning if nasal carcinoma is diagnosed.
TX at a glance
Topical intranasal instillation of clotrimazole (or enilconazole) is indicated only if the cribriform plate is intact.
Prior debridement of fungal plaque lesions may improve therapeutic outcome of topical therapy.
When the cribriform plate is breeched, prolonged oral therapy with itraconazole is indicated.
Systemic antifungal therapy (e.g., itraconazole) is also indicated if soft tissues outside the nasal passages or sinuses are infected.